Translate this page into:
A Prospective Type of Study Comparing Functional and Radiological Outcome Between the Use of Long and Short Proximal Femoral Nail in Treating Patients with Intertrochanteric Femur Fractures

*Corresponding author: Dr. Anubhav Viresh Kumar Agrawal, Department of Orthopaedics, ND Desai Medical College and Hospital, College Road, Nadiad, Gujarat, India. anubhavagrawal64@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agrawal Anubhav VK, Vala PC, Patel AH, Patel B. A Prospective Type of Study Comparing Functional and Radiological Outcome Between the Use of Long and Short Proximal Femoral Nail in Treating Patients with Intertrochanteric Femur Fractures. Int J Recent Surg Med Sci. 2024;10:94-101. doi: 10.25259/IJRSMS_19_2024.
Abstract
Objectives
To assess the functional and radiological outcome of long and short PFN for treating intertrochanteric femur fractures.
Material and Methods
A prospective hospital-based study was conducted on 60 patients in a tertiary hospital between May 2022 and June 2023, which were randomized into Group A (patients treated with short PFN) and Group B (patients treated with long PFN) using a computer-based table of random numbers. Patients were followed up by 12 days one, three, and six months. Functional outcome was assessed in terms of Harris Hip Score (HHS), and radiological outcome was measured in terms of time of union, complications, and fracture alignment.
Results
The majority of patients were between 60 and 65 years old. The most common cause of the mode of injury was trivial falls (65.00%). Mean HHS score after 6, 12, 16, and 24 weeks for Group A and B was 75.96 and 76.25, 81.16 and 82.52, 84.01 and 86.23 and 88.94 and 90.11, respectively. Mostly, complication was found in Group B (16.67%) compared to Group A (13.33%). Duration of surgery was 71.4 minutes for Group A and 90.6 minutes for Group B. Mean radiological time to union for group A and B was 16.4 and 17 weeks, respectively.
Conclusion
PFN is a highly efficient implant, irrespective of length, used in the fixation of intertrochanteric femur fractures falling into the category of AO/OTA 31-A1.31-A2. Short PFN has an advantage in terms of decreased operative time C-arm exposure, whereas long PFN should be preferred in elderly patients due to the high chances of osteoporosis, as it splints the entire length of the diaphysis, preventing stress riser and incidence of peri-implant fracture.
Keywords
Intertrochanteric femur fracture
AO/OTA classification
Harris hip score
proximal femoral nail (PFN)
INTRODUCTION
Intertrochanteric femur fractures are the most commonly operated fracture type globally. The residual lifetime risk of hip fracture at 50 years of age is estimated to be 5.6% for men and 20% for women.[1]
This is more common in elderly females due to a history of slip and fall at home, and in younger patients, it is due to high-velocity trauma.[1] Treatment options available are either intramedullary or extramedullary devices. The type of implant used for fracture fixation depends on the stability of the fracture pattern. The intact posteromedial cortex is an indicator of a stable fracture pattern, as it can resist compressive loads after it is reduced. Unstable fracture patterns include posteromedial comminution, fracture of the lateral wall, Basi cervical type pattern, displaced lesser trochanter fractures, reverse obliquity patterns, and failure to reduce fracture prior to internal fixation.[1]
For a stable fracture pattern, a dynamic hip screw (DHS) is the most common implant used for fracture fixation. For unstable fracture types, incidences of limb shortening, medialisation of distal fragments, and implant cutouts are high. This led to the development of intramedullary implants or cephalomedullary nails (CMN).[2]
Among CMN, some surgeons prefer using long proximal femoral nail (PFN) as it would avoid diaphyseal stress riser by splinting the entire length of the femur, thereby reducing the risk of peri-implant fracture. Also, it has nullified the incidence of postoperative anterior thigh pain. Increasing the working length is considered a better fixation device for intertrochanteric fractures with subtrochanteric extension.
Short PFN has the advantage of shorter operative duration, thus reducing intraoperative blood loss and, hence requirement for blood transfusion. However, it provides unstable fixation for fractures with subtrochanteric extension.[3] So, this study aims to compare the functional outcome of short and long PFN in treating intertrochanteric femur fractures.
MATERIAL AND METHODS
A clinical randomized retrospective type of study was conducted among 60 (age >20 years) patients presenting with intertrochanteric femur fracture (<2 weeks old) at the Department of Orthopaedics at N.D Desai Medical College and Hospital, Nadiad, Gujarat, between May 2022 and June 2023.
Sample size
The sample size for the proposed study is approximately 60.
We accepted p < 0.05 as significant, meaning we are ready to accept the probability that the result observed due to chance is 5%. Confidence level = 95%, αError rate = 5 % (one-sided), and power of study = 80%. Assuming the 20% functional difference between the results of long and short variants of PFN, the sample size is calculated with the help of an online sample size calculator that comes out to be 54 (27 in each group), which is approximated to 60 (30 in each group).
The individuals were informed about the examination procedure, and informed written consent was taken in local language from the patients before participation in the study. Patients who fulfilled the inclusion criteria were randomized into groups A and B using a computer-based table of random numbers, wherein the sequence of implants to be used was decided. To remove the selection and gender bias, I did block randomization with gender as a stratification factor.
Inclusion criteria:
-
1)
Skeletally mature patients of either sex
-
2)
Patients with intertrochanteric femur fractures belonging to group AO-31A1 and 31A2 according to the AO/OTA system of classification
Exclusion criteria:
-
1)
Pathological fracture
-
2)
Compound fracture
-
3)
Polytrauma patients and patients with I/L or C/L femoral shaft fractures
-
4)
Fractures falling into reverse oblique type 31A3
Data entry and analysis
All data was tabulated and then analyzed with appropriate statistical tools, ‘MedCalc.’ Mean, standard deviation and variance were calculated, and the following statistical significance tests were applied:
-
1)
‘Chi-square test’ and ‘Fisher’s exact test’ were used for the statistical significance test
-
2)
Test of significance for difference of proportions
-
3)
Student’s T-test was used as the statistical tool to test for the significance of observed mean differences
Differences were assessed using one-way analysis of variance (ANOVA). A pairwise comparison of one-way ANOVA was made using post hoc analysis and the student-Newman-Keuls Q-test. The corrected P-value was obtained directly, and the cut-off value was 0.05. Finally, the calculated value was compared with the tabulated value at a particular degree of freedom and finds the level of significance. A ‘p-value’ will be considered to be non-significant if >0.05 and significant if <0.05. The probability of error at 0.05 was considered significant, while at 0.01 and 0.001, as highly significant.
Methodology: On admission, a patient with a complaint of pain in the hip and unable to bear weight since the time of fall was evaluated and examined from head to toe. The affected side lower limb was immobilized by skin traction. After stabilization of the patient hemodynamically, an X-ray of the pelvis with both hips AP and involved hip with femur full-length AP and lateral view (wherever possible) was done. The fracture pattern was grouped according to classification/inclusion criteria. Routine blood investigations, chest X-ray, and electrocardiogram (ECG) (in necessary patients) were ordered. After getting pre-anesthetic clearance, patients were planned for operation on an elective basis. Informed consent was taken from patients and relatives for surgical intervention, part preparation was done and patients were kept fasting overnight.
Implant details
-
1)
Length of short PFN – 180–250 mm
-
2)
Length of long PFN – 320–420 mm
-
3)
Proximal diameter – 17 mm
-
4)
Distal diameter – 9,10,11,12 mm
-
5)
Neck-shaft angle – 135
-
6)
Proximal valgus angle – 6
Surgical intervention
All patients received injectable third-generation antibiotics 30 minutes before surgical incision. The patient was positioned in the supine position. The affected limb was adducted by 10–15 degrees. The unaffected leg [Figure 1 and 2] was flexed and widely abducted so as to position the C-arm in between the legs to get anterior-posterior and lateral views of the hip and femur. Closed reduction was attempted with traction and internal rotation, and if failed, then open reduction followed by internal fixation was done using either long or short PFN.

- Implant details.
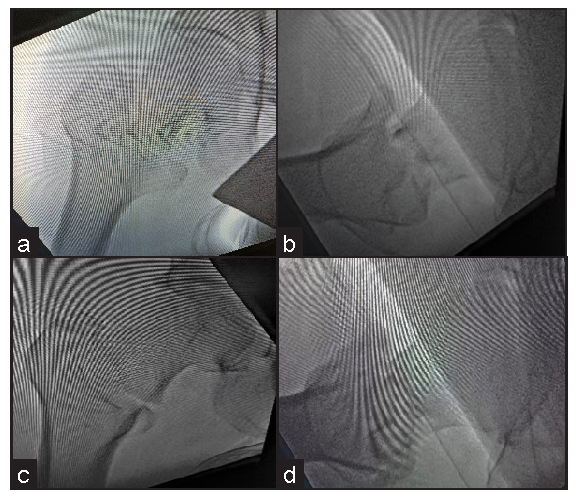
- (a,b) Pre-reduction xray, (c,d) Post-reduction xray.
Operative steps
After close reduction under C-arm guidance
Entry [Figure 3a and b] is taken just medial to the tip of the greater trochanter, a guide wire is inserted, and proximal reaming is done for accommodating the proximal larger diameter of PFN followed by insertion of the nail over a guide wire. Guidewire inserted for lag screw and hip pin [Figure 3c and d].

- (a,b) Entry taken just medial to tip of greater trochanter in AP view and centre in lateral view, (c,d) Guide pin for derotation screw and lag screw in inferior quadrant in AP view and centre in lateral view.
The guide wire for the lag screw should pass through the inferior quadrant supporting the calcar area, and the guide wire for the hip pin (derotation screw) should pass through the superior quadrant in AP view. Both wires should be in the center of the neck and head in lateral view [Figure 4]. For fracture unstable reduction is done using spike placed anteriorly and passing thick k wire anteriorly through neck [Figure 5].
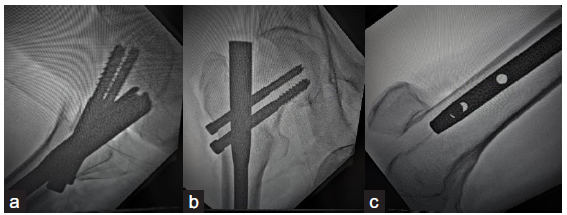
- Final placement of derotation and lag screws (a) Both hip screws in centre of head and neck in lateral view), (b) Lag screw in calcar area and derotation screw in superior quadrant, (c) distal dynamic locking bolt.

- (a,b) Close reduction of Unstable fractures using thick K wire and spike, (c,d) Fracture reduced by spike placed anteriorly and held with k wire passed anteriorly.
Postoperative protocol
All patients were given I/V antibiotics (1.5 gm cefoperazone + sulbactam and 500 mg Amikacin 12 hourly) for 24–48 hours and then shifted to oral. Patients were made to sit up in bed on the second postoperative day and static quadriceps exercise was started along with active knee bending, ankle and toe movement. On the second postoperative day, the dressing over the surgical wound was changed, and if found dry and healthy with no discharge, the patient was discharged.
Follow-up
Done on the 14th postoperative day for suture removal, weight bearing was commenced depending upon fracture stability and adequacy of fixation. Weight-bearing was delayed for unstable and osteoporotic-type fractures. All the patients were followed up on the 6th, 12th, and 24th week (one month, three months, and six months) to assess functional and radiological outcomes and compare between the two groups. Harris Hip Score (HHS) [Table 1] was used for functional outcome assessment, which included a questionnaire for about ten components:
-
1)
Pain
-
2)
Range of motion
-
3)
Limp
-
4)
Support
-
5)
Gait distance
-
6)
Stair climbing
-
7)
Ease of using footwear
-
8)
Sitting
-
9)
Public transport use
-
10)
Deformity
| Score | Rating |
|---|---|
| 90–100 | Excellent |
| 80–89 | Good |
| 70–79 | Fair |
| <70 | Poor |
A total score of 100 was allotted after summing scores for individual points.
At each follow-up, AP and lateral views radiograph were done to assess radiological outcome in terms of:
-
1)
Progression and time of union
-
2)
Z effect
-
3)
Reverse Z effect
-
4)
Implant breakage
-
5)
Peri-implant fracture
-
6)
Varus collapse
-
7)
Screw cut out
-
8)
Symptomatic back out of screw
HARRIS HIP SCORING
Illustrations of operated cases
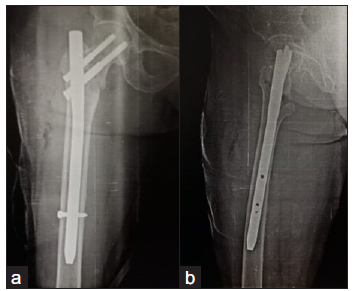
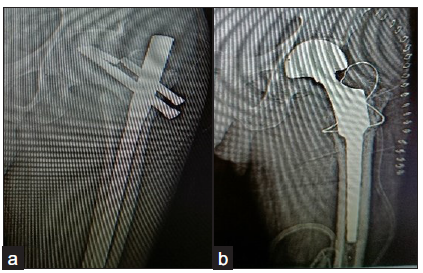
Case 1: A 65-year-old female patient with C/O right hip pain. Figure 6 showing Antero-posterior and lateral view of Intertrochanteric femur fracture.
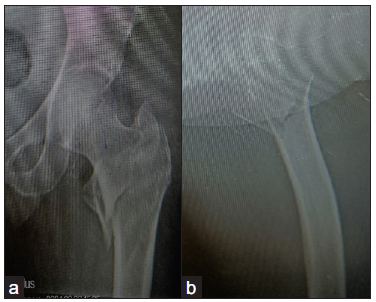
- AP and lateral views.
Figures 7 and 8 showing post-op follow up xrays at 3 and 6 months respectively depicting well formed callus on anteromedial aspect with positive reduction.
- Shows calllus formation on anteromedial aspect at 3 months.
- Well united fracture treated with long PFN at 6 months follow up.
Cases operated with short PFN
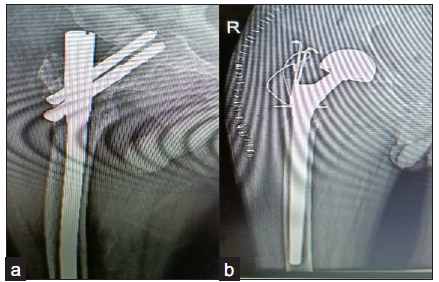
Case 1: A 70-year-old male patient [Figure 9] with diabetes mellitus as a comorbidity was admitted with a history of slips and falls at home. Patient was operated with Short PFN and fracture was well united as seen in Figures 10 and 11 at 3 and 6 months follow-up respectively.

- Preoperative X-ray.
- Well formed callus at 3 months in AP and lateral view.
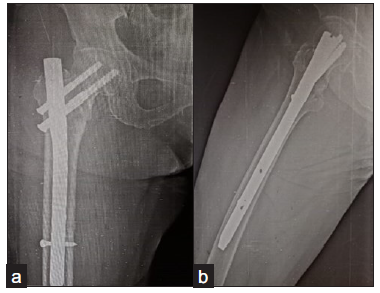
- AP and lateral views showing united fracture.
RESULTS
In our study of over 60 patients, 30 were treated with short proximal femoral nailing, and the other 30 were treated with long proximal femoral nailing.
The most common age group in studied patients was 60–65 years, that is, 8 and 9 (26.67% and 30.00%) in short PFN and long PFN, respectively [Table 2].
| Age distribution in years | Number of patients | |
|---|---|---|
| Short PFN | Long PFN | |
| 50–59 | 7 | 6 |
| 60–65 | 8 | 9 |
| 66–70 | 8 | 8 |
| 71–75 | 7 | 7 |
| Total | 30 | 30 |
PFN- Proximal femoral nail
The most common mode of injury was trivial fall, that is, 39 (65%) [Table 3].
| Mechanism of injury | Number of cases | Percentage |
|---|---|---|
| Road traffic accidents | 9 | 15.00 |
| Fall from height | 12 | 20.00 |
| Trivial fall | 39 | 65.00 |
Functional outcome
Mean HHS score in AO-31A1 type IT# after 6, 12, 16, and 24 weeks for short PFN and long PFN was 76.23 and 74.90, 81.15 and 82.96, 85.67 and 86.59 and 89.63 and 90.56, respectively.
Mean HHS score in AO-31A2 type IT # after 6, 12, 16, and 24 weeks for short PFN and long PFN was 76.03 and 74.55, 80.94 and 81.60, 82.89 and 84.11 and 88.63 and 89.16, respectively.
Radiological outcomes
The mean radiological time to union (in weeks) for short PFN and long PFN was 16.4 and 17 weeks, respectively.
Complications
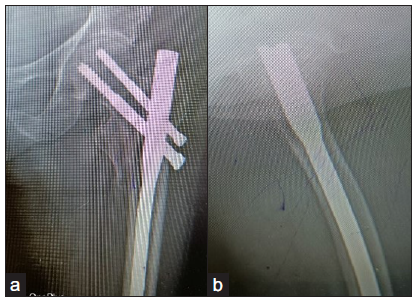
There was one case os screw backout which was treated with repositioning of both screws with washer [Figure 12a and b]. One patient came with varus collapse with broken implant in which implant was removed and long calcar supporting stem hemiarthroplasty was done [Figure 13a and b]. There was One case of varus collapse with screw cut out [Figure 14a and b] and other case of varus collapse with screw cut through [Figure 15a and b].
- Showing implant back out reoperated with exchange screws.
- (a) Varus collapse at 3 months follow up with broken implant, (b) Reoperated with implant removal with calcar supporting lonfg stem modular hemiarthroplasty.
- (a) Follow up xray at 3 months showing varus collapse with screw cutout, (b) Implant removal with long diaphyseal modular hemiarthroplasty.
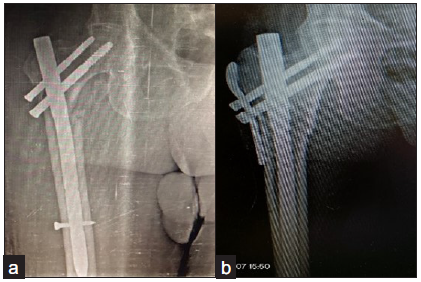
- (a) Varus collapse with screw cut out at 3 months follow up, (b) Reoperated with Long PFN with Trochanteric stabilization plate.
So the complication rate found in group A treated with short PFN was 13.33%, that is, 4 out of 30 cases, whereas in group B, it was 5 out of 30, that is, 16.66% [Table 4].
| Complication | Type of Fixation | |
|---|---|---|
| Short PFN | Long PFN | |
| Anterior thigh pain | 1 | 0 |
| Peri-implant fractures | 0 | 0 |
| Z effect | 0 | 0 |
| Reverse Z effect | 0 | 1 |
| Varus collapse with a screw cut through | 0 | 1 |
| Screw back out | 2 | 2 |
| Infection | 1 | 1 |
PFN- Proximal femoral nail.
Among 60 cases, 22 patients belonged to AO type 31 A1 and 38 patients belonged to AO-31A2 [Table 5]. The duration of surgery was 71.4 minutes for short PFN and 90.6 minutes for long PFN [Table 6].
| Type of fracture | Number of cases | Percentage |
|---|---|---|
| AO-31A1 | 22 | 36.66 |
| AO-31A2 | 38 | 63.33 |
AO: Arbeitsgemeinschaft für Osteosynthesefragen, OTA: Orthopaedic trauma assosciation.
| Short PFN | Long PFN | |
|---|---|---|
| Duration of surgery (minutes) | 71.4 | 90.6 |
PFN: Proximal femoral nail.
DISCUSSION
The primary treatment goal for intertrochanteric fractures is to achieve stable fracture fixation and make the patient ambulatory, followed by restoration of the patient to their pre-injury stage so as to avoid complications related to prolonged immobilization like bed sores.
In our study, the most common age group was 60–65 years, that is, 26.67% and 30.00%, in short PFN and long PFN, respectively. In the study conducted by Y Zhang,[4] the average patient’s age was 74.83 years. So this was due to the fact that increasing age increases the frequency of fractures, the cause being osteoporosis.
The most common mode of injury in this study was trivial fall, that is, 39 (65%). Similar results were given by Siva Mahesh et al.[5] They concluded that the leading cause of fracture was a trivial fall in 84.27% of cases.
The mean duration of surgery was 71.4 minutes for short PFN and 90.6 minutes for long PFN. Results were similar to the study conducted by Christopher Boone et al.[6], where the average operative time was found to be significantly greater (P < 0.001) for long (56.8 ± 19.4 minutes) than for short (44.0 ± 10.7 minutes) intramedullary nail procedures. Chinmoy Das et al.[7] also found a significant difference in the operative duration of short PFN as compared to long PFN, where the former had a lesser duration.
The results obtained while analyzing the functional outcome of both groups were comparable, finding no statistically significant difference (p > 0.05) between the two modes of treatment. There is evidence suggesting that intertrochanteric femur fractures with subtrochanteric extension are best treated with long PFN.
Similarly, the study conducted by K Rahman MA[8] showed that the average Harris Hip Score at final follow-up in Group A was 81.0 ± 11.62 and in Group B 80.3 ± 10.83, which concluded that irrespective of length, PFN is an efficient method for fixation of intertrochanteric femur fractures. Similarly, the study conducted by Chinmoy Das et al.[7] concluded that both short and long PFN can be efficiently used for unstable intertrochanteric femur fracture.
In this study, the mean radiological time to union (in weeks) for short PFN and long PFN was 16.4 and 17 weeks, respectively. In the study conducted by K Rahman MA,[8] the average time of union in Group A (short PFN) was 15.69 ± 2.72 weeks, while that of Group B (long PFN) was 15.77 ± 2.05 weeks.
In another study done by Xue-Feng Guo,[9] the average healing time of the long nail group was (6.5 ± 3.1) months, and the short nail group was (6.8 ± 3.7) months, revealing no significant differences (p = 0.09).
Complication Rate
There was no significant difference in complication rate observed in the group treated with short PFN as compared to that treated with long PFN.
CONCLUSION
This is a prospective type of study that compares functional and radiological outcomes of long and short PFN in treating stable and unstable intertrochanteric femur fractures of type AO/OTA 31A1 and 31A2. Both long and short PFN provide comparable functional outcomes; this was calculated in terms of Harris Hip Score, which was not statically significant for both groups (p-value> 0.5).
Neither of the groups showed any significant difference in the meantime of radiological union. However, there was a significant difference found in the operative duration of the short PFN over the long PFN in terms of decreased operative time of the former, thus decreasing C-arm time and number of radiological exposures. In patients with nail curve and femoral bow mismatch, short PFN should be preferred to avoid perforation of the anterior cortex. In older patients with significant osteoporosis, it’s more advisable to use long PFN as it splints the entire length of diaphysis preventing stress riser and incidence of anterior thigh pain. In terms of complication rate, results of both short and long PFN were comparable. Longer follow-up and larger sample size could better explain the long-term outcomes of both long and short PFN.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Rockwood and Green’s Fractures in Adults. Philadelphia (PA): Wolters Kluwer Health; 2015. p. :2076.
- A Prospective Study of the Functional Outcome of Intertrochanteric Femoral Fracture Managed with Short Proximal Femoral Nail. Int J Contemp Med Res. 2020;7:B9-16.
- [CrossRef] [Google Scholar]
- Short Versus Long Cephalomedullary Nails for Pertrochanteric Hip Fracture. Orthopedics. 2017;40:83-8.
- [CrossRef] [PubMed] [Google Scholar]
- Long and Short Intramedullary Nails for Fixation of Intertrochanteric Femur Fractures (OTA 31-A1, A2 and A3): A Systematic Review and Meta-analysis. Orthop Traumatol Surg Res. 2017;103:685-90.
- [CrossRef] [PubMed] [Google Scholar]
- Long Versus Short Twin-screw integrated Cephalomedullary Nail (InterTAN) for the Surgical Management of Intertrochanteric Fractures of the Hip in Indians. Cureus. 2023;15:e45942.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Short Versus Long Intramedullary Nails for the Treatment of Intertrochanteric Femur Fractures (OTA 31-A1 and A2) J Orthop Trauma. 2014;28:e96-100.
- [CrossRef] [PubMed] [Google Scholar]
- Functional Outcome of Long Proximal Femoral Nail Versus Short Proximal Femoral Nail in Peri-trochanteric Fractures in the Elderly Patient. Int J Orthop Sur. 2022;30:49-52.
- [Google Scholar]
- Short Versus Long Proximal Femoral Nail in the Management of Intertrochanteric Fractures – A Comparative Study. Int J Burns Trauma. 2023;13:99-109.
- [PubMed] [PubMed Central] [Google Scholar]
- A Comparative Study of the Therapeutic Effect Between Long and Short Intramedullary Nails in the Treatment of Intertrochanteric Femur Fractures in the Elderly. Chin J Traumatol. 2015;18:332-5.
- [CrossRef] [PubMed] [Google Scholar]







