Translate this page into:
Comparison of Ultrasonography and Fine Needle Aspiration Cytology in the Diagnosis of Malignant Breast Lesions in a Rural Setup
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
How to cite this article: Kalwani R, Kher KS, Daftari SS. Comparison of Ultrasonography and Fine Needle Aspiration Cytology in the Diagnosis of Malignant Breast Lesions in a Rural Setup. Int J Recent Surg Med Sci 2016;2(2):58-65.
Abstract
Introduction:
Breast cancer is the most common cancer diagnosed in women worldwide. These rising trends have emphasized the need of prompt detection, effective clinical evaluation, and exact diagnosis of the breast disease.
Aim:
To analyze and compare the sensitivity, specificity, and predictive values and accuracy of ultrasonography (USG) and fine needle aspiration cytology (FNAC) in diagnosing malignant breast lump.
Materials and methods:
A cross-sectional, prospective study was done. One hundred sixteen female patients attending surgery department with breast lump were included. After complete clinical evaluation of the lump, all patients underwent USG and FNAC examination for diagnosis of the lump, and further subjected to excisional biopsy/definitive surgery, the results of which were further compared with the histopathological results to determine the accuracy, sensitivity, specificity, and predictive values of FNAC and USG.
Results:
Out of 116, 61 (52.58%) benign lesions were found while the remaining 55 (47.41%) resulted to be malignant lesions on histopathological examination (HPE). Ultrasonography reported 46 true positive, 60 true negative, and 4 false negative cases with 6 inconclusive reports; whereas, FNAC reported 47 true positive, 61 true negative, and 6 false negative cases with 2 inconclusive reports. There were no false positive cases detected by USG and FNAC. Thus, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and diagnostic accuracy for USG was found to be 92, 100, 100, 93.75, and 96.36% (χ2-value = 94.88, p-value = 0.0001,S) and values of 88.68, 100, 100, 91.04, and 94.73% were obtained for FNAC respectively (χ2-value = 92.04, p = 0.0001,S).
Conclusion:
In diagnosing malignant breast lesion, USG and FNAC are 100% specific. Although USG appears more sensitive than FNAC, the percentage of indeterminate report is higher with USG.
Keywords
Breast cancer
Breast lump
Diagnostic accuracy
Fine needle aspiration cytology
Ultrasonography
INTRODUCTION
Breast cancer is the most common cancer affecting women worldwide.1 In females, it is the second most common cause of cancer-related deaths after lung cancer. The age-adjusted incidence rates ranges from 6.2 to 39.5 per 100,000 Indian women.2 With growing awareness of breast cancer in the general population, a lump in the breast causes great physical, emotional, and psychological trauma to the patient and family members. Therefore, a distinction of benign from malignant is of paramount importance for patient and proper management.3
A definitive diagnosis of benign lesion not only saves the patient from unnecessary stress, but also relieves the health services from undue burden. On the contrary, a definitive preoperative diagnosis of malignant lesion provides many opportunities for patient's counseling and planning of possible single-stage surgical treatment.3
Cancer of the breast can present either as a lump or a nipple discharge.4 Evaluation of this breast lump involves the rational use of a detailed history, clinical breast examination, imaging modalities, and tissue diagnosis, i.e., TRIPPLE ASSESSMENT.5 Although final diagnosis is made by the histopathological examination (HPE) of the excised specimen, the routine excision of all breast lumps would not be rationale, because as much as 80% of the breast lumps are benign.6 Thus, there is a need to utilize a less-invasive and cost-effective method, which is accurate, easier to apply, reproducible, valid, and must not require much of preparation to diagnose the lump, without resorting to a more painful and invasive open biopsy method.4 Presently, a wide range of diagnostic modalities are available for the breast lump evaluation. This includes ultrasound Doppler scanning, fine needle aspiration cytology (FNAC), mammography (MMG), and recently, magnetic resonance imaging (MRI) and contrast-enhanced ultrasound.3 However, due to the higher cost of MMG and MRI and their limited availability, not all patients can benefit from this. This suggested the preferred use of less expensive and affordable diagnostic tools like FNAC and ultrasonography (USG).
Ultrasound imaging of the breast is another technique for evaluation of the breast lumps with the advantages like no radiation exposure, noninvasive, high accuracy in diagnosing cystic lesions with more accuracy in the breast with dense parenchymal tissue, but it is an operator-dependent technique and hence some interobserver variations may exist.7
Fine needle aspiration cytology is a simple, reliable, valid, and reproducible tool for evaluation. It is even less traumatic and virtually painless procedure with no requirement of anesthesia, giving high percentage of true positive results, thus making it patient-friendly standard tool for diagnosis in breast lumps.3,8
Although the accuracies of FNAC and USG in the diagnosis of breast lumps have been tested individually in many studies, yet there is a dearth of literature in comparison of the two modalities for evaluation of the same. Thus this study was proposed to evaluate and compare the accuracy of USG and FNAC in the diagnosis of newly detected palpable breast lump in comparison to the final HPE report of the biopsied specimens.
MATERIALS AND METHODS
A prospective, cross-sectional study was conducted in indoor patients of the department of General Surgery, Acharya Vinoba Bhave Rural Hospital (AVBRH), Sawangi, who presented with clinically palpable breast lump. Recurrent lump at the same site of any previous operation and history of prior irradiation to chest or breast were excluded. Cystic breast lesions diagnosed clinically or by USG, and breast abscess presenting as lump and yielding pus on aspiration were also excluded, as such lesions were managed by aspiration or incision and drainage and were not excised.
Prior, the Institutional Ethical Committee clearance was taken and informed consent of all patients were obtained. Totally, 116 patients were enrolled in the study. They underwent routine clinical evaluation and then investigated by USG and FNAC and further subjected to excisional biopsy/definitive surgery. The specimen obtained was sent for HPE.
Clinical evaluation included the patient's demographic details, reproductive history, history of breast diseases, and physical examination of the lump followed by diagnostic evaluation.
Ultrasonographic evaluation at the Department of Radiodiagnosis, AVBRH, using 7.5 MHz probe (ALOKA ProSound Alpha-7) was performed by an eminent radiologist who had 10 years' experience in breast ultrasound.
The reports were grouped into four categories for easy analysis as benign, indeterminate, malignant, and normal breast.
The cases were then sent to Aspiration Cytology room, Pathology Outpatient Department, Datta Meghe Institute of Medical Sciences (DMIMS), Wardha, India, for FNAC examination of breast lump. Aspiration was done using disposable 23 gauge needle and 20cc syringe mounted on a suitable holder. Reports were collected and grouped into four categories as benign, malignant, indeterminate, and inadequate sample.
Further, all the breast lumps underwent excisional biopsy/definitive surgery and the specimens were sent in formalin solution for HPE at the Department of Pathology, DMIMS, India. The reports were grouped into benign and malignant for analysis. The final histopathological report was taken as the gold standard and data was analyzed to determine the specificity, sensitivity, predictive values, and diagnostic accuracy of FNAC and USG.
Analysis was done using descriptive and inferential statistics with chi-square test [Statistical Package for the Social Sciences (SPSS) software 17.0 version] and p < 0.05 was considered as the level of significance.
OBSERVATIONS AND RESULTS
Demographic Profile
A total of 116 female patients with 116 breast lumps were included in the study. Out of the total of 116 patients, the HPE being gold standard revealed 61 patients (52.58%) who had benign breast disease whereas 55 patients (47.41%) were found to have malignant breast lump. The age range in malignant cases was found to be 26 to 75 years with the mean age of 51.25 ± 11.40 years and the maximum no. of malignant cases were found in the 5th decade followed by 6th decade (p < 0.05). The maximum number of cases were of Hindu religion followed by Muslims with no Christian patient (p > 0.05). Among 55 malignant cases, 54 (98.18%) were multipara and only 1 case (1.82%) was nullipara.
Out of the total of 55 malignant females, 40 (72.72%) were from the rural areas and 15 (27.27%) were from the urban cities. We found that 72% (n = 29 out of 40) of the breast cancer patients that were from the rural areas had consulted the clinician after a delay of >6 months on the self-detection of lump. Whereas approximately 70% (n = 11 out of 15) of the malignant cases that were from urban cities had consulted the clinician within the 15 days of noticing the lump.
On examining the location of lump, we found that the maximum number of lumps, i.e., 47.41% were found in the upper-outer quadrant (p < 0.05). On examining the size of lump, we found that 56.36% of the malignant cases (n = 31) that presented to us had the size corresponding to that of T3 stage (>5 cm) whereas 41.82% (n = 23) cases had a lump size corresponding to that of T2 stage (2-≤ 5 cm) with the overall average size of lump being 5.36 ± 2.93 cm. Among the malignant patients who had presented within 6 months, 64% of them had the lump size of T2 stage, with 32% had size of T3 stage, whereas in the group of malignant patients who had presented after 6 months, 76.67% of them had already reached the lump size of T3 stage, with 23.33% had size of T2 stage (p < 0.05) (Table 1).
| Delay in the presentation of lump | Size of malignant lump at the time of presentation | |||
|---|---|---|---|---|
| ≤2 cm | 2 to ≤5 cm | >5 cm | Total | |
| <6 months | 1(4%) | 16 (64%) | 8 (32%) | 25 (45.45%) |
| >6 months | 0 | 7 (23.33%) | 23 (76.67%) | 30 (54.54%) |
| Total | 1(1.8%) | 23 (41.81%) | 31 (56.36%) | 55 (100%) |
Results of Histopathology
On examining the pathology of breast lumps after final histopathological results, we found that the most common pathology of breast lump was fibroadenoma (49.13%) followed by ductal carcinoma (43.96%), then followed by fibroadenosis (2.5%) and then each of metaplastic carcinoma, medullary carcinoma, papillary carcinoma, stromal tumor, and subareolar hyperplasia as 0.86% (Table 2).
| Histopathological result | Total | |
|---|---|---|
| Benign | Fibroadenoma | 57 |
| Fibroadenosis | 3 | |
| Subareolar hyperplasia | 1 | |
| Total | 61 | |
| Malignant | Metaplastic carcinoma | 1 |
| Medullary carcinoma | 1 | |
| Papillary carcinoma | 1 | |
| Stromal tumor | 1 | |
| Invasive ductal carcinoma | 51 | |
| Total | 55 | |
Results of Ultrasonography
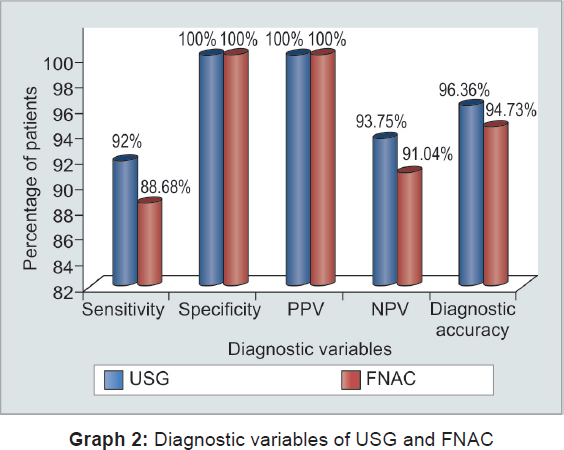
Out of a total of 116 breast lumps, USG had given 64 as benign, 46 as malignant, 6 as indeterminate with no normal breast finding report (Figs 1A and B). After comparing with the final histopathological reports (Table 3), we found that there were total 46 true positive and 60 true negative reports, whereas a total of 4 false negative with no false positive report was given by USG. There were totally 6 inconclusive or indeterminate cases reported by USG. The final results of USG (Graph 2) revealed the sensitivity as 92%, specificity as 100%, positive predictive value (PPV) of 100%, negative predictive value (NPV) of 93.75% with the overall diagnostic accuracy of 96.36% (p-value = 0.0001,S).

- Irregular, speculated, hypoechoic lesion with infiltrative margin (A), calcification (B). Ultrasonography reported this case as malignant lump. On HPE, it was confirmed as invasive ductal carcinoma
| Histopathological results | ||||
|---|---|---|---|---|
| Malignant | Benign | Total | ||
| USG (6 inconclusive reports) | Malignant | 46 | 0 | 46 |
| Benign | 4 | 4 | 64 | |
| Total | 50 | 60 | 110 | |
| USG in females <35 years | Malignant | 5 | 0 | 5 |
| Benign | 0 | 50 | 50 | |
| Total | 5 | 50 | 55 | |
| USG in females >35 years | Malignant | 41 | 0 | 41 |
| Benign | 4 | 10 | 14 | |
| Total | 45 | 10 | 55 | |
| FNAC (2 inconclusive reports) | Malignant | 47 | 0 | 47 |
| Benign | 6 | 61 | 67 | |
| Total | 53 | 61 | 114 | |
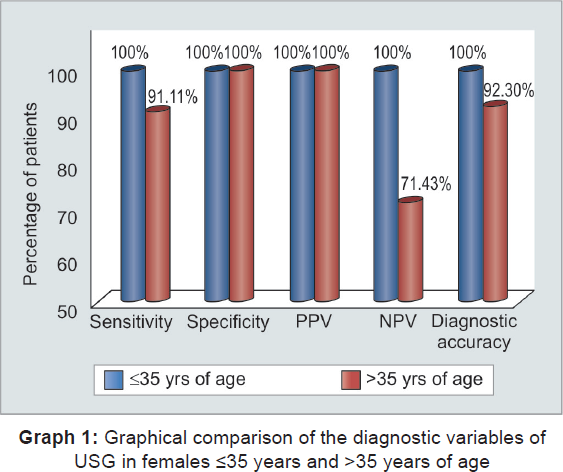
The USG reports were again analyzed based on the age by dividing the patients age groups into two of ≤35 years and >35 years, due to the difference in the diagnostic ability of USG in these two different breast densities (Graph 1). The result of USG was found better in these younger age group than the older patients, with all diagnostic variables: Sensitivity, specificity, PPV, NPV, and overall diagnostic accuracy found to be 100%, whereas in age group of more than 35 years, USG revealed sensitivity as 91.11%, specificity as 100%, PPV as 100%, NPV of 71.43% with the overall diagnostic accuracy of 92.30% (p-value = 0.0001,S).
Results of the Fine Needle Aspiration Cytology
Out of the total of 116 breast lumps examined, FNAC reported 67 (57.7%) breast lumps as benign and 47 (40.51%) cases as malignant (Fig. 2), with 1 case each of indeterminate report and inadequate sample. After comparing with the final histopathological reports (Table 3), we found that there were total 47 true positive and 61 true negative reports given by FNAC, with a total of 6 false negative and no false positive reports. There was only 1 indeterminate report and 1 case of inadequate sample given by FNAC. The final results of FNAC (Graph 2) revealed sensitivity of 88.68%, specificity of 100%, PPV of 100%, NPV of 91.04% with an overall diagnostic accuracy = 94.73% (p-value = 0.0001,S).

- Invasive ductal carcinoma (Cytopath, FNAC. 10×, Pap stain) shows discohesive malignant ductal cell sheets and ducts
Comparison of Results of USG and FNAC
Out of the total of 116 cases, there were only 16 cases, where differential reports or disparity were found between reports of USG and FNAC. A total of 6 false negative reports were given by FNAC in which the masses were reported as benign, but they were actually found malignant on final HPE. In all those 6 cases, USG could correctly diagnose them as malignant. There were a total of 4 false negative reports by USG, in which USG had suggested them as benign but they were found malignant on HPE. Out of those 4 cases, 2 were correctly diagnosed by FNAC as malignant. And in the rest of 2 false negative reports by USG, FNAC was inconclusive in diagnosing the condition. In other words, we can say that the 2 cases where FNAC was inconclusive in diagnosing the breast lump were also wrongly diagnosed by USG. There were total 6 indeterminate reports given by USG, which were correctly diagnosed by FNAC as 5 malignant and 1 benign condition and which was confirmed in HPE.
DISCUSSION
Carcinoma breast continues to be a major threat to women's health worldwide. However, its incidence differs significantly between developed and underdeveloped countries. In the course of diagnosis of a disease, the clinical evaluation is always followed by the reports derived from reliable investigation tools to strengthen the accuracy of the clinical diagnostic skill. Thus, this study aimed to determine the diagnostic accuracy of the two main tools of diagnosis of lump in breast, i.e., USG and FNAC and is discussed below.
Age
In our study, the mean age of malignant cases was 51.25 ± 11.40 years and the peak incidence was found in 5th decade of life followed by 6th decade. Our findings are in agreement with the data of National Cancer Registry Program (1996) of Indian Council of Medical Research (ICMR) who reported the average age of females with breast cancer to be 51 to 53 years.9
Religion
According to the National Cancer Registry Program (1996) in India in Mumbai, breast cancer incidence rates are highest among Parsis and Christians and lowest among Jains and Buddhists.10 The possible reasons for high breast cancer incidence in the Parsi community are their westernized lifestyle, consanguineous marriages, and late age of marriage and childbirth.2 However in our study, majority of patients were Hindu followed by Muslims and with no Christian patient. This contrast finding may be due to the relatively lesser Christian population in the surrounding rural region.
Parity
In our study, out of 55 malignant patients, there was only 1 nullipara and the rest 54 multipara. This observation is not in accordance with previous studies by Kelsey et al11 and Lambe et al12 who stated that nulliparous women have a slightly higher risk of breast cancer.13
Side and Location of Lump
On examining the location of lump, we found that the upper outer quadrant was the commonest site of the lump in our study, comprising 47.41% of the total lumps in that quadrant. This was consistent with the findings of Takhellambam et al14, Farhath et al,15 and Hussain et al.16 These higher number of breast lumps in this quadrant of breast is due to the fact that there is relatively more amount of the epithelial tissue of breast in this quadrant.17
Delay in the Presentation of Lump and Its Outcome
The higher stage at presentation has a direct influence on the overall prognosis of the disease. More than half of the malignant cases, i.e., 56.36% that presented to us had already reached the lump size corresponding to that of T3 stage followed by 41.82% cases lump size corresponding to that of T2 stage. The average size of the malignant lump was found to be 5.36 ± 2.93 cm.
We also found that the patients with malignant breast lumps that were from rural areas, 72% of the them had consulted the clinician after a delay of more than 6 months when the disease has already progressed, whereas the patients that were from urban cities, 70% of them had consulted within the 15 days of noticing the lump. This was in accordance with the results of Mukherjee et al13 and Malik et al.18
This clearly shows that the patients from urban areas are more aware and cautious regarding the breast disease as they are presenting early in the course of disease whereas patients from rural areas are late presenters due to ignorance and unawareness. This substantial delay in the referral of patients from underprivileged, remote areas, where the patients continue to receive symptomatic treatment till the time that the disease becomes incurable, is due to the lack of proper screening program and inadequate and unequal distribution of the health care facilities in underdeveloped countries.19
Ultrasonography
In our study, the sensitivity and specificity of USG for diagnosing malignant breast lesion were found to be respectively, 92 and 100%, which seem to be in conformity with the sensitivity range of 67 to 97% and specificity range of 85.7 to 100% reported by the previous studies.14,20,21,22 These wide variations amongst different studies could be due to different methods of case selections, different resolution power of ultrasound equipment used, and due to the fact that ultrasound is an operator-dependent technique.
The sensitivity of 92% found in our result suggest that 8 out of 100 cases having malignant lesion would be missed if USG is solely used for the evaluation of breast lump. Hence, there is a need to seek for additional investigation to rule out the malignancy in a benign report of USG. We found a NPV of 93.75%, which means that if USG gives a negative result in a case, there are only 93.75% chances that the patient is not having the disease. 6.25% probability still exists of that case being a malignant one. This indicates that the negative USG result does not confirm that the patient is not having the malignancy.
However, in our study, 100% specificity and 100% PPV means that if USG gives a positive result (malignant report), it definitely means presence of the disease. It is because there were no false positive cases given by USG, and it can be considered almost diagnostic of malignancy.
When we considered the results of USG in younger age group (≤35 years of age), the sensitivity, specificity, PPV, and NPV of USG in the diagnosis of malignant breast mass were all 100% against the respective values of 91.11, 100, 100, and 71.43% when considering those >35 years of age. Also, the percentage of indeterminate results was less in younger age group, i.e., 1.8% vs 8.3%. This clearly shows the more accurate results of USG in younger patients. Similar results were obtained in the study done by Takhellambam et al.14
These lesser indeterminate reports in ≤35 years age group suggested that the chance of missing a lump was less in younger age group, indicating the accuracy of USG to be more in this group. This is because young patients usually have dense breasts with little intraparenchymal fat, therefore forming a distinct layer of subcutaneous and retromammary fat, sandwiching a compact layer of breast parenchymal tissue. On ultrasound, the normal breast parenchyma appears as a layer of light colored echoes, while the normal fat layer appears as a darker layer. Abnormal growth, be it solid or cystic, benign or malignant, stands out as a darker shadow inside the lighter background of breast parenchyma.23
However, when intramammary fat content increases in obese patients, or postmenopausal women, these appear as patchy dark shadows inside the breast parenchyma. Abnormal tumor growth may then become masked by such shadows on ultrasound.23
Fine Needle Aspiration Cytology
Fine needle aspiration cytology of breast lump is an accepted and established method to determine the nature of the lump and reduce the number of open breast biopsies. Moreover, FNAC has been found to have sensitivity ranging from 83 to 97.5% and specificity of more than 99%.4,8,14,16,24,25 In this study, sensitivity, specificity, PPV, and NPV of breast FNAC in the diagnosis of malignancy was 88.67, 100, 100, and 91.4% respectively, which was quite comparable to the findings of the other studies.8,14,26 These variations could be due to the different inclusion criteria of breast lump (like size, palpable, or nonpalpable) in different studies; inclusion of atypia/suspicious result as malignant in calculation of sensitivity in some studies; and exclusion of inadequate results in some studies.27
The sensitivity of FNAC as 88.67%, found in our result, suggests that 11 out of 100 cases having malignant lesion would be missed, if FNAC is solely used for the evaluation of breast lump. Thus, further additional investigation should be considered to completely rule out the malignancy if FNAC gives negative result. We found NPV of 91.04%, which means that if FNAC gives a negative result in a case, there are only 91.04% chances that the patient is not having the disease; 8.96% probability still exists of that case being a malignant one.
The reason for these false negative results could be lump related, such as small or deep lumps, acellular aspirates from very hard lumps, hemorrhagic aspirates from highly vascular tumors, and aspirates from cystic lumps or the sampling error. Sampling error can be minimized by proper localization and aspiration technique performed by experienced pathologist.3,28
A 100% specificity and 100% PPV result means that if FNAC gives a positive result (malignant report), it definitely means presence of the disease. It can be considered confirmatory and further treatment decision can be made solely on this report without any further additional diagnostic investigation. The conditions that have a risk of a false positive result are papillary lesions, atypical epithelial hyperplasia, regenerating epithelial atypia, and atypia of ductal epithelium in a cyst.2 In our study we had no false positive result by FNAC. Considering patients' comfort, lack of requirement of anesthesia, rapid analysis and reporting, reduced cost, and relatively less false positive results make FNAC an ideal initial diagnostic modality in breast lumps.
Comparison of FNAC vs USG
The overall diagnostic accuracy of USG was found to be higher than FNAC (96.36% vs 94.73%). These higher values for USG are due to the fact that in all the cases, USG procedure was done by a Senior Professor of Radiology having experience of 10 years in breast ultrasound. Secondly, these slightly higher results of USG do not reflect the number of inconclusive or indeterminate reports given by USG as they were not included in the calculation, which is a limiting factor with USG.
Thus, the above findings suggest that both the diagnostic tools equally contributes for the diagnosis of the breast lumps, and both the investigations are complimentary to each other.
The sensitivity and NPV of USG were higher than that of FNAC (92% vs 88.68% and 93.75% vs 91.04% respectively). However, the percentage of inconclusive result was higher with USG than with FNAC (5.17% vs 1.72%).
There are certain strong points in our study. First, the gold standard test taken in our study is the histopathological report, which is valid, reproducible, and has been accepted as the gold standard worldwide. For a good study, the reference test against which the diagnostic test is compared should be the gold standard. A very strong point, again of our study, is the fact that both radiologist and the cytopathologist performing the USG and FNAC respectively, belonged to the two different departments of the institute and hence they were blinded from each others' results and also from the final histopathological report. Nor, they were given any clinical impression about the lump.
There are certain limitations of our study. First, the indeterminate reports were excluded from the calculation of specificity and sensitivity. That is the reason, sensitivity and diagnostic accuracy of ultrasound were found higher than FNAC. And so, their calculated values did not reflect this limitation of USG against FNAC. Secondly, cystic lesions and abscess were excluded from the study as they were treated mainly by aspiration and drainage, and hence no tissue sample could be obtained for HPE. This selectiveness of cases may limit the generalization of the findings in clinical practice.
CONCLUSION
Cancer of the breast is a grave disease and it often presents as a lump in breast, and hence the evaluation of it is important with the motive to rule out malignancy. This requires thorough clinical examination with the rational use of imaging modality and tissue diagnosis. Ultrasound of the breast is an emerging, relatively inexpensive, more accessible, accurate, and dynamic tool in the assessment of palpable breast lumps without the risk of ionizing radiations. Though previously confined as an adjunct tool in breast imaging, now it seems to be an appropriate initial imaging test to avoid unnecessary interventions and patient discomfort. Ultrasound is an operator-dependent investigation and hence if it is done by an experienced sonologist, sensitivity of USG can reach equal to or even surpass the sensitivity of FNAC.
Although the specificity and PPVs of both the diagnostic tools in diagnosing malignant breast lump were found to be 100% in our study, thereby giving the inference that a positive (malignant) result of either test can solely form the treatment decision without additional diagnostic investigation. But practically, an image-based modality like USG, does not form the basis of any definitive surgery of a malignant condition. Hence, if clinical examination and USG are suggestive of malignancy, but FNAC gives a benign report, then we need to have confirmatory histological diagnosis before a definitive surgery.
Sensitivity, NPV, and the overall diagnostic accuracy of USG were found higher than FNAC but the number of inconclusive or indeterminate reports was also higher with USG. In addition, FNAC was able to diagnose the lump where USG was inconclusive and the USG could diagnose the case where FNAC was falsely negative. Hence, none of these modalities can replace each other and rather should be considered complimentary to each other.
Both of these modalities have individually shown very good results and can show a diagnostic accuracy up to 100% if applied combined along with the proper implication of clinical diagnosis. The exact place of these diagnostic tools in the evaluation of beast lump would depend on the expertise and availability of these modalities in a clinical setup and also on the age factor of patients along with the clinicians' degree of suspicion on the nature of lump.
Further advancement in the technique of both these procedures like FNAC under imaging guidance, addition of Doppler in USG may increase their accuracy.
RECOMMENDATIONS
Ultrasonography has proven its efficacy in all ages and especially dense breast and should be considered as the first line investigation for the evaluation of breast lump, especially in women under the age of 35 years. If the clinical diagnosis and USG results are concordant, then, i.e., practically diagnostic of malignancy. The USG has shown good accuracy in higher age females, and due to its relatively inexpensive cost, easy accessibility, with no risk of radiations, it can also be applied as a first line screening modality in higher age females in a developing country like India, where there is already a scarcity of mammographic facilities in the rural regions. However, more research and randomized controlled trials are needed to validate this finding.
On the contrary, FNAC has also shown very good diagnostic accuracy in diagnosing malignant breast disease, and it could also prove its accuracy in the cases where the USG findings were indeterminate or inconclusive. Hence, both the modalities were complimentary to each other. To reduce the false negative and inconclusive results of USG, it should be done by an experienced sonologist with addition of color Doppler as it significantly improves the diagnostic accuracy of ultrasound. To reduce the false negative results of FNAC, it should be done under USG guidance to precisely localize the solid suspected region and avoid inadequate sampling errors.
Thus, both the diagnostic tools individually have shown very good diagnostic ability and accuracy. Hence none of them can replace each other as both tools are complimentary to each other and if applied combined in the form of Triple Assessment, can show its diagnostic accuracy up to 100%.
Breast screening programs with awareness about breast cancer and the importance of the breast self-examination at age 40 and above should be conducted for early detection of breast lump, which then can be thoroughly evaluated to diagnose malignant lesion so as to decrease the mortality. Certainly, more studies are required, addressing these recent advancements, to precisely define the exact place of FNAC and USG in the management of breast lump.
Source of support:
Nil
ACKNOWLEDGMENT
Authors would like to acknowledge and dedicate this paper to their friend Dr Soni, Assistant Professor, Department of Cardiothoracic Physiotherapy for being their and constant strength and standing beside in all the research work of this paper.
Conflict of interest:
None.
REFERENCES
- Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127(12):2893-2917.
- [CrossRef] [PubMed] [Google Scholar]
- Breast cancer care in India: the current scenario and the challenges for the future. Breast Care (Basel). 2008;3(1):21-27.
- [CrossRef] [PubMed] [Google Scholar]
- Triple assessment as a preoperative diagnostic tool for breast cancer at Bugando Medical Centre in northwestern Tanzania. Tanzan J Health Res. 2013;15(4):223-229.
- [CrossRef] [PubMed] [Google Scholar]
- Role of fine needle aspiration cytology in diagnosis of breast lumps. Kathmandu Univ Med J. 2007;5(2):215-217.
- [CrossRef] [PubMed] [Google Scholar]
- The comparative accuracy of ultrasound and mammography in the detection of breast cancer. Med J Malaysia. 2014;69(2):79-85.
- [Google Scholar]
- Detection and evaluation of a palpable breast mass. Mayo Clin Proc. 2001;76(6):641-648.
- [CrossRef] [PubMed] [Google Scholar]
- The use of ultrasound in benign breast disorders. World J Surg. 1989;13(6):692-698.
- [CrossRef] [PubMed] [Google Scholar]
- Palpable breast lump: fine needle aspiration cytology v/s histopathology: a correlation of diagnostic accuracy. Int J Surg. 2009;18(1):1.
- [CrossRef] [Google Scholar]
- Consolidated report of the population based cancer registries 1990–1996. New Delhi: Indian Council of Medical Research; 2001.
- [Google Scholar]
- An epidemiological assessment of increasing incidence and trends in breast cancer in Mumbai and other sites in India, during the last two decades. Asian Pac J Cancer Prev. 2003;4(1):51-56.
- [Google Scholar]
- Reproductive factors and breast cancer. Epidemiol Rev. 1993;15(1):36-47.
- [CrossRef] [PubMed] [Google Scholar]
- Transient increase in the risk of breast cancer after giving birth. N Engl J Med. 1994;331(1):5-9.
- [CrossRef] [PubMed] [Google Scholar]
- Presentation and diagnostic accuracy of fine-needle aspiration cytology and ultrasonography in detecting breast cancer in tribal females of rural West Bengal. Arch Clin Exp Surg. 2015;4(3):142-147.
- [CrossRef] [Google Scholar]
- Comparison of ultrasonography and FNAC in the diagnosis of malignant breast lesions. J Clin Diagn Res. 2013;7(12):2847-2850.
- [Google Scholar]
- Diagnostic accuracy of FNAC in evaluation of breast lumps. J Med Sci Clin Res. 2016;4(2):9275-9279.
- [Google Scholar]
- Comparison of fine needle aspiration cytology with excision biopsy of breast lump. J Coll Physicians Surg Pak. 2005;15(4):211-214.
- [Google Scholar]
- The breast.Greenfield's surgery scientific principles and practice. (5). Philadelphia: Lippincott Williams & Wilkins; 2011. p. :1241-1281.
- [Google Scholar]
- Pattern of presentation and management of Ca breast in developing countries. There is a lot to do. J Pak Med Assoc. 2010;60(9):718-721.
- [Google Scholar]
- Clinico-pathological study of carcinoma breast in Benin City. Afr J Reprod Health. 2001;5(2):56-62.
- [CrossRef] [PubMed] [Google Scholar]
- Role of high frequency ultrasonography in the evaluation of palpable breast masses in Chinese women: alternative to mammography? J Ultrasound Med. 1996;15(9):637-644.
- [CrossRef] [PubMed] [Google Scholar]
- The accuracy of breast ultrasound in the evaluation of clinically benign discrete, symptomatic breast lumps. Clin Radiol. 1998;53(7):490-492.
- [CrossRef] [PubMed] [Google Scholar]
- Predictive value of ultrasonography in the diagnosis of palpable breast lump. Kathmandu Univ Med J. 2003;1(2):78-84.
- [Google Scholar]
- Fine needle aspiration cytology, imprint cytology and tru-cut needle biopsy in breast lumps: a comparative evaluation. J Indian Med Assoc. 1991;89(7):192-195.
- [Google Scholar]
- Correlation between histopathology and fine needle aspiration cytology diagnosis of palpable breast lesions: a five-year review. Afr J Med Sci. 2007;36(4):295-298.
- [Google Scholar]
- Ten year consolidated report of the Hospital Based Cancer Registries, 1984–1993, an assessment of the burden and care of cancer patients. New Delhi: Indian Council of Medical Research; 2001.
- [Google Scholar]
- Comparison between fine needle aspiration cytology (FNAC) and core Needle biopsy (CNB) in the diagnosis of breast lesions. G Chir. 2014;35(7):171-176.
- [CrossRef] [Google Scholar]







