Translate this page into:
Post-Operative Analgesia and Enhanced Recovery after Pecs 1 and Pecs 2 Blocks in Patients Undergoing Modified Radical Mastectomy/Breast-Conserving Surgery with Axillary Lymph Nodal Clearance

*Corresponding author: Dr. James Thiek, Department of Surgical Oncology, Assam Cancer Care Foundation, Barpeta, India. jmsthiek@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Thiek J, Sharma D, Guha A, Kalita L. Post-Operative Analgesia and Enhanced Recovery after Pecs 1 and Pecs 2 Blocks in Patients Undergoing Modified Radical Mastectomy/Breast-Conserving Surgery with Axillary Lymph Nodal Clearance. Int J Recent Sur Med Sci. 2023;9:134-8. doi: 10.25259/IJRSMS-2022-12-2
Abstract
Background
Patients undergoing modified radical mastectomy (MRM)/breast-conserving surgery (BCS) with axillary nodal clearance experience significant post-operative pain, resulting in immobilization and increased usage of analgesics. These factors in turn result in delayed discharge.
The pecs 1 and pecs 2 blocks have proven to be of significant benefit in relieving post-operative pain in such patients.
Objectives
A case series was performed at our institute to note the effects of pecs 1 and pecs 2 blocks on post-operative opioid use, early mobilization of the upper limbs, decreased incidence of early post-operative limb swelling and enhanced recovery after surgery.
Material and Methods
We included six patients who underwent BCS with axillary lymph node dissection/MRM wherein intraoperative pecs 1 and pecs 2 blocks were used.
Patients were given pecs 1 and 2 blocks with 10+20 mL 0.25% injection of bupivacaine under ultrasound guidance after induction.
Results
In our study, opioids were completely avoided and it was seen that post-operative pain was adequately controlled with single doses of non-steroidal anti-inflammatory drugs if patients received intra-operative pecs 1 and 2 blocks. The pain control was rather sustained and adequate for the institution of early post-operative physiotherapy and thus early discharge and enhancing recovery after surgery.
Conclusion
Post-operative analgesia provided by pecs 1 and 2 blocks resulted in adequate and sustained pain control for early institution of upper limb physiotherapy and mobilization of patients after MRM/BCS with axillary lymph node dissection, which subsequently results in decreased incidence of early post-operative oedema of limb on operated side and early recovery after surgery.
Keywords
Carcinoma breast
Modified radical mastectomy
pecs block
Surgery
Oncology
Case Series
Case 1
A 36-year-old female belonging to ASA class 1, diagnosed with carcinoma in the left breast, underwent left modified radical mastectomy (MRM) under general anaesthesia. The patient was given pecs 1 and 2 blocks with 10+20 mL 0.25% inj. of bupivacaine under ultrasound guidance after induction. Ten hours after the surgery, the patient complained of pain with a visual analogue scale (VAS) score of 4. Infusion of paracetamol 1 gm was given after which pain was alleviated. On post-operative day one, upper limb physiotherapy was initiated and the patient was doing it without any discomfort or pain. On post-operative day two, the limb was evaluated for any oedema, which was absent. The patient was doing physiotherapy as directed. She was discharged with drain after adequate drain care was taught to her caretakers.
Case 2
A 54-year-old female belonging to ASA class 2, diagnosed with carcinoma in the left breast, underwent left MRM under general anesthesia. The patient was given pecs 1 and 2 blocks with 10+20 mL 0.25% inj. of bupivacaine under ultrasound guidance after induction. Ten hours after the surgery, the patient had no complaint of post-operative pain. On post-operative day one, upper limb physiotherapy was initiated and the patient was able to do it without any discomfort or pain. On post-operative day two, the limb was evaluated for any oedema, which was absent. The patient was doing physiotherapy as directed. She was discharged with drain after adequate drain care was taught to her caretakers.
Case 3
A 45-year-old female belonging to ASA class 1, diagnosed with carcinoma in the right breast, underwent right MRM under general anesthesia.[1–7] The patient was given pecs 1 and 2 blocks with 10+20 mL 0.25% inj. of bupivacaine under ultrasound guidance after induction. Six hours after the surgery, the patient complained of pain with a VAS score of 5. Infusion of paracetamol 1 gm was given after which pain was alleviated. On post-operative day one, upper limb physiotherapy was started and the patient was able to do it out with some pain with a VAS score of 3; pain was controlled with oral aceclofenac 100 mg. On post-operative day two, the limb was evaluated for any oedema, which was absent, and the pain also resolved. The patient was doing physiotherapy as directed. She was discharged with drain after adequate drain care was taught to her caretakers.
Case 4
A 52-year-old female belonging to ASA class 2, diagnosed with carcinoma in the left breast, underwent left MRM under general anesthesia. The Patient was given pecs 1 and 2 blocks with 10+20 mL 0.25% inj. of bupivacaine under ultrasound guidance after induction. Six hours after the surgery, the patient complained of pain with a VAS score of 3. Infusion of paracetamol 1 gm was given after which pain was alleviated. On post-operative day one, upper limb physiotherapy was initiated and the patient was able to do it without any pain or discomfort. On post-operative day two, the limb was evaluated for any oedema, which was absent, and the pain also resolved. Patient was carrying out physiotherapy as directed. Patient was discharged with drain after adequate drain care was taught to her caretakers.
Case 5
A 58-year-old female belonging to ASA class 2, diagnosed with carcinoma in the right breast, underwent right MRM under general anesthesia. The patient was given pecs 1 and 2 blocks with 10+20 mL 0.25% inj. of bupivacaine under ultrasound guidance after induction. Eight hours after the surgery, the patient complained of pain with a VAS score of 6. Infusion of paracetamol 1 gm was given after which pain was alleviated. On post-operative day one, upper limb physiotherapy was initiated and the patient was able to do it without any pain or discomfort. On post-operative day two, the limb was evaluated for any oedema, which was absent, and the pain also resolved. The patient did physiotherapy as directed. She was discharged with drain after adequate drain care was taught to her caretakers.
Case 6
A 41-year-old female belonging to ASA class 1, diagnosed with carcinoma in the right breast, underwent right MRM under general anesthesia. The patient was given pecs 1 and 2 blocks with 10+20 mL 0.25% inj. of bupivacaine under ultrasound guidance after induction. Eight hours after the surgery, the patient complained of pain with a VAS score of 3. Infusion of paracetamol 1 gm was given after which pain was alleviated. On post-operative day one, upper limb physiotherapy was initiated and the patient did it without any pain or discomfort. On post-operative day two, the limb was evaluated for any oedema, which was absent, and the pain also resolved. The patient was doing physiotherapy as directed. She was discharged with drain after adequate drain care was taught to her caretakers.
Discussion
Use of peripheral nerve block as part of comprehensive anaesthesia care is becoming a norm these days.[1–7]
Post-operative pain and the resulting immobility is a major morbidity, which delays the initiation of upper limb physiotherapy, which in turn leads to a delay in discharge of the patient and results in post-operative oedema of the limb on the operated site.
Control of post-operative pain after MRM usually needed high dose of opioids, which have a spectrum of side effects. In our study, opioids were completely avoided and post-operative pain was adequately controlled with single doses of non-steroidal anti-inflammatory drugs if patients received intra-operative pecs 1 and 2 blocks. The pain control was rather sustained and adequate for the institution of early post-operative physiotherapy facilitating early discharge and thus enhancing recovery after surgery.
A case of carcinoma left breast who underwent left BCS + axillary lymph node dissection at our cancer center, immediate post-operative pictures [Figure 1]. A case of carcinoma left breast who underwent left Breast conserving surgery (BCS) + axillary lymph node dissection at our cancer center, immediate post-operative pictures [Figure 2]. Same case post-operative day 7 picture [Figure 3]. Same case post-operative day 14 picture [Figure 4]. A case of paget’s disease of the nipple with underlying invasive ductal carcinoma of left breast planned for left modified radical mastectomy (MRM) – pre-operative pictures [Figure 5]. A case of paget’s disease of the nipple with underlying invasive ductal carcinoma of left breast planned for left modified radical mastectomy (MRM)– pre-operative pictures [Figure 6]. Intra-operative picture of the same patient – Axillary Vein (AV) and Thoraco-Dorsal Pedicle (TDP) are both marked [Figure 7]. Intra-operative picture of the same patient – Thoraco-Dorsal Pedicle (TDP) and Long Thoracic Nerve (LTN) are marked, respectively [Figure 8].

- A case of carcinoma left breast who underwent left BCS + axillary lymph node dissection at our cancer center, immediate post-operative pictures.

- A case of carcinoma left breast who underwent left Breast conserving surgery (BCS) + axillary lymph node dissection at our cancer center, immediate post-operative pictures.

- Same case post-operative day 7 picture.

- Same case post-operative day 14 picture.

- A case of paget’s disease of the nipple with underlying invasive ductal carcinoma of left breast planned for left modified radical mastectomy (MRM) – pre-operative Frontal view.

- A case of paget’s disease of the nipple with underlying invasive ductal carcinoma of left breast planned for left modified radical mastectomy (MRM)– pre-operative left view.

- Intra-operative picture of the same patient – Axillary Vein (AV) and Thoraco-Dorsal Pedicle (TDP) are both marked.
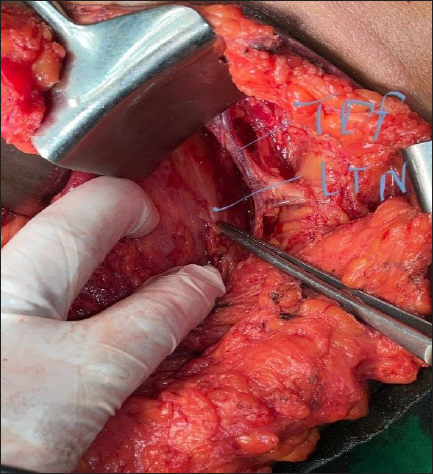
- Intra-operative picture of the same patient –Thoraco-Dorsal Pedicle (TDP) and Long Thoracic Nerve (LTN) are marked, respectively.
Conclusion
In our study, post-operative analgesia provided by pecs 1 and 2 blocks resulted in adequate and sustained pain control for early institution of upper limb physiotherapy and mobilization of patients after MRM/BCS with axillary lymph node dissection, which subsequently results in decreased incidence of early post-operative oedema of the limb on the operated side and early recovery after surgery. It also negated the need for high-dose opioids post-operatively, which results in less opioid-related side effects.
Ethical approval
The need for ethical clearance was waived as this was a retrospective study.
Acknowledgment
None.
Declaration of patients consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Consent statement
Informed and written consent from the patients and family members was acquired for the participation of the patients in the study and the use and publication of the patient data in the said study.
References
- The ‘pecs block’: a novel technique for providing analgesia after breast surgery. Anaesthesia. 2011;66:847-8.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound description of pecs II (Modified Pecs I): a novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012;59:470-5.
- [CrossRef] [PubMed] [Google Scholar]
- Pectoralis-II myofascial block and analgesia in breast cancer surgery: A systematic review and meta-analysis. Anesthesiology. 2019;131:630-48.
- [CrossRef] [PubMed] [Google Scholar]
- Pectoral nerves I and II blocks in multimodal analgesia for breast cancer surgery: A randomized clinical trial. Reg anesth Pain Med. 2015;40:68-74.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of pectoral nerve block versus thoracic paravertebral block for postoperative analgesia after radical mastectomy: A randomized controlled trial. Br J Anaesth. 2016;117:382-6.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective double blind randomized placebo-controlled clinical trial of the pectoral nerves (Pecs) block type II. J Clin Anesth. 2017;40:46-50.
- [CrossRef] [PubMed] [Google Scholar]
- Single-shot pectoral plane (Pecs I and Pecs II) blocks versus continuous local anaesthetic infusion analgesia or both after non-ambulatory breast-cancer surgery: A prospective, randomised, double-blind trial. Br J Anaesth. 2018;120:846-53.
- [CrossRef] [PubMed] [Google Scholar]







