Translate this page into:
Adolescent Gynecological Surgeries: Cause for Concern
*Corresponding author: Monika Anant, MBBS, MS2C, room no 242, second floor, OPD Building, All India Institute of Medical Sciences (AIIMS) Patna, Phulwarisharif, Patna, Bihar, India. drmonika.anant@gmail.com
Abstract
Introduction
Gynecological surgery in adolescent girls (10–19 years) remains challenging due to remarkable differences in anatomy, physiology and need for fertility preserving conservative surgical approach. We aimed to identify the various gynecological causes, operative outcomes, and need for follow-up surgeries in adolescents.
Methods
A single-center hospital record-based retrospective study was conducted for gynecological surgeries performed on adolescents in a 5-year period with exclusion of obstetrical and nongynecological causes.
Results
Sixty-eight adolescents of mean age 16.77 ± 2.317 years underwent gynecological procedures wherein 63 (92.64%) were postmenarchal girls. Pain abdomen (75%), menstrual abnormality (47%), and abdominal swelling (47%) were their main complaints. Note that 35 (51.4%) surgeries performed were for adnexal masses and 24 (35.3%) for obstructive Mullerian anomalies or neovagina creation. Other indicated surgeries were uterine leiomyoma (4.4%), Bartholin’s cyst (5.8%), and pelvic abscess (1.4%). The mean interval of symptoms to the diagnosis was 1.22 ± 1.381 years while the mean diagnosis to surgery interval was 8.71 ± 5.880 days. A statistically significant difference (243.3 vs. 783.1 days, p < 0.00001) was found in the symptoms to diagnosis interval and the length of hospital stay (difference in means 16 days, p < 0.00001) in the two major operative groups. Minimal access surgery could be completed in 37% of cases. Complications encountered were bowel injury in 5.8%, bladder injury in 2.9%, blood transfusion requirement in 5.8%, and reoperation in 2.94%. Follow-up revealed one death, adjuvant chemotherapy in 7.3%, and suppressive hormone therapy for endometriosis in 13% of operated girls.
Conclusion
Diagnosis of a gynecological presentation is protracted and delayed in adolescents. Both diagnosis and surgery is challenging, and minimal invasive surgery is preferable. Malignancy diagnosis or exclusion, treatment, and follow-up should be prioritized to limit delays in the decision to treat. Timely and appropriate, as far as possible conservative surgery and adherence to follow-up protocols will ensure successful outcomes.
Keywords
Adolescent gynecology
Endoscopy (laparoscopy and hysteroscopy)
Germ cell tumors of the ovary
Mullerian anomalies/intersex
Surgery
Introduction
Adolescence marked by growth spurt, thelarche, adrenarche, and menarche in females is the transition phase from childhood to adulthood. World Health Organization defines adolescent age between 10 and 19 years, wherein early adolescence (10–14 years) has physical changes and body transformation, late adolescence is between 15 and 19 years.[1] The adolescent gynecological problems encountered are unique, involve meticulous diagnostic skills, and careful decision of treatment plan as future fertility is at stake.[2] The embarrassment about menstruation, fear of disease, and ignorance of available services delay presentation as well as consultation having valuable implications on quality of life and fertility.[3]
Adolescents seeking gynecological consultation commonly present with abdominopelvic pain and abnormal menstruation with causes ranging from physiological changes to complex conditions requiring surgical intervention.[4] Gynecological surgery poses a challenge of preserving reproductive organs and functions limiting the surgical exercise for a safe and conservative approach. A detailed parental counseling session with explicit consent is required.[5] As far as possible, use of minimally invasive techniques and fertility preservation should be attempted for faster recovery reducing school absenteeism, cosmesis, and reduced adhesion formation in pelvis.
This study aimed to identify various gynecological etiologies that required surgical intervention in adolescent females in our center, with the objective to identify the various causes of surgery and surgical outcomes and need for long-term follow-up in such patients.
Material and Methods
A retrospective hospital record-based study was conducted, after clearance from the Institutional Ethics Committee (AIIMS/Pat/IEC No.507:2020). The study was performed in the Department of Obstetrics and Gynecology, in a tertiary care center in Eastern India. The hospital records of patients in age group 10 to 19 years who underwent gynecological surgeries in a 5-year period of January 2015 to December 2019 were retrieved from file records of the medical record section.
Adolescents who were medically treated and those who underwent obstetrical and nongynecological surgeries were excluded from the study. The demographic details, clinical presentation, investigations, diagnosis, surgical procedure, and hospital stay of these adolescent patients were pooled from the medical records. The histopathological reports, management details, and surgical outcomes were also recorded. Relevant data from records were entered into a predesigned piloted form and follow-up course was evaluated on routine 4 weeks postoperative follow-up and also enquired telephonically.
The collected data was entered on Microsoft Excel sheets and Statistical Package for Social Sciences (SPSS) for Windows version 22.0 (SPSS Inc., Chicago, Illinois, United States) was used for the analysis and two-sided p-value of 0.05 is considered as significant for this study. The continuous variables were represented by mean ± standard deviation for normally distributed and frequencies for categorical variables. Chi-square or Fisher’s exact test was used as a test of significance (calculation of p-value) for comparing qualitative and Student’s t-test used for quantitative variables.
Results
This study included 68 adolescents between the age group 10 and 19 years who underwent invasive surgery for different gynecological conditions over the 5-year period. There were a total of 1,160 gynecological surgeries performed during this time period out of which 68 (5.8%) surgeries were performed on adolescents which included 6 (8.8%) minor and 62 (91.1%) major surgeries.
Mean age of the patients was 16.77 ± 2.317 years. Majority of the patients were in the late adolescent age group (16 to 19 years, 55.8%) and 44.11% were early adolescent. Note that 63 (92.64%) were postmenarchal girls and only 5 (7.3%) premenarchal. Only 76.47% of the young girls were literate.
The most common presenting complaint was pain abdomen (75%) followed by menstrual abnormality (47.05%) and lump abdomen (47.05%). Nausea, vomiting, and early satiety were mainly present in patients with malignant ovarian tumors seven (10.2%). Five (7.3%) patients had urinary retention, diagnosed with cryptomenorrhea, large ovarian cyst, and immature teratoma, and two patients had vaginal septum resulting in hematocolpos and causing urinary retention. Patients with Bartholin’s cyst complained of recurrent perineal lump in four (5.88%) [Figure 1].

- Frequency of cases according to presenting symptom.
The most frequent cause for invasive surgery was adnexal mass (51.4%, n = 35) of which seven (20%) were performed as a result of malignant ovarian tumor which comprised 10.2% of the total. Immature teratoma was the most common finding in histopathology. Rare single cases of rhabdomyosarcoma uterine cervix and pelvic abscess were also seen. Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome was the most common finding among Mullerian abnormalities (14.7%) where vaginoplasty using McIndoe technique was done.
It was seen that patients with adnexal mass mostly presented with pain and lump, followed by menstrual irregularity. While those with Mullerian anomalies presented with absent or irregular menstrual bleed, followed by pain and only one-fifth of these patients presented with distension or lump. These findings were significant. Very few patients with either adnexal mass or Mullerian anomaly (5 vs. 12%) presented with urinary retention [Table 1].
Clinical presentation |
n (%) |
p-value |
|
|---|---|---|---|
|
Adnexal mass n = 35 |
Mullerian anomaly n = 24 |
||
Pain |
29 (82.9) |
15 (62.5) |
0.078 |
Distension/Lump |
27 (77.1) |
5 (20.8) |
<0.00 |
Menstrual abnormality |
12 (34.3) |
17 (70.8) |
0.006 |
Urinary retention |
2 (5.7) |
3 (12.5) |
0.358 |
The initiation of symptom and time taken to diagnosis was noted and the mean symptom to diagnosis interval was of 1.22 ± 1.381 years. Most of the patients (36.76%) with adnexal mass presented within 1 year of onset of symptoms whereas patients with Mullerian anomaly presented late (> 1 year). Patients with fibroid uterus, Bartholin’s cyst, pelvic abscess, and rhabdomyosarcoma also presented late (> 1 year).
Mean diagnosis to surgery interval was 8.71 ± 5.880 days. Note that 73.52% of the patients underwent surgery within 7 days of the diagnosis of their condition. A single patient had delay of more than a month and underwent myomectomy after correction of anemia [Figure 2].

- Diagnosis to surgery interval.
There was a significant difference between symptoms to diagnosis interval in cases of adnexal mass (243.3 days) and Mullerian anomalies (783.1 days). However, the time gap between diagnosis and treatment was comparable for both the groups [Table 2].
Variables |
Mean (+ SD) |
Significance p < 0.05 |
|
|---|---|---|---|
|
Adnexal mass n = 35 |
Mullerian anomaly n = 24 |
||
Onset of symptoms to diagnosis |
243.3 (367.6) |
783.1 (434.9) |
<0.00001 |
Diagnosis to surgery |
7.9 (5.1) |
9.5 (1.3) |
0.267 |
Abbreviation: SD, standard deviation.
Ultrasonography could establish definitive diagnosis in almost all the cases (94.11%) except the clinically diagnosed four cases of Bartholin’s cyst. Adnexal masses not characterized as benign by ultrasonography required ovarian tumor markers and computerized tomography for distinguishing malignant from benign (n = 35). Magnetic resonance imaging (MRI) provided a complete overview of pelvic anatomy in cases of Mullerian abnormalities.
After decision for surgery, preoperative blood investigations, anesthesia checkup, and optimization of patient condition were done for all patients as per hospital protocol. General anesthesia was the preferred method (91.1%) in abdominal and minimal invasive surgeries and regional anesthesia for vaginal surgeries.
Laparoscopy (36.76% cases) was undertaken for benign cases except those with massive masses or suspected malignancy. Also, myomectomy for large uterine fibroid and pelvic abscess drainage with adhesiolysis was performed as open surgeries. For open surgeries (n = 17), nine (52.94%) had longitudinal incision whereas transverse in eight (47.05%) patients. Vaginal route for cases of MRKH, cryptomenorrhea, and vaginal stenosis surgery was done. Combined abdominopelvic route was required in two (2.9%) cases for excision of the uterine rudimentary horn along with vaginoplasty.
Blood transfusion was required in four patients (5.8%). Intraoperative bowel injury occurred in four (5.8%) patients; among them two had malignant ovarian tumor and severe adhesions were present, one patient during vaginoplasty, and another during pelvic abscess drainage and adhesiolysis. Bladder injury occurred in two (2.9%) patients, one with rhabdomyosarcoma uterine cervix where mass extended from uterine surface till bladder base and another in Turner mosaic with MRKH previously operated. Surgical site infection occurred in two (2.9%) patients.
Mean hospital stay after surgery was 9.19 ± 7.59 days. Maximum patients (42.64%) were discharged within 5 days of surgery. A comparison of hospital stay and follow-up treatment revealed four-fifths of patients with adnexal masses had hospital stay of < 7 days and advised hormonal treatment. However, patients with Mullerian anomaly had a longer hospital stay of 16 days (66%) for the vaginal mold change usually on seventh postoperative day. The difference in total hospital stay duration was found to be highly significant [Table 3].
Variables |
n (%) |
Significance |
|
|---|---|---|---|
|
Adnexal mass n = 35 |
Mullerian anomaly n = 24 |
||
Stay in hospital |
p < 0.00001a |
||
1 wk |
27 (79.4) |
2 (8.3) |
|
2 wk |
4 (11.8) |
16 (66.7) |
|
2–4 wk |
3 (8.8) |
5 (20.8) |
|
1–2 mo |
0 |
1 (4.2) |
|
Adolescents who underwent cystectomy for endometrioma (13.23%) were given suppressive hormonal treatment postsurgery. Two (2.94%) patients were reoperated for constriction rings in vaginoplasty group of patients. Out of seven adolescents who underwent surgery for malignant ovarian tumor, one died (19 years with serous cystadenocarcinoma), two had stage 1a dysgerminoma, and five (7.3%) needed chemotherapy (four with advanced stage tumor and one with rhabdomyosarcoma). A patient of McIndoe vaginoplasty underwent emergency hysterectomy for acute abdomen of hematometra in rudimentary uterine horn [Figure 3].
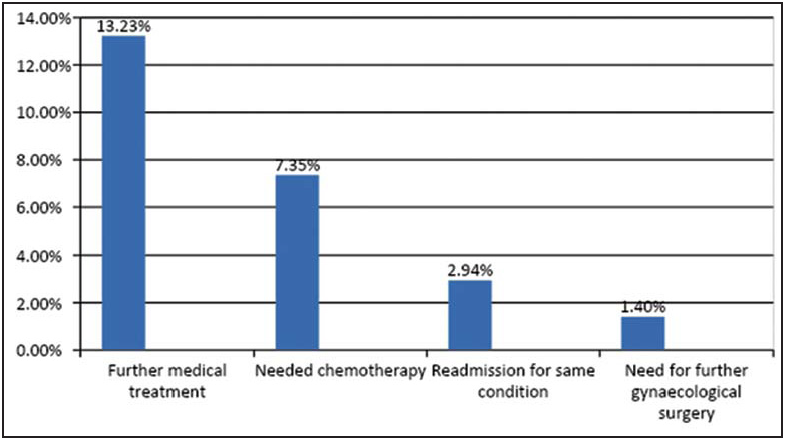
- Patient outcomes at follow-up.
Discussion
Gynecological surgery in an adolescent girl can be a life-changing event having deep impact physically as well as psychologically and having future implications for health, fertility, and cosmesis. The priority while formulating a plan for management should be toward fertility organ preserving approach, unlike the conventional aggressive approach earlier.
This study evaluated adolescents over a 5-year period reporting to the gynecological department, 7,865 adolescents visited the outpatient department of which 3.3% required hospitalization for surgery, 68 (0.86%) underwent surgeries for gynecological causes, and 196 (2.49%) for obstetrical causes.
The mean age of the patients was 16.77 ± 2.317 years and the majority (55.8%) was in the age group of 16 to 19 years. Out of these, 92.64% were postmenarchal adolescents which is similar to the reported mean age of 16 years and 87.5% being postmenarche.[4]
For this cohort the most common complaint was pain abdomen followed by menstrual abnormality and lump abdomen, while menstrual problems are the most common cause for consultation in outpatient in adolescents. Young patients with ovarian tumors have acute or chronic abdominal pain, nausea, vomiting, and increase of abdominal volume as reported by Mărginean et al.[6] which matches the presentation of patients with malignant ovarian tumors of this study. Although urinary retention is a rare symptom in young girls, five (7.3%) girls in this study presented with acute retention due to huge hematocolpos and hematometra. Two percent of all gynecologic visits per year are for symptomatic Bartholin’s cysts and abscesses,[7] whereas we found 5.88% patients in the present study with recurrent perineal lump/swelling due to Bartholin’s cyst, all of whom had early marriage and sexual activity.
The largest group for major surgery was found to be adnexal masses (35/68) of which malignant ovarian tumor comprised 10.2% cases which falls in the range of 4.9 to 13% rates of malignant and germ cell tumor in adolescent girls as reported by various studies.[8,9] Goals of surgical intervention were fertility sparing conservative surgeries improving symptoms and preserving future reproductive capacity.
Mullerian anomalies (35.29%) surgeries involved neovagina creation, excision of rudimentary uterine horn with functional endometrium, and severe pelvic endometriosis with pain symptoms. Accurate diagnosis of an obstructive genital anomaly early after menarche helps prevent unnecessary surgeries and infection-related complications. Prompt surgical correction resulted in relief of symptoms and reduced the risk of endometriosis.[10]
Among the rare conditions, a rhabdomyosarcoma uterine cervix and a pelvic abscess in sexually inactive girl were operated. Rhabdomyosarcoma cervix is the least common site for genitourinary tract rhabdomyosarcoma with a reported peak incidence in 14 to 18 years age for the embryonal type.[11] Pelvic inflammatory disease and other tubo-ovarian abscesses are infections typically transmitted sexually, but few have reported nonsexually transmitted tubo-ovarian abscesses in adolescents. Fei et al have reported that majority of tubo-ovarian abscess in nonsexually active adolescent girls require surgical treatment.[12]
Diagnosis of gynecological conditions are late or missed in adolescents due to nonspecific complaints, low index of suspicion, and considering the more common, acute abdomen conditions mimicking adnexal causes. In this cohort of adolescents, presentation was late with a long symptom to diagnosis interval (1.22 ± 1.381 years); however, once diagnosis was made, the surgical plan was swiftly executed, so the mean diagnosis to surgery interval was short (8.71 ± 5.880 days). Three-fourths (73.52%) patients underwent surgery within 7 days of the diagnosis. Ovarian torsion due to mature teratoma was the complication for which most emergency intervention was undertaken, all the more important in the adolescent age group as the delay in intervention can cause permanent ovarian damage with an impact on future fertility.[7] According to American College of Obstetricians and Gynecologists (2019), the most common ovarian pathologies found in adolescents with adnexal torsion are benign functional ovarian cysts and benign teratomas.[13]
Transabdominal ultrasonography, lacking ionizing radiation is the initial imaging modality of choice in children and adolescents, which established diagnosis in 94.11% of patients in this study, easily distinguishing benign cysts, from solid or complex masses. MRI becomes the gold standard imaging modality to differentiate soft tissue boundaries in Mullerian anomalies and a high degree of agreement (90.9%) of MRI and surgical findings has been reported.[14]
Assay of serum ovarian tumor markers, even negative, do not exclude the possibility of malignancy as the markers are positive in only 54% of cases.[15] In this study two patients had elevated cancer antigen-125 who were diagnosed with serous cystadenocarcinoma, three patients of immature teratoma had normal tumor markers, and two patients of dysgerminoma had elevated lactate dehydrogenase and β-human chorionic gonadotropin.
Minimal access surgery in adolescents should be performed by highly competent surgeons, particularly when complex congenital anomalies or advanced endometriosis is suspected.[16,17] Among open surgeries, a suprapubic transverse incision is advantaged by lower postoperative pain, less risk of long-term hernia complications, and better cosmesis. However, massive abdominopelvic masses and suspected malignancy do require longer midline longitudinal incisions for complete exploration.
Majority of the patients in this cohort had a favorable outcome with an uneventful recovery with certain conditions requiring follow-up therapy for endometriosis, germ cell tumors, and Mullerian anomalies. Endometriosis requires long-term postoperative medical therapy[18] for suppression of disease progression achieved by combined or progesterone-only contraceptive pills or gonadotropin releasing agonist injections with progesterone add back therapy for refractory cases. Note that 13.23% endometriosis patients provided with progesterone hormonal therapy are doing well after 1-year follow-up. Four adolescent girls requiring chemotherapy for ovarian germ cell tumors and one for rhabdomyosarcoma cervix are currently in follow-up. Patients with obstructive Mullerian anomalies, who underwent vaginoplasty, were followed up regularly for evaluation of patency of the vaginal canal and resumption of regular menstrual cycles. Repeat admissions were required for a few for failure to dilate, restenosis, and vaginal constriction ring, which are well-documented complications. Patients with failed vaginal dilatation present a difficult surgical challenge, may be undertaken for relaxing incisions, Z-plasty, or graft placement.[19] Even hysterectomy and adnexectomy are sometimes required for severe obstructive symptoms making these the most challenging gynecological surgeries performed in adolescent girls.
The importance of this study lies in the complete evaluation of the 5-year period including all causes of invasive gynecologic surgery in adolescent girls. The immediate surgical outcomes and follow-up management have also been included in this review. However, the authors feel that as it is a single-center study with a small sample size, the results may not be generalizable to the whole population.
Gynecological surgeries in adolescents have remarkable differences in anatomy, physiology, and surgical techniques compared with adults. For ideal outcomes, a multidisciplinary team of gynecologists, endocrinologists, endoscopists, fertility experts, pediatricians, oncologists, as well as parents is necessary. The treatment should not end at surgery but a proper scheduled follow-up till adulthood or even later till child-bearing should be a part of a comprehensive management plan.
Acknowledgment
None.
Conflict of interest
None declared.
Disclaimers, if any
None.
References
- Adolescent gynaecology problems in rural South India: a review of hospital admission in a tertiary care teaching hospital in Ammapettai, Tamil Nadu, India. Int J Reprod Contracept Obstet Gynecol. 2017;6:1920-3.
- [Google Scholar]
- Pediatric gynecology: assessment strategies and common problems. Semin Reprod Med. 2003;21:329-38.
- [CrossRef] [PubMed] [Google Scholar]
- Gynecological problems of adolescent girls attending outpatient department at tertiary care center with evaluation of cases of puberty menorrhagia requiring hospitalization. J Obstet Gynaecol India. 2016;66:400-6.
- [CrossRef] [PubMed] [Google Scholar]
- Laparoscopic approach to adnexal mass in adolescents: a retrospective analysis. J Datta Meghe Inst Med Sci Univ. 2017;12:55-60.
- [Google Scholar]
- Gynecologic surgery in the pediatric and adolescent populations: review of perioperative and operative considerations. J Minim Invasive Gynecol. 2016;23:1033-9.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric ovarian tumors, a challenge for pediatrician and gynecologist: three case reports (CARE compliant) Medicine (Baltimore). 2019;98:e15242.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The Bartholin gland cyst: past, present, and future. J Low Genit Tract Dis. 2004;8:195-204.
- [CrossRef] [PubMed] [Google Scholar]
- Ovarian tumors in children and adolescents–a clinical study of 52 patients in a university hospital. J Pediatr Adolesc Gynecol. 2011;24:25-8.
- [CrossRef] [PubMed] [Google Scholar]
- Adnexal mass requiring surgical intervention in adolescent girls. Eur J Gen Med. 2015;12:239-43.
- [Google Scholar]
- Mullerian anomalies in the pediatric and adolescent population: diagnosis, counselling and treatment options. Ann Infert Rep Endocrin.. 2019;2:1016.
- [Google Scholar]
- Embryonal rhabdomyosarcoma of the uterine cervix: a report of 14 cases and a discussion of its unusual clinicopathological associations. Mod Pathol. 2012;25:602-14.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Tubo-ovarian abscess in non-sexually active adolescent girls: a case series and literature review. J Pediatr Adolesc Gynecol. 2021;34:328-33.
- [CrossRef] [PubMed] [Google Scholar]
- Adnexal Torsion in Adolescents: ACOG Committee Opinion No, 783 Summary. Obstet Gynecol. 2019;134:435-6.
- [CrossRef] [PubMed] [Google Scholar]
- The utility of ultrasound and magnetic resonance imaging versus surgery for the characterization of Müllerian anomalies in the pediatric and adolescent population. J Pediatr Adolesc Gynecol. 2012;25:181-4.
- [CrossRef] [PubMed] [Google Scholar]
- Review of ovarian tumors in children and adolescents: radiologic-pathologic correlation. Radiographics. 2014;34:2039-55.
- [CrossRef] [PubMed] [Google Scholar]
- Minimal access surgery in adolescent gynaecology. BJOG. 2009;116:214-9.
- [CrossRef] [PubMed] [Google Scholar]
- Endometriosis in adolescents. JSLS. 2015;19:e2015.00019.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Management of postoperative vaginal stenosis with osmotic dilatation. J Pediatr Adolesc Gynecol. 2013;26:e64.
- [Google Scholar]








