Translate this page into:
Role of Magnetic Resonance Cholangiopancreatography in Cases of Obstructive Jaundice in Correlation with Ultrasonography
Corresponding Author: Mohammadali S Jiwani, Resident, Department of Radiodiagnosis, Datta Meghe Institute of Medical Sciences, Wardha, Maharashtra, India, Phone: +917038949616 e-mail: dr.ali.jiawni@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
How to cite this article: Jiwani MS, Banode PJ, Kharche AD, Jiwani A A, Vaidhya SV. Role of Magnetic Resonance Cholangiopancreatography in Cases of Obstructive Jaundice in Correlation with Ultrasonography. Int J Recent Surg Med Sci 2016;2(2):70-84.
Abstract
Jaundice is a common problem in society, it is important to discriminate between obstructive and non obstructive cause due to high morbidity in cases of obstructive jaundice, also non obstructive jaundice requires medical management while obstructive jaundice requires surgical intervention. Our study was done with aims to determine role of MRCP in cases of obstructive jaundice in correlation with ultrasonography keeping post surgical follow ups/ ERCP/ histopathology as gold standard for final diagnosis. All patients in our study undergone USG followed by MRCP. We had included total 100 patients out of which 58 females and 42 males. Out of all patients we have observed 56 malignant causes and 44 benign causes. We have observed benign conditions are seen more frequently in adults while increase in frequency of malignancy with increase in age thus there found to have direct relationship of malignant etiology with increase in age. Most common benign cause observed in our study was choledocholithiasis while most common malignancy was carcinoma head of pancreas. In our study we have concluded that MRCP is better modality with high sensitivity, specificity and diagnostic accuracy as compared to USG also with use of MRCP invasive procedures like ERCP can be avoided just for diagnostic purpose. We have also noticed few limitations of both USG and MRCP in process of diagnosis.
Keywords
Jaundice
Magnetic resonance cholangiopancreatography
Obstructive jaundice
Ultrasonography.
INTRODUCTION
The word “jaundice” comes from the French word JAUNE, which means yellow. Jaundice is a yellowish discoloration of the skin, sclera, and mucous membranes by bilirubin, a yellow orange bile pigment.1 It is broadly divided into obstructive (surgical) and nonobstructive (medical) types of jaundice.2 Jaundice is one of the most common causes of morbidity in society. It is important to discriminate between obstructive from nonobstructive type because nonobstructive jaundice requires medical management, while obstructive jaundice requires surgical intervention.
Obstructive jaundice is a challenging condition to the surgeon because of its high morbidity and mortality. Ill-chosen procedure for management may increase further load of morbidity to the disease, thus preoperative evaluation of disease is important to know the cause of obstruction, nature of lesion, and extent and level of involvement.3,4
The great advances in the last few decades have made us know better about the pathophysiology, diagnosis, staging, and efficacy of management. With increase in the therapeutic option the role of a radiologist has also been increased and made necessary rather than simply differentiating obstructive from nonobstructive jaundice, as a surgeon can choose better plan of management by knowing the etiology, location, level, and extent of disease like biliary enteric anastomosis.5,6
Various invasive and noninvasive modalities are available for investigation of obstructive jaundice. Noninvasive modalities are ultrasonography (USG), computed tomography (CT), and magnetic resonance cholangiopancreatography (MRCP), while invasive modality includes endoscopic retrograde cholangiopancreatography (ERCP). Ultrasonography has always been chosen as the primary modality of screening by physicians while CT and MRCP are seen as diagnostic modality. With evolution of better sequences by Wallener et al in 1991, MRCP has played a major role as noninvasive radiation-free modality of choice for diagnosis. Endoscopic retrograde cholangiopancreatography has advantage of both diagnostic and therapeutic potential, while it has the disadvantage of having complications like cholangitis, biliary leakage, pancreatitis, bleeding, and incomplete opacification in 30 to 40% of cases.7-9
AIMS AND OBJECTIVES
This is a prospective study to determine the role of MRCP in cases of obstructive jaundice in correlation with USG taking postsurgical follow-ups/ERCP/histopathology as gold standard.
MATERIALS AND METHODS
The approval for the study was obtained from the ethical committee of our institution. Consent was taken from all patients undergoing USG and MRCP. We prospectively studied 100 patients (58 females and 42 males) in the age 12 to 80 years over the period from July 2014 to August 2016 at Acharya Vinoba Bhave Rural Hospital attached to Jawaharlal Nehru Medical College, Sawangi (Meghe), Wardha. Initial USG evaluation was followed by magnetic resonance imaging (MRI)/MRCP. Ultrasonography was performed with Aloka (prosound 7 alpha) and MRI/MRCP with 1.5 T 4E (model: BRIVO MR355). Magnetic resonance cholangiopancreatography was done in all patients using our standard MRCP protocol.
All patients clinically suspected as having obstructive jaundice were included in our study.
All patients with clinical features of biliary obstructive disease were included in the study. Following patients were excluded:
Patients not giving consent
Patients with contraindications to MRI
Patients with prehepatic/hepatic jaundice.
RESULTS
We have included a total of 100 patients in our study, out of which 42 were males and 58 were females, all subjected to USG and MRCP. The youngest patient in our study was a 12-year-old female having choledochal cyst, and the eldest was a 80-year-old male suffering from carcinoma of the head of pancreas. Patients in our study presented with various symptoms; we have counted each symptom separately, out of which common symptoms are yellowish discoloration of sclera and skin, right upper quadrant pain, nausea, vomiting, fever, dark colored urine, clay colored stools, weight loss, lump in abdomen, etc. Serum alkaline phosphatase, serum gamma glutamyltransferase (GGT), total serum bilirubin, and conjugated bilirubin level were assessed in our cases.
Statistical analysis was done by using descriptive and inferential statistics using chi-square test. Binary classification and software analysis were done using Statistical Package for the Social Sciences (SPSS) 17.0 version and GraphPad Prism 6.0 version; p < 0.05 is considered as level of significance.
Graph 1 shows maximum patients with obstructive jaundice were observed in elderly subjects >60 years age group.

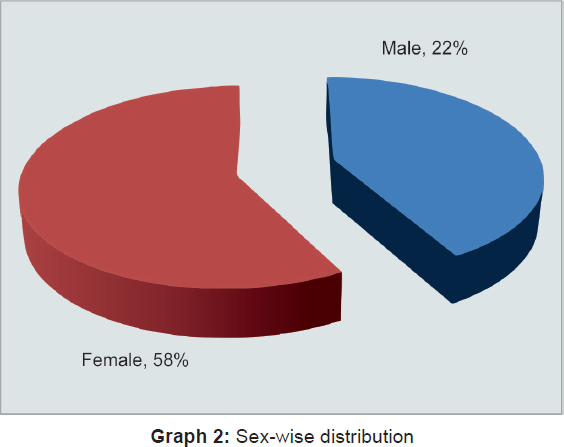
Graph 2 shows female preponderance in our study group with male to female ratio being 42:58, i.e., 1:1.40.
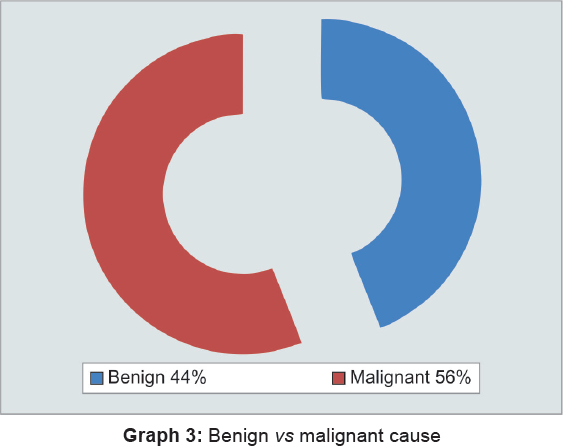
Graph 3 shows malignant causes are more frequently seen as cause of obstructive jaundice as compared with benign causes.
Graph 4 shows significant difference in benign and malignant causes in extremes of age groups. Benign causes are more common in young adults, with maximum number of patients between 16, 30, 31, 45 years of age, while maximum number of malignant causes is seen in elder age groups, i.e., 45 to 59 and 60 and above. Increase in age groups shows inverse relation with benign cause, while malignant cause shows direct relationship.
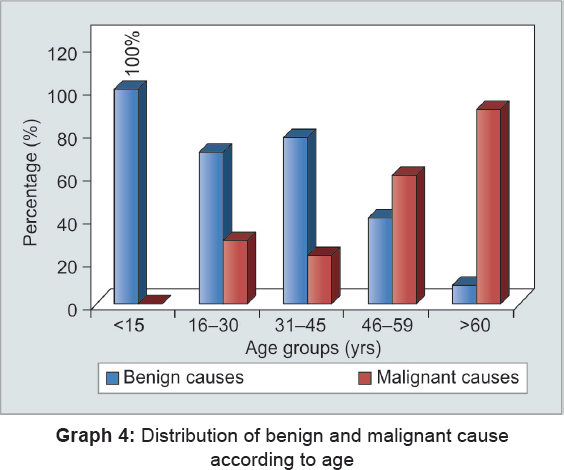
Table 1 shows that out of total benign causes choledocholithiasis is the most common benign cause comprising of 50% of total benign causes followed by pancreatitis being 18.8% of total.
| Various benign causes | Number | Percentage |
|---|---|---|
| Choledocholithiasis | 22 | 50.00 |
| Pancreatitis | 8 | 18.18 |
| Choledochal cyst | 4 | 9.09 |
| Trauma | 3 | 6.82 |
| Hydatid cyst | 2 | 4.55 |
| Sclerosing cholangitis | 3 | 6.82 |
| Sludge | 2 | 4.55 |
| Total | 44 | 100 |
Table 2 shows most common malignant cause in our study was carcinoma head of pancreas (26.79%) followed by periampullary carcinoma (21.43%) and cholangiocarcinoma (17.86%).
| Causes | Number | Percentage |
|---|---|---|
| Carcinoma head of pancreas | 15 | 26.79 |
| Periampullary carcinoma | 12 | 21.43 |
| Cholangiocarcinoma | 10 | 17.86 |
| Carcinoma gallbladder | 7 | 12.50 |
| Lymphoma | 3 | 5.36 |
| Klatskin tumor | 9 | 16.07 |
| Total | 56 | 100 |
Graph 5 shows significant difference of distribution of various causes among males and females. Benign causes are more common in females (most common cause being choledocholithiasis), with a male to female ratio of 1:2.66, while malignant causes are more common in males (most common malignant causes in males are carcinoma head of pancreas followed by periampullary carcinoma and cholangiocarcinoma), with a male to female ratio of 3:2.60 (Tables 3 to 8).

| Causes | Final diag. | On USG | Sensitivity | Specificity | PPV | NPV | Accuracy | p-value |
|---|---|---|---|---|---|---|---|---|
| Choledocholithiasis | 22 | 16 | 84.21 | 88 | 84.21 | 88 | 86.36 | 0.0001,S |
| Pancreatitis | 8 | 5 | 83.33 | 94.74 | 71.43 | 97.30 | 93.18 | 0.0001,S |
| Choledochal cyst | 4 | 3 | 75.00 | 95.00 | 60.00 | 97.44 | 93.18 | 0.0001,S |
| Trauma | 3 | 1 | 25 | 97.50 | 50 | 92.86 | 90.91 | 0.039,S |
| Hydatid cyst | 2 | 2 | 100 | 100 | 100 | 100 | 100.00 | 0.0001,S |
| Sclerosing cholangitis | 3 | 1 | 33.33 | 95.24 | 33.33 | 95.34 | 91.11 | 0.045,S |
| Sludge | 2 | 2 | 100 | 100 | 100 | 100 | 100 | 0.0014,S |
| Carcinoma head of pancreas | 15 | 10 | 76.92 | 95.35 | 85.71 | 88 | 87.72 | 0.0001,S |
| Periampullary carcinoma | 12 | 10 | 91.67 | 97.73 | 91.67 | 97.73 | 96.43 | 0.0001,S |
| Cholangiocarcinoma | 10 | 6 | 66.67 | 97.87 | 80.00 | 100 | 92.60 | 0.0001,S |
| Carcinoma gallbladder | 7 | 6 | 75 | 97.92 | 85.71 | 95.92 | 94.64 | 0.0001,S |
| Lymphoma | 3 | 3 | 100 | 100 | 100 | 100 | 100.00 | 0.0001,S |
| Klatskin tumor | 9 | 8 | 90 | 94.87 | 90 | 97.87 | 96.49 | 0.0001,S |
PPV: Positive predictive value; NPV: Negative predictive value; S: Significant
| Causes | Final diag. | On MRCP | Sensitivity | Specificity | PPV | NPV | Accuracy | p-value |
|---|---|---|---|---|---|---|---|---|
| Choledocholithiasis | 22 | 20 | 95.24 | 95.65 | 95.24 | 95.25 | 95.45 | 0.0001,S |
| Pancreatitis | 8 | 7 | 87.50 | 97.30 | 77.78 | 97.30 | 93.48 | 0.0001,S |
| Choledochal cyst | 4 | 4 | 100 | 100 | 100 | 100 | 100.00 | 0.0001,S |
| Trauma | 3 | 3 | 100 | 100 | 100 | 100 | 100.00 | 0.0001,S |
| Hydatid cyst | 2 | 2 | 100 | 100 | 100 | 100 | 100.00 | 0.0001,S |
| Sclerosing cholangitis | 3 | 2 | 66.67 | 97.56 | 33.33 | 95.24 | 95.45 | 0.045,S |
| Sludge | 2 | 2 | 100 | 100 | 100 | 100 | 100.00 | 0.0001,S |
| Carcinoma head of pancreas | 15 | 14 | 93.33 | 97.78 | 93.33 | 97.78 | 96.67 | 0.0001,S |
| Periampullary carcinoma | 12 | 10 | 90.91 | 95.56 | 83.33 | 97.73 | 94.64 | 0.0001,S |
| Cholangiocarcinoma | 10 | 9 | 90 | 94.65 | 81.82 | 97.78 | 96.50 | 0.0001,S |
| Carcinoma gallbladder | 7 | 7 | 100 | 100 | 100 | 100 | 100.00 | 0.0001,S |
| Lymphoma | 3 | 2 | 66.67 | 98.15 | 66.67 | 98.15 | 96.49 | 0.0001,S |
| Klatskin tumor | 9 | 9 | 100 | 100 | 100 | 100 | 100 | 0.0001,S |
PPV: Positive predictive value; NPV: Negative predictive value; S: Significant
| Histopathological diagnosis | ||||
|---|---|---|---|---|
| Benign | Malignant | Total | ||
| USG | Benign | 29 | 10 | 39 |
| Inconclusive | 6 | 3 | 9 | |
| Malignant | 9 | 43 | 52 | |
| Total | 44 | 56 | 100 | |
| Histopathological diagnosis | χ2-value | |||||
|---|---|---|---|---|---|---|
| Benign | Malignant | Total | ||||
| MRI with MRCP | Benign | 41 | 3 | 44 | χ2 = 77.13 | |
| Malignant | 3 | 53 | 56 | df = 1 | ||
| Total | 44 | 56 | 100 | p = 0.0001,S | ||
| USG | TP | FP | FN | TN | χ 2 -value | p-value |
|---|---|---|---|---|---|---|
| Benign | 29 | 10 | 9 | 52 | 35.87 | 0.0001,S |
| Malignant | 43 | 9 | 9 | 39 | 40.89 | 0.0001,S |
S: Significant
| MRCP | TP | FP | FN | TN | χ 2 -value | p-value |
|---|---|---|---|---|---|---|
| Benign | 41 | 3 | 2 | 54 | 80.73 | 0.0001,S |
| Malignant | 53 | 3 | 2 | 42 | 80.81 | 0.0001,S |
S: Significant
DISCUSSION
Obstructive jaundice is one of the most challenging conditions faced by general surgeons, which leads to significantly high mortality and morbidity.3
Surgical jaundice (obstructive) occurs due to various benign and malignant conditions causing any type of obstruction to the bile flow from liver to intestine.1
Early detection of the cause of obstructive jaundice and nature of the lesion helps surgeons to choose proper line of management. Various radiological investigations play a pivotal role in diagnosing the lesion, level of obstruction, and extent of disease. Our study has been conducted to determine the role of MRCP/MRI in cases of obstructive jaundice as compared with USG while keeping histopathology/postsurgery follow-ups and ERCP as a gold standard for final diagnosis.
In our study, we included a total of 100 patients suspected as having obstructive jaundice on clinical and biochemical parameters. The youngest patient in our study was a 12-year-old female suffering from choledochal cyst and eldest one was a 80-year-old male suffering from carcinoma head of pancreas.
In our study, there were a total of 58 females and 42 males showing female preponderance. This result is consistent with a study conducted by Gameraddin et al10 who reported that females are more frequently affected with obstructive jaundice than males. Maximum number of patients were seen in the age group more than 60 years, with mean age of presentation 46 ± 15 years.
Out of all studied patients with obstructive jaundice, 56 had malignant causes while 44 had benign causes; these results are consistent with those of Sharma and Ahuja,11 who in their study had observed 73.3% patients had malignant cause, while 24.7% had benign cause. Similar results were shown by Moghimi et al12 and Huang et al.13 It is also observed that benign causes are more frequently seen in females while malignancy is predominantly seen in elderly men; this finding was explained by Saluja et al.14
Siddique et al15 and Park et al16 stated that presence of gall stones attributed to cholesterol stones are presumed to be related to metabolic disorders, which are more commonly seen in women, and malignancy predominates in males due to their habits of alcohol abuse and tobacco chewing. The maximum number of benign causes is seen in age group of 16 to 30 and 31 to 45 years, while malignant causes are predominantly seen in the late 50s and above 60-year age group; increased incidence of malignant obstructive jaundice with increasing age has also been reported by Chalya et al17 and Siddique et al.15
In our study, majority of patients with obstructive jaundice presented with icterus, right upper quadrant pain, dark-colored urine, and clay-colored stools. And of all serological assessment done, significant changes were seen in serum alkaline phosphatase, serum GGT, and serum conjugated bilirubin. Similar study results were given by Verma et al.18
All patients in our study underwent USG prior to MRCP; out of all 44 benign causes choledocholithiasis (22 cases, i.e., 50% of all benign) was the commonest cause. Out of all 22 cases, 17 cases were females and 5 cases were males. Ultrasonography successfully detected 16 cases, while in 3 cases it misdiagnosed as calculus, 2 of them were further diagnosed as cholangiocarcinoma and 1 was adenomyomatosis on histopathology. In the remaining 3 cases USG was not able to detect the calculus due to the patient being fat and excessive bowel gases. Overall sensitivity, specificity, and diagnostic accuracy of USG were found to be 84.21, 88, and 86.36% respectively, and of MRCP 95.24, 95.65, and 95.45% respectively. Our study is consistent with that of Verghese et al19 who in 1999 reported that USG in the detection of common bile duct (CBD) stones showed sensitivity, specificity, and accuracy of 91, 88, and 92% respectively.20 Other similar studies are those of Laokpessi et al21 and Soto et al22; in their study they found sensitivity of 94% and specificity of 100% for detecting biliary calculi on MRCP. Suthar et al23 in 2015 found sensitivity, specificity, and accuracy of 100, 100, and 100% respectively, on MRCP. Similar results were also shown by Kim et al.20
There were a total of four cases of choledochal cyst in our study; of them USG was able to diagnose three cases; however, two cases of pseudocyst of pancreas were missed to be diagnosed as choledochal cyst due to its closed approximation with CBD and lower age group presentation of patient, giving sensitivity of 75%, specificity of 95%, and diagnostic accuracy of 93.18%. Magnetic resonance cholangiopancreatography diagnosed all four cases of choledochal cyst and was also able to differentiate them from pseudocyst of pancreas in two cases, which were falsely diagnosed by USG as choledochal cyst giving sensitivity, specificity, and diagnostic accuracy of 100%. Our study is in concordance with Bhatt et al,24 who in their study found 100% accuracy for USG and MRCP in diagnosing anatomical variants. Suthar et al23 showed 100% sensitivity, specificity, and diagnostic accuracy of MRCP and 80% sensitivity of USG for detecting choledochal cyst. Similar results were given by Raguraman,25 who studied 50 patients of anatomic variants diagnosed with MRCP out of which one was a case of biliary atresia and two were choledochal cysts. Both showed diagnostic accuracy of 100% and Al-Obaidi et al26 showed the same results.
Out of eight cases of pancreatitis, five patients were males and three patients were females. Ultrasonography successfully diagnosed five cases as pancreatitis which showed parenchymal calcification and prominent main pancreatic duct in cases of chronic pancreatitis. Ultrasonography misdiagnosed two cases of groove pancreatitis as carcinoma head of pancreas, one case of focal pancreatitis remained unrevealed due to excessive bowel gases and fatty patient. Thus, USG showed sensitivity of 83.33%, specificity of 94.74%, and diagnostic accuracy of 93.18%. Magnetic resonance cholangiopancreatography diagnosed seven of eight cases and missed one case of pancreatitis, which was associated with ascites. Ultrasonography found parenchymal calcification better than MRCP. Magnetic resonance cholangiopancreatography found to have better visualization of main pancreatic duct dilatation stating about its irregularity, proper etiology of chronic pancreatic and associated complication like presence of stricture, distal CBD calculus, and any parasite causing obstruction to both CBD and main pancreatic duct as compared with USG. Magnetic resonance cholangiopancreatography showed sensitivity, specificity, and diagnostic accuracy of 87.50, 97.30, and 93.48% respectively; this finding is in concordance with Yattoo et al27 who in 2014 showed diagnostic accuracy of USG is between 30 and 80% while that of MRCP is 80 to 90% in diagnosing chronic pancreatitis.
We had three cases of primary sclerosing cholangitis in our study, which showed multiple strictures, irregularities of bile ducts, and bile duct wall thickening on MRCP. Similar findings were described by Katabathina et al.28 In our study, USG showed insignificant thickening and peri-ductal increased echogenicity with dilated segments in one case; however, it failed to diagnose sclerosing cholangitis in the rest of the two cases. Ultrasonography showed sensitivity, specificity, and diagnostic accuracy of 33.33, 95.24, and 91.11% respectively; MRCP diagnosed two cases showing sensitivity, specificity, and diagnostic accuracy of 66.66, 97.56, and 95.45% respectively. Our results are comparable to a study done by Angulo et al29 who showed MRCP had an overall diagnostic accuracy of more than 90% in the detection of primary sclerosing cholangitis.
Out of all 17 benign strictures MRCP diagnosed 16 cases as benign stricture, and 1 case which was diagnosed as benign stricture on the basis of its morphological character came out to be malignant. Magnetic resonance cholangiopancreatography was able to detect level of obstruction in all cases. Out of all 17 benign strictures, 12 were located proximally, while 5 involved distal CBD, showing sensitivity, specificity, and diagnostic accuracy of 94.44, 96.30, and 100% respectively; this is similar to a study done by Singh et al30 who showed 100% sensitivity, specificity, and diagnostic accuracy of MRCP in diagnosing benign biliary stricture. Also, Al-Obaidi et al26 showed higher sensitivity (100%), specificity (98.5%), accuracy (98.7%) of MRI/MRCP for cases with benign stricture as compared with sensitivity of USG (20–40%), which is consistent with the present study. Bhatt et al24 found accuracy of MRCP being 100% in diagnosing benign biliary stricture. Our results are higher than those of Hintze et al,31 who in 1997 found sensitivity of 87% and specificity of 87% of MRCP for the diagnosis of benign stricture, and Li et al32 in their study found that sensitivity of MRCP in diagnosis of benign stricture was 81%, specificity 92%, and accuracy 87% (adjust reference accordingly; this may be due to improvement in spatial resolution and better software nowadays).
There were two cases of hydatid cyst of the liver; both were diagnosed correctly by USG and MRCP. Our findings comparable to those of Osilouridis et al33 who showed 80 to 90% accuracy of USG and 100% accuracy by MRCP and those of Al-Obaidi et al.26
Two cases of sludge causing obstruction to bile flow were accurately diagnosed by both USG and MRCP.
In our study, malignant preponderance was also seen in many previously done studies by Sharma and Ahuja,11 Moghimi et al,12 and Huang et al.13 Out of all 100 patients, 56 had malignant etiology; this kind of pattern in our study may be explained because the study was done in a tertiary hospital and malignant patients were referred to us for treatment. In our study, most common malignant cause was found to be carcinoma head of pancreas followed by periampullary and cholangiocarcinoma.
There were a total of 15 cases of carcinoma head of pancreas; out of them, USG was able to detect 10 cases; 1 case of groove pancreatitis was wrongly diagnosed as carcinoma head of pancreas and was later found to have annular pancreas with recurrent pancreatitis on MRI/MRCP. Another case of polypoidal intraluminal cholangiocarcinoma involving distal CBD was misdiagnosed as carcinoma head of pancreas, which was further diagnosed on MRCP as intraluminal cholangiocarcinoma. Ultrasonography had sensitivity, specificity, and diagnostic accuracy of 76.92, 95.35, and 87.72% respectively. Magnetic resonance imaging/MRCP diagnosed 14 cases of carcinoma head of pancreas; 1 case of focal pancreatitis was wrongly diagnosed as carcinoma head of pancreas. Magnetic resonance cholangiopancreatography showed sensitivity, specificity, and diagnostic accuracy of 93.33, 97.78, and 96.67% respectively. Ultrasound is unable to detect the locoregional spread accurately. Our findings are similar to a study done by Al-Obaidi et al26 in 2007 who found that sensitivity, specificity, and diagnostic accuracy of USG is 66.3, 80.7, and 73.75% respectively, while MRCP showing that sensitivity, specificity, and diagnostic accuracy of MRCP is 90, 97.8, and 95% respectively. Tam et al34 reported sensitivity of 80% and specificity of 95%, and Haminem et al34 in a study of 66 patients of suspected pancreatic cancers reported a diagnostic accuracy, sensitivity, and specificity of 91, 95, and 96%.
Out of all 10 cases of cholangiocarcinoma, USG successfully detected 6 cases. One case of benign focal thickening was wrongly diagnosed as cholangiocarcinoma and USG was not able to diagnose three cases showing sensitivity of 66.67%, specificity of 97.87%, and diagnostic accuracy of 92.60%; MRCP able to diagnose 9 cases correctly. Two cases of stricture were wrongly diagnosed as cholangiocarcinoma, giving sensitivity, specificity, and diagnostic accuracy of 90, 94.65, and 96.50% respectively; our study showed comparable results with those of Singh et al,30 showing sensitivity, specificity, and diagnostic accuracy of USG 66.67, 100, and 96% respectively, and of MRCP of 83.33, 98, and 100% respectively. Similar results were also given by Guibaud et al,35 Barish and Soto36 and Pavone et al,37 who concluded their studies with sensitivities ranging from 80 to 86% and specificities of 96 to 98% and diagnostic accuracies of 91 to 100%.
Out of all nine cases of Klatskin tumor, USG was able to detect eight cases. One case of Klatskin tumor was misdiagnosed as benign stricture; MRCP diagnosed all nine cases accurately. Ultrasonography showed sensitivity, specificity, and accuracy of 90, 94.87, and 96.49% respectively, while MRCP showed sensitivity, specificity, and accuracy of 100% respectively. Our study is comparable to that of Raguraman25 who found 100% accuracy for both USG and MRCP and Bhatt et al24 who found 83% accuracy of USG and 100% accuracy of MRCP. Our USG findings also approximate with findings by Hann et al38 who reported that USG detected 87% of Klatskin tumor.
One case was diagnosed to have extrinsic malignant nodal compression in both the modalities approaching 100% accuracy in both, later diagnosed as case of metastatic lymph node compressing CBD.
Out of all seven cases of carcinoma gallbladder, USG successfully detected six cases and one case was falsely diagnosed as inflammatory thickening. Ultrasonography was unable to show subtle local metastasis to liver in four cases; however, MRCP diagnosed all cases of carcinoma gallbladder with its local metastasis and involvement of intrahepatic biliary radicles. In our study, USG showed sensitivity, specificity, and diagnostic accuracy of 75, 97.92, and 94.64% respectively, and for MRCP/MRI 100% our study is in concordance with that of Bhatt et al.24 In their study, they found an accuracy of 100% for MRCP alone in diagnosing gallbladder carcinoma. Yoshimitsu et al39 in their study showed the accuracies of MRI, helical CT, and ultrasound were 93, 75, and 66% respectively.
Out of 27 cases of malignant strictures, MRCP gave accurate findings in 24 and misdiagnosed 1 case as malignant stricture, which turned out to be benign. Magnetic resonance cholangiopancreatography correctly diagnosed level of obstruction in all malignant strictures; in majority of the cases it had involved confluence and proximal CBD showing sensitivity, specificity, and diagnostic accuracy of 88.89, 94.44, and 92.24% respectively. Our results are in concordance with those of Singh et al30 showing sensitivity of 85.7%, specificity of 96.3%, and accuracy of 93.3%. Similar results were seen in studies done by Reinhold and Bret40 and Lopera et al.41
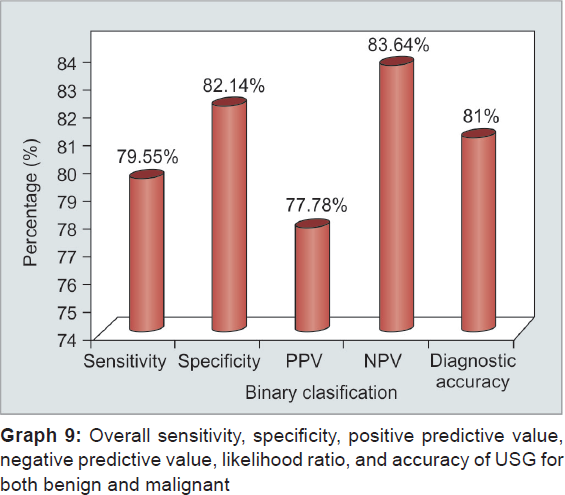
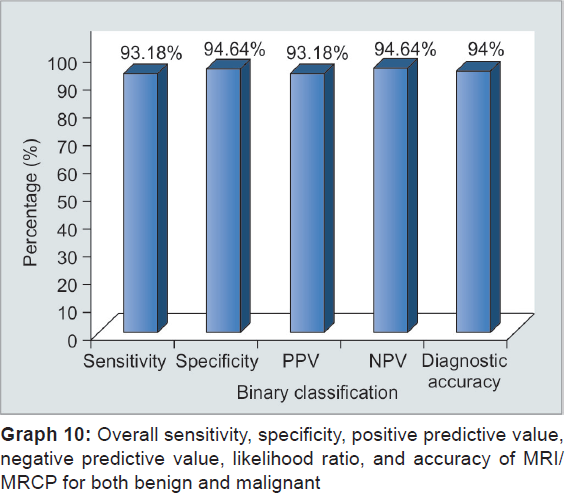
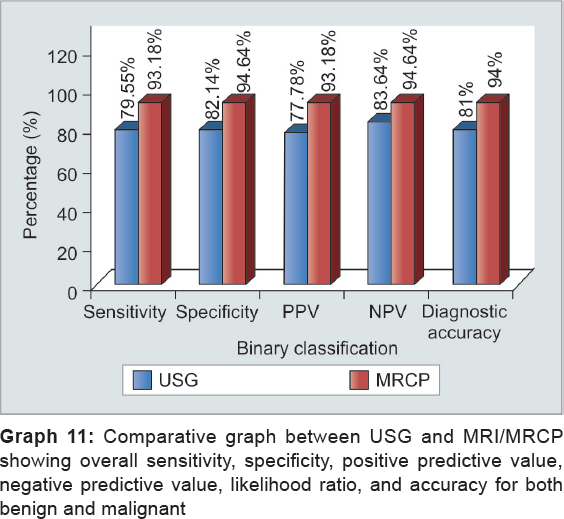
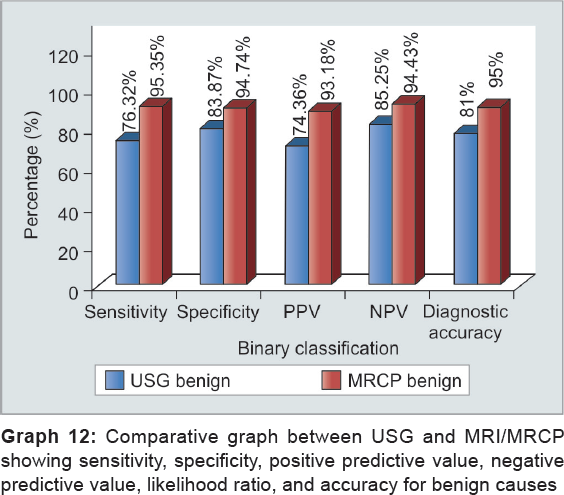
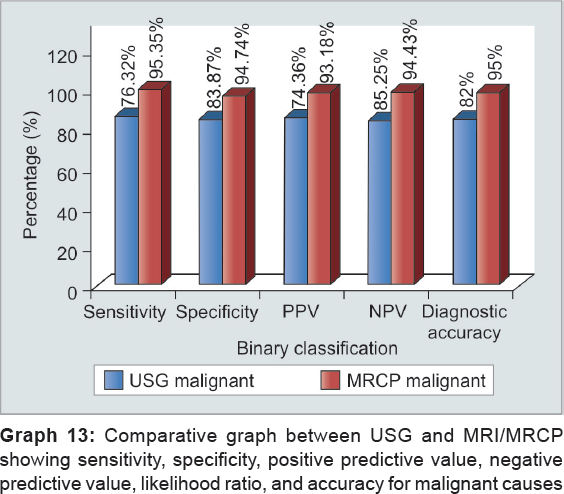
From the above observations, overall sensitivity, specificity, and accuracy of USG to diagnose collectively both benign and malignant cause are 79.55, 82.14, and 81% respectively, while of MRCP is 93.18, 94.64, and 94% respectively. Ultrasonography can differentiate benign from malignant with sensitivity, specificity, and diagnostic accuracy of 76.32, 83.87, and 81% respectively, while it can make out malignant from benign with sensitivity, specificity, and diagnostic accuracy of 82.69, 81.25, and 82% respectively. However, MRCP effectively diagnosed benign cases with sensitivity, specificity, and diagnostic accuracy of 95.35, 94.74, and 95% respectively, and it can diagnose malignant with sensitivity, specificity, and diagnostic accuracy of 96.36, 93.33, and 95% respectively (Graphs 6 to 13). Our results are in concordance with those of Amandeep et al.30 In their study, for benign causes, USG showed sensitivity, specificity, and diagnostic accuracy of 80.77, 95.83, and 88% respectively, while for malignant causes, it showed to have sensitivity, specificity, and diagnostic accuracy of 79.17, 96.15, and 88% respectively. In their study, they found with MRCP for benign lesions sensitivity, specificity, and diagnostic accuracy was 100, 95.83, and 98% respectively, whereas for malignant lesions, they observed sensitivity, specificity, and diagnostic accuracy of 95.83, 100, and 98% respectively. Similar results were shown by Verma et al18 who demonstrated the sensitivity and specificity of 85.3 and 88.4% respectively, on ultrasound, 92.3 and 86% on MRCP respectively, for detecting the benign etiology of obstruction, while the sensitivity and specificity of 88.4 and 85.3% on ultrasound and 94.2 and 95% on MRCP respectively, were found for detecting the malignant etiology of obstruction. Francesco et al42 demonstrated similar findings for benign lesions in their study who stated the diagnostic accuracy, sensitivity, and specificity of USG were 78.62, 16.67, and 97.29% respectively, and of MRCP was 93.13, 90, and 94% respectively; the diagnostic accuracy, sensitivity, and specificity of USG being 93.13, 98.23 and 92.59% and 93.13, 90, and 94% of MRCP respectively. Similar results were shown by Pasanen et al,43 Sharma and Ahuja,11 Saluja et al,14 Park et al,16 and Hekimoglu.44



LIMITATIONS
Like any other modality, MRI/MRCP has also few limitations:
Claustrophobia is a common limitation of any MRI study and also one of the limitations of MRCP.
No therapeutic and interventional procedure can be carried out with the help of MRCP.
Breath-holding is not possible in elderly, children, and debilitated patients.
It is time consuming and requires cooperation by the patient.
Few artifacts and presence of fluid within gastrointestinal tract lowers the image quality, thus leading to compromised reports.
Secretin was only given in four cases due to low affordability of patient, so role of secretin cannot be evaluated.
Ultrasonography was found to have limitations in diagnosing distal CBD and main pancreatic duct pathologies, especially in cases of fatty patients and patients having excessive bowel gases.
CONCLUSION
Based upon our study, following conclusions can be drawn:
Ultrasonography was found to be a good screening modality, while MRCP was found to be a better noninvasive, radiation-free diagnostic tool in the evaluation of cases of obstructive jaundice. Magnetic resonance cholangiopancreatography is a better noninvasive helping tool for surgeons, thereby differentiating obstructive from nonobstructive cause. Preoperative evaluation of suspected cases of obstructive jaundice lets surgeons know better about anatomy, anatomical variants, level of obstruction, nature and extent of lesion, which in turn helped them to go for better therapeutic option like biliary enteric anastomosis.
With the use of MRCP, we can overcome limitations of USG by visualizing whole biliary tree, especially its distal aspect. It is also a very useful tool in case of obese patients and children.
Invasive procedures like ERCP can be avoided as a diagnostic procedure because of high diagnostic specificity and accuracy of MRCP. It can even be used in failed ERCP cases and also shows biliary tree proximal as well as distal to the level of obstruction with appropriate accuracy.
Magnetic resonance cholangiopancreatography is one of the most promising tools for diagnosing most of the lesions and its nature with high degree of accuracy. There is now enough evidence to suggest that the efficacy of MRI and MRCP is at par with that of ERCP and can be considered as the gold standard for diagnostic evaluation of the pancreaticobiliary system.
GALLERY
Case 1
Ultrasonography in a 12-year-old girl: There is fusiform dilatation of proximal CBD with mild prominence of intrahepatic biliary radical. On coronal T2-weighted imaging and MRCP same findings s/o type I choledochal cyst are shown (Fig. 1).

- Choledochal cyst
Case 2
Ultrasonography showing mixed echogenic collection in right lobe of liver showing extension into intrahepatic biliary radical and gallbladder; USG showed freely moving membranes in this case; Magnetic resonance imaging/MRCP: Axial T2-weighted imaging showing mixed intensity collection predominantly hyperintense lesion with hypointense serpentine membrane within; MRCP image showing serpentine hypointense membrane noted within gallbladder and CBD (Fig. 2).

- Hydatid cyst with intrabiliary rupture
Case 3
Ultrasonography showing dilated CBD and intrahepatic biliary radical with ill-defined hyperechoic mass lesion noted in a periampullary region, abutting head of pancreas and seen separately from pancreas; Magnetic resonance imaging/MRCP: Axial and coronal T2-weighted imaging showing isointense mass lesion in the pancreas with hyperintense rim around it. On MRCP image it is seen to be within distal CBD causing obstruction and dilated CBD and intrahepatic biliary radical (Fig. 3).

- Extrahepatic distal common bile duct cholangiocarcinoma
Case 4
Ultrasonography showing hyperechoic calculus noted impacted within cystic duct and prominent proximal CBD; Magnetic resonance cholangiopancreatography/MRI: Coronal T2-weighted imaging showing impacted calculus within cystic duct causing compression over CBD. This case was known for repeated choledocholithiasis and repeated episodes of jaundice (Fig. 4).

- Mirizzi syndrome
Case 5
Ultrasonography showing ill-defined hypoechoic mass lesion in the pancreatic head region causing dilatation of CBD and intrahepatic biliary radical; Magnetic resonance imaging/MRCP: Axial T2-weighted imaging (T2WI) and MRCP image showing dilated main pancreatic duct and CBD giving double duct sign, another axial T2WI image showing predominantly hyperintense mass lesion in the pancreatic head region with associated dilatation of CBD and intrahepatic biliary radicles (Fig. 5).

- Carcinoma head of pancreas
Source of support:
Nil
Conflict of interest:
None.
REFERENCES
- Hepatic and biliary disorders.The Merck manual of diagnosis and therapy. (17th). Whitehouse Station (NJ): Merck & Co; 1999.
- [Google Scholar]
- Jaundice. Maingot's abdominal operations. Vols. I and II. (10th). Singapore: McGraw Hill; 2001. p. :315-336.:1701-336.
- [Google Scholar]
- Ultrasound in obstructive jaundice: prospective evaluation of site and cause. Radiology. 1983;147(2):511-515.
- [CrossRef] [PubMed] [Google Scholar]
- The biliary tract.Grainger and Allison's diagnostic radiology–a textbook of medical imaging. (4th). London: Churchill Livingstone, Harcourt Publishers Limited; 2001.
- [Google Scholar]
- The role of intravenous cholangiography in preoperative assessment for laparoscopic cholecystectomy. Br J Radiol. 1993;66(792):1125-1127.
- [CrossRef] [PubMed] [Google Scholar]
- Dilated biliary tract: evaluation with MR cholangiography with a T2 weighted contrast-enhanced fast sequence. Radiology. 1991;181(3):805-808.
- [CrossRef] [PubMed] [Google Scholar]
- The role of ultrasound in diagnosis of obstructive jaundice causes in Sudanese population. IOSR J Nurs Health Sci. 2013;1:25-28.
- [CrossRef] [Google Scholar]
- Aetiological spectrum of Obstructive jaundice and diagnostic ability of ultrasonography: a clinician's perspective. Trop Gastroenterol. 1999;20(4):167-169.
- [Google Scholar]
- Obstructive jaundice in Iran: factors affecting early outcome. Hepatobiliary Pancreat Dis Int. 2008;7(5):515-519.
- [Google Scholar]
- The common causes and differential diagnosis of malignant jaundice. Zhonghua Nei Ke Za Zhi. 1993;32(6):400-404. (article in Chinese)
- [Google Scholar]
- Differentiation between benign and malignant hilar obstructions using laboratory and radiological investigations: a prospective study. HPB. 2007;9(5):373-382.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of the aetiological spectrum of obstructive jaundice. J Ayub Med Coll Abbottabad. 2008;20(4):62-66.
- [Google Scholar]
- Acute cholecystitis: comparison of MR cholangiography and US. Radiology. 1998;209(3):781-785.
- [CrossRef] [PubMed] [Google Scholar]
- Etiological spectrum and treatment outcome of obstructive jaundice at a University teaching Hospital in northwestern Tanzania: a diagnostic and therapeutic challenges. BMC Res Notes. 2011;4:147.
- [CrossRef] [PubMed] [Google Scholar]
- Obstructive jaundice–aetiological spectrum, clinical, biochemical and radiological evaluation at a tertiary care teaching hospital. Internet J Trop Med. 2010;7(2)
- [CrossRef] [Google Scholar]
- A prospective comparison of MRCP with ERCP in the evaluation of patients with suspected biliary tract diseases. Clin Radiol. 1999;54(8):513-520.
- [CrossRef] [PubMed] [Google Scholar]
- Using MR cholangiopancreatography to reveal anomalous pancreaticobiliary ductal union in infants and children with choledochal cysts. AJR Am J Roentgenol. 2002;179(1):209-214.
- [CrossRef] [PubMed] [Google Scholar]
- Value of magnetic resonance cholangiography in the preoperative diagnosis of common bile duct stones. Am J Gastroenterol. 2001;96(8):2354-2359.
- [CrossRef] [PubMed] [Google Scholar]
- Detection of choledocholithiasis with MR cholangiography: comparison of 3D FSE and single and multisection half Fourier rare sequences. Radiology. 2000;215(3):737-745.
- [CrossRef] [PubMed] [Google Scholar]
- Role of MRCP in differentiation of benign and malignant causes of biliary obstruction. J Clin Diagn Res. 2015;9(11):TC08-TC12.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of diagnostic accuracy between USG and MRCP in biliary and pancreatic pathology. Indian J Radiol Imaging. 2005;5(2):177-181.
- [CrossRef] [Google Scholar]
- MRI combined with MRCP versus helical CT in evaluation of patients with obstructive jaundice. Int J Recent Sci Res. 2015;6(4):3642-3650.
- [Google Scholar]
- The role of ultrasound and magnetic resonance imaging in the diagnosis of obstructive jaundice. Imaging Diagn Obstruct Jaundice. 2007;6(1):7-17.
- [Google Scholar]
- The efficacy of magnetic resonance cholangiopancreatography in assessing the etiology of acute idiopathic pancreatitis. Int J Hepatobiliary Pancreat Dis. 2014;4:32-39.
- [CrossRef] [Google Scholar]
- Adult bile duct strictures: role of MR imaging and MR cholangiopancreatography in characterization. Radiographics. 2014;34(3):565-586.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance cholangiography in patients with biliary disease: its role in primary sclerosing cholangitis. J Hepatol. 2000;33(4):520-527.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic accuracy of MRCP as compared to ultrasound/CT in patients with obstructive jaundice. J Clin Diagn Res. 2014;8(3):103-107.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical significance of magnetic resonance cholangiopancreatography (MRCP) compared to endoscopic retrograde cholangiopancreatography (ERCP) Endoscopy. 1997;29(3):182-187.
- [CrossRef] [PubMed] [Google Scholar]
- Image directed and color Doppler studies of the gallbladder tumours. J Clin Ultrasound. 1994;22(9):551-555.
- [CrossRef] [PubMed] [Google Scholar]
- Frank intrahepatic rupture of hepatic hydatid cyst, evaluation with MRI & MRCP. ECR (01)ECR (11):303.
- [Google Scholar]
- Diagnosis, staging and surveillance of pancreatic cancer. AJR. 2003;180(5):1311-1323.
- [CrossRef] [PubMed] [Google Scholar]
- Bile duct obstruction and choledocholithiasis: diagnosis with MR cholangiography. Radiology. 1995;197(1):109-115.
- [CrossRef] [PubMed] [Google Scholar]
- MR cholangiopancreatography: techniques and clinical applications. AJR. 1997;169(5):1295-1303.
- [CrossRef] [PubMed] [Google Scholar]
- MRI of the biliary and pancreatic ducts. Eur Radiol. 1999;9(8):1513-1522.
- [CrossRef] [PubMed] [Google Scholar]
- Cholangio carcinoma at the hepatic hilus: sonographic findings. Am J Roentgenol. 1997;168(4):985-989.
- [CrossRef] [PubMed] [Google Scholar]
- Dynamic MRI of the gallbladder lesions: differentiation of benign from malignant lesions. J Magn Reson Imaging. 1997;7(4):696-701.
- [CrossRef] [PubMed] [Google Scholar]
- MR cholangiopancreatography. Abdom Imaging. 1996;21(2):105-116.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant hilar and perihilar biliary obstruction: use of MR cholangiography to define the extent of biliary ductal involvement and plan percutaneous interventions. Radiology. 2001;220(1):90-96.
- [CrossRef] [PubMed] [Google Scholar]
- A comparative study in 131 patients with suspected biliary obstruction. Med Sci Monit. 2005;11(3):8-18.
- [Google Scholar]
- Diagnostic accuracy of ultrasound, computed tomography, and endoscopic retrograde cholangiopancreatography in the detection of obstructive jaundice. Scand J Gastroenterol. 1991;26(11):1157-1164.
- [CrossRef] [PubMed] [Google Scholar]
- MRCP vs. ERCP in the evaluation of biliary pathologies: review of current literature. J Dig Dis. 2008;9(3):162-169.
- [CrossRef] [PubMed] [Google Scholar]







