Translate this page into:
External Fixator vs. Locking Compression Plate in “Supracutaneous” Mode for Open Distal Tibial Fractures: A Comparison on Economics, Union, Functional Outcome and Complications

*Corresponding author: Dr. Manik Sehgal, Department of Orthopaedics, Pt Jawahar Lal Nehru Govt Medical College, Chamba, India. Maniksehgal2001@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kaur R, Sharma A, Thakur SK, Sehgal M. External fixator vs. locking compression plate in “supracutaneous” mode for open distal tibial fractures: A comparison on economics, union, functional outcome and complications. Int J Recent Surg Med Sci. 2024;10:12-21. doi: 10.25259/IJRSMS-2022-2-11
Abstract
Objectives
Historically, in the pre-antiseptic era, there was a great fear of open tibial factors because of high incidence of infection eventually leading to amputation and in many cases septicemia and death. Despite improvements in surgical techniques in the last century, the optimum treatment for open type IIIa and Type II tibial farcture remains controversial. Literature available on use of Ex-fix as a definitive and permanent modality is very sparse and is not encouraging. In order to maintain biology of the fracture and to expedite the healing process many institutions and surgeons are using Locking compression plate as an external fixator which is fondly called as supracutaneous plating (SCP).
Material and Methods
The patients who had Gustilo and Anderson type II and IIIa # of distal Tibia were enrolled in this study. They were randomized into 2 groups. In one group (Ex-Fix) external fixator was applied in and in another group SCP was done. Four general indicators, including direct cost of hospitalization, first surgery time, time to full weight bearing, and time to complete union were compared between the groups. The functional outcome of the ankle was assessed. Presence of infection, Time to union was noted in both cases.
Results
Mean time to fracture union was statistically less in SCP group 5.84 months as compared to 7.21 months in Ex–fix group. Also, 12 patients in Ex-fix group had to undergo a reoperation as compare to only 1 in SCP group. This led to higher cost of expenditure and higher duration of stay in Ex-fix group. AOFAS Score, Teeny and Wiss were better in SCP group as compared to Ex-fix group.
Conclusion
Highlighting the role Of LCP in Supracutaneous mode as a definitive and final surgery , thus reducing the financial and psychological implication of reoperations in open grade and tibial fractures which are seen in patients managed with Ex-fix in definitive mode or as an interval for secondary nailing, we recommend the use of routine use of SCP in such tibial fractures after thorough debridement and diligent handling of soft tissue.
Keywords
Economy
supracutaneous
trauma
INTRODUCTION
Tibial fractures belong to the most common category of long bone fractures encountered in the career of an orthopaedic surgeon. Because of the precarious blood supply, subcutaneous nature and minimal presence of soft-tissue over the shaft of the tibia, these fractures are vulnerable to open fractures with a high rate of non-union and infection. The incidence of tibia fractures is 40% of all open fractures, and these fractures are mostly complicated by damage to the skin, muscle, and neurovascular bundle.[1]
Also historically, in the pre-antiseptic era, there was a great fear of open tibial fractures because of the high incidence of infection, leading to amputation and, in some cases, septicemia and death.
Even today, with so much advancement in antisepsis, antibiotics, and newer fixation methods, this remains a challenging condition to treat. Recognition of early toileting debridement and fixation in collaboration with the plastic surgery department has improved the outcome, but this still remains a challenging problem, and there are many controversies regarding the type of fixation and the decision for second surgeries.
Gustilo and Anderson classification[2] has helped a lot in classifying these injuries so that a definitive protocol can be established for deciding the mode and type of fixation according to fracture classification.
Currently, the treatment of open distal tibial fractures includes thorough wound debridement, early bone stabilisation with an external fixator (Ex-Fix), and coverage of the bone with soft tissue. This aids in enabling early mobilisation, restoration of limb function, provision of a muscle cover for adequate blood supply to the bone and prevention of infection.[3]
Damage control orthopaedics, which is based on the principle of minimally invasive surgery of short duration and consists of Ex-Fix, followed by definitive internal fixation with nailing or plating, is being done to decrease the complication rate.[3] But it puts extra economic and psychological stress on the patient. The patient has to undergo two major surgeries, first is Ex-Fix followed by definitive nailing or plating, depending upon the soft tissue condition.
Using Ex-Fix as the only and definitive surgery has been tried in some studies,[4] but there are many serious and critical issues related to pin-track infection, malalignment, and poor union rates, leading to unplanned and urgent secondary fixation procedures and consequently adding more financial and psychological burdens.[5,6]
But for developing nations like India, where roads are not as safe as in western countries, safety measures are not strictly followed, and the incidence of such open tibial fractures is much higher. Putting patients and the economy under the extra burden of doing staged surgeries can add to patient’s morbidity and psychological stress. Using Ex-Fix as a definitive method can lead to much more complications.
In modern orthopaedics, the principle of biological osteosynthesis has gained a great reputation in fracture management. And in order to maintain the biology of the fracture and expedite the healing process, many institutions and surgeons are using a locking compression plate (LCP) as an Ex-Fix which is fondly called supracutaneous plating.[7,8]
In our study done in a medical institute located in difficult hilly terrain in a backward district of India, which sees a lot of open tibia patients, we compared the results of Ex-Fix versus supracutaneous plating in Open Grade II and IIIa distal tibial fractures.[2]
MATERIAL AND METHODS
This prospective interventional comparison study was carried out in the department of Orthopaedics for 12 months. Forty patients more than 18 years of age who had Gustilo and Anderson type II and Type IIIa[2] fractures of the distal tibia in both sexes were enrolled in this prospective study done at Pt. Jawahar Lal Nehru Govt. Medical College, Chamba, Himachal Pradesh. They were randomised into two groups of 20 each, according to the day of admission. A Senior consultant available on Tuesday, Thursday and Saturday performed Ex-Fix on these patients. Authors available on Monday, Wednesday and Friday performed supracutaneous plating. Initial toileting and debridement protocols were similar in both groups.
The patients were given a random study number, and there were no exclusions after Randomisation. Patients with pathological fractures, endocrine and rheumatologic disorders, diabetes mellitus, chronic kidney disease, immunodeficiency states, psychological impairment, or a low IQ were excluded. Those with open fractures according to Gustilo and Anderson type I or type III b and more, or fractures with a displaced intra-articular fragment, were also excluded.
Required approvals were obtained from the Ethics Committee of the medical college, and proper informed consent in local vernacular was obtained from all patients before surgery. The patients were selected based on those satisfying the inclusion criteria and followed up in the post-operative period immediately and for one year.
Surgical technique
All surgeries were performed by two orthopaedic consultants on the same OT team. Patients were operated on the same day, preferably within 10 hrs after trauma under coverage of broad-spectrum antibiotics. Thorough irrigation, debridement and lavage were performed on all the patients to remove all contaminants and necrotic soft tissue [Figures 1a and 1b]. Intravenous antibiotics were started on admission and continued until the fourth post-operative day. Pneumatic tourniquets were used in both groups.

- (a, b) Thorough toileting and debridement.
Steps for SCP
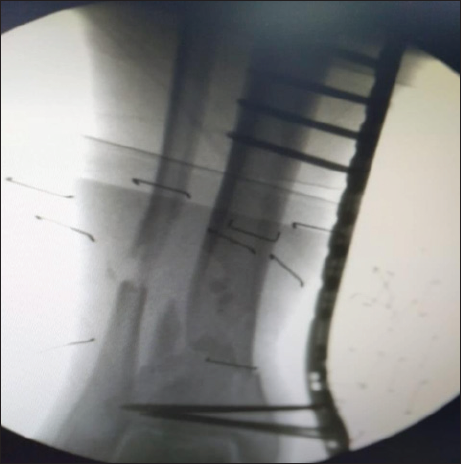
Fracture reduction is done prior to the application of the plate. LCP metaphyseal plate of the required length is taken by putting it over the tibia and crosschecking under the Image intensifier. The plate is initially fixed to the proximal and distal fragments with a k-wire after obtaining fracture reduction under Image intensifier guidance [Figures 2a and 2b]. LCP is placed as close to the bone as possible,[9] but some space at least one finger breadth is left for swelling and regular wound care, to increase the mechanical stability of the fixation [Figure 3]. For the distal tibia, a minimum of four screws proximally and four screws distally are recommended [Figure 4]. Distal screw length is properly checked so as to avoid intra-articular placement. Then holes are drilled over locking drill-sleeves through stab incisions made over the intact soft tissue envelope, and screws are placed first distally and later in the proximal fragment after ensuing good reduction. A screw tract and wound dressing were also done.

- (a) Open grade 3b fracture distal tibia. (b) Temporary reduction achieved under fluoroscopy and maintained with K wire.

- Final picture after plate application.
- Final picture after reduction.
Steps for Application of Ex-Fix
If anticipated skin closure is not interfering with connecting rods, Steinman pin is inserted in the calcaneum with one assistant giving traction and the other one giving counter traction [Figures 5 and 6].

- (a, b) Open Grade IIIa fracture of tibia.
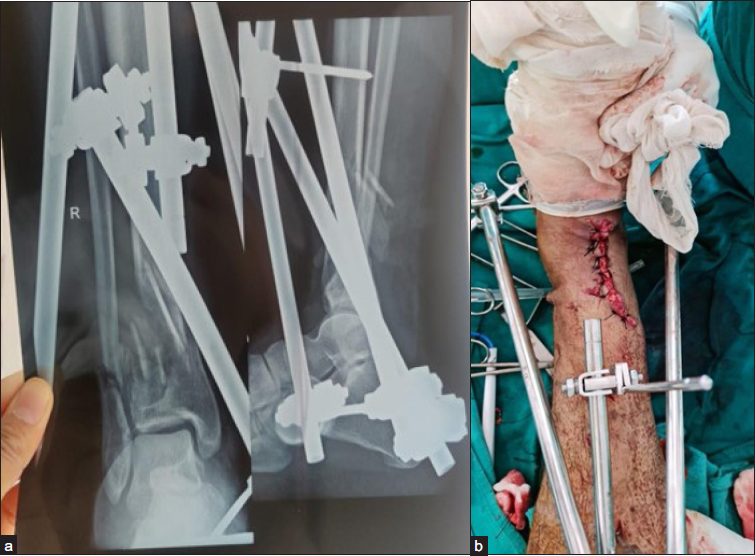
- (a) Radiograph after final reduction (b) clinical image after final reduction.
Two stab marks were given distal to the fracture site on the anteromedial aspect of the tibia, just medial to the shin. Similarly, two stab marks were made proximal to the fracture site. Cortical and cancellous Schanz screws were inserted in the respective bones. In the case where the skin defect is large, temporary reduction is done with k wire and then Ex-Fix is applied in the similar fracture.
In the cases, where much of the distal tibial metaphyseal area was present, T-type Ex-Fix geometry was used and the ankle was kept free. Nearby screws were kept closer to the fracture site and ditan Schanz pins were kept as far away as possible to provide maximum stability.
Implant and debridement costs were calculated in INR (Indian rupees).
The duration of surgery was recorded from the incision to wound closure. Postoperatively, IV 2nd generation cephalosporins and aminoglycoside antibiotics were continued for 4 days, followed by oral antibiotics for 5 days, along with limb elevation, analgesics, antacids, and trypsin chymotrypsin.
Early physiotherapy was encouraged by advocating active and passive movements at the knee and ankle joints.
An average stay in the hospital was recorded. The criteria for poor wound healing and superficial infection were defined as consistent drainage from the wound site for at least two days, or separation of wound edges to a width > 1 cm and a length > 1 cm.[10]
As a routine, after one month of surgery, follow-up radiographs were taken in all study patients to evaluate the progress of the fracture union. Gradual weight-bearing was permitted depending on the X-ray picture. Patients were called for both clinical and radiological assessments every 2 months until the fracture union was evident. When a bridging callus was visible on the X-ray, full weight bearing was encouraged. The union was defined when at least 3 cortices in both Anterio Posterior (AP) and lateral views have a bridging callus, and there is no pain, tenderness or abnormal mobility around the fracture site.[11]
The Ex-Fix and SCP were removed, as an outpatient procedure, once the complete union as per radiological and clinical criteria took place. Any complications and data, such as time to full weight bearing and time to complete bony union during follow-up were noted. The follow-up time averaged 17.15 months (range, 12–24 months) in the Ex-Fix F group and 16.20 months (range, 12–19 months) in the SCP group.
Parameters like cost of hospitalisation and surgery, surgical duration, time to full weight bearing, and time to complete union were compared between the two groups.
The functional outcome of the ankle was assessed with the help of AOFAS (American Orthopedic Foot and Ankle Society Ankle Score) and Teeny–Wiss criteria (symptoms and functional evaluation of ankle) at 12 months. Since it was for distal tibial fractures only, ankle scores were calculated.
The radiological outcome was assessed using the Teeny–Wiss scoring system and fracture union.[12]
The presence of infection and the time to union was calculated.
RESULTS
Data collected from the study of 40 cases; with a follow-up range of 6–24 months (mean 15 months) and results recorded were evaluated for demographic, injury characteristics, functional outcome, radiological outcome and complications.
There were 40 patients in the study. Twenty-five were males and fifteen were females. Twenty-three patients had type IIIa open fractures and 17 had type II open distal tibia fractures [Table 1].
| Ex-Fix (n = 20) | SCP (n = 20) | |
|---|---|---|
| Age (years) | ||
| Mean (range) | 45.31 (24–63) | 42.17 (26–65) |
| Gender | ||
| Male, n (%) | 13 (70) | 12 (60) |
| Female, n (%) | 7 (30) | 8 (40) |
| Gustilo–Anderson grading | ||
| Type-II | 8 (40) | 9 (45) |
| Type-IIIa | 12 (60) | 11 (55) |
The average time from injury to debridement (26 vs. 24) and average time from admission to debridement (18 vs. 17) were almost similar in both groups and statistically insignificant [Table 2].
| Variable | Ex- fix group | SCP group | P value |
|---|---|---|---|
| Average time from injury to debridement | 26 hours (4–84 hrs) | 24 hours (6–120 hrs) | NS |
| Average time from admission to debridement | 18 hours (0.6–48 hrs) | 17 hours (2–72 hrs) | NS |
| Type of implant used | Trans articular | LCP SS-8 | NS |
| Fix- 13 | LCP titanium-12 | ||
| T clamp EX-fix- 7 | |||
| Wound coverage | |||
| Primary closure | 17 | 19 | NS |
| Secondary cover | 2 | 1 | |
| Flap | 1 | ||
| Secondary Procedure | 12 | 1 | NS |
The percentage of patients with type II and type IIIa fractures getting Ex-Fix and SCP, respectively, was almost the same. So no bias was there according to the classification of fractures and the time interval between injury, admission and surgery.
The duration of surgery was statistically lower in the Ex-Fix group (1.20 hours) as compared to the SCP group (1.45 hour) [Table 3].
| General assessment indicators | Ex- Fix Group (n =20) | SCP group (n = 20) | P value |
|---|---|---|---|
| Total cost (INR) | 13,000 (6000–20,000) | 18,000 (10,000–26,000) | 0.052 |
| Cost for second | 35,000 | 5,000 (n = 1) | 0.0002 |
| Procedure | N = 12 | ||
| First surgery time | 1.20 | 1.45 | 0.002 |
| (hours) | (0.43–2.12) | (0.68–2.17) | |
| Time to full weight | 4.94 | 3.41 | <0.001 |
| Bearing (months) | (3.10–6.83) | (2.73–4.27) | |
| Time to complete | 7.21 | 5.84 | <0.001 |
| Union (months) | (4.60–14.13) n = 8 | (4.22–10.25), n = 19 |
When we considered the first admission and surgery, there was not much of a significant difference in cost incurrence between the two operating groups. However, when including the patients who had to undergo secondary procedures for fixation in both groups (n = 12 for Ex-Fix and n = 1 for SCP), the average cost of hospitalisation and surgery was way higher in the ExFix group [Table 3].
Union
Fracture union was defined as union within 6 months, delayed union as healing between 6 and 8 months, and non-union as the absence of healing after 8 months. The mean time to fracture union in the 8 open fractures in the Ex-Fix group, where no secondary procedure was required, was 7.21 months (4.60–14.13). The mean time for the fracture to unite in the 19 open tibia fractures in the SCP Group was 5.84 months (4.22–10.25) [Table 3].
Ten patients in the Ex-Fix group required secondary bone grafting and surgery. No bone grafting was done in the SCP group.
Pin track infections, superficial deep soft tissue infections
Pin track infections are an inherent and universal problem in Ex-Fix. Six patients developed pin track infections in Ex-Fix group [Figure 7]. In five of them, IV antibiotics according to pus culture sensitivity healed the infection, while in one patient, the pin had to be replaced under local anaesthesia. Only one screw site infection was seen in the SCP group, which was managed with oral antibiotics.

- Pin tract infection necessitating pin removal.
The incidence of deep tissue infection was similar in both groups. One patient in each group had to be reoperated for a deep infection. Antibiotic beads were inserted in these patients.
One patient in the Ex-Fix group had skin necrosis [Figure 8] for which the Flap procedure was performed.

- Necrosis of the skin leading to Flap procedure.
Figure 9 shows similar fracture patterns managed with Ex-Fix and SCP, respectively.

- Almost similar fracture pattern managed with Ex-fix on the left side and SCP on the right side.
Reoperations
Sixty percent of the patients in EX-Fix group were reoperated. Eleven patients had non-union and underwent bone grafting (6 patients) and fibular osteotomy (5) and definitive fixation with Intra medullary locking nail (IMLN) (6 patients) and SCP (% patients). No resurgery was done in the SCP group because of the lack of union. However, one patient developed a deep infection in the SCP Group, which necessitated the removal of the implant and the insertion of antibiotic beads. Luckily, the fracture was united and the infection was settled at the time of the removal of beads.
The incidence of delayed union was 60% in the Ex-Fix group and 30% in the SCP group. These eventually got united with dynamization and full weight bearing.
The time to get full weight bearing (months) was 4.94 months (3.10–6.83) in Ex-Fix groups, while it was significantly earlier at 3.41 months (2.73–4.27) in SCP groups.
The AOFAS score, including pain and function, was better in the SCP group as compared to the Ex-Fix group (p < 0.005). It indicates a better functional outcome and painless recovery in the SCP group [Table 4].
| Complication | Ex fix (n = 20) | SCP | p value |
|---|---|---|---|
| Infection | |||
| Pin-track infection, n (%) | 6 (30) | 1 (5) | 0.725 |
| Superficial wound infection, n (%) | 4 (20) | 1 (5) | 0.678 |
| Deep tissue infection, n (%) | 1 (5) | 1 (5) | 1.2 |
| Delayed union, n (%) | 12 (60) | 6 (30) | 0.008 |
| Non-union, n (%) | 8 (40) | 1 (5) | 0.004 |
| Secondary operation of changing fixation system, n (%) | 12 (60) | 1 (5) | 0.001 |
According to the Teeny–Wiss criteria, 18 patients (90%) had excellent/good outcomes in the SCP group, whereas 6 (30%) patients had good outcomes in the Ex-Fix group. Twelve cases with reoperation and complications in the LCP Group had a fair outcome [Table 5].
| Ex-Fix* | SCP† | P value | |
|---|---|---|---|
| AOFAS§ mean (95% CI) score at one year | 65.7 (61.4–70) | 83.9 (81.7–86.1) | <0.05 |
| Pain | 22.5 | 30.5 | <0.05 |
| Function | 34.3 | 42.2 | <0.05 |
| Alignment | 9.1 | 9.1 | <0.05 |
| Teeny and Wiss criteria (symptoms and functional evaluation of ankle) | |||
| Excellent | 6 (30%) | 18 (90) | <0.05 |
| Good | 2 (10%) | 2 (10) | >0.05 |
| Fair | 12 (60%) | - | |
| Radiological outcome using | |||
| Teeny–Wiss radiological score | |||
| Anatomical | 7 (35) | 15 (75) | <0.05 |
| Good | 5 (25) | 3 (15) | NS |
| Fair | 6 (30) | 2 (10) | NS |
| Poor | 2 (10) | 0 | <0.05 |
§American orthopedic foot and ankle society ankle score.
Radiological outcome using the Teeny–Wiss radiological score was Excellent in 75% of cases of SCP group, while only 35% of patients in the Ex-Fix group had an excellent radiological outcome.
Other complications
One patient in the SCP group had “free” head of locking screw [Figure 10] during implant removal. Luckily, all locking screws were removed, so by rotating the plate around the axis of the screw, uneventful removal of the screw and plate was done.

- “Freeing” of head of locking screw, creating difficulty in implant removal.
DISCUSSION
Open tibial fractures pose a significant challenge due to problems such as infection, soft tissue injury, malunion and non-union.[9]
These cases are best managed with immediate and urgent thorough irrigation and wound debridement. To obtain and maintain alignment and stability, an Ex-Fix, reamed or unreamed nailing with soft tissue cover, has been proposed.[10]
In spite of considerable advancements in surgical procedures in the last century, the definitive treatment for open type IIIa and Type II tibial fractures remain controversial.
There are various schools of thought regarding the initial application of Ex-Fix followed by conversion to Intamedullary (IM) nailing or plating.[11] However, the time duration of when to convert Ex-Fix to intramedullary nail is not defined in any of these studies, and the incidence of non-union and infections is very common.
Complications like infection following IMLN are very serious and limb threatening. It also adds significant economic and psychological morbidity for the patient.
External fixation has seen renewal in modern trauma management, especially in Damage Control Orthopaedics. But the literature available on the use of Ex-Fix as a definitive and permanent modality is very sparse and not encouraging. Ex-Fixes have their own limitations like infection, loss of reduction, non-union, large apparatus making it difficult in daily routine activities, and the incidence of reoperations.
We have used LCP as an Ex-Fix in open Grade II and IIIa fractures and have compared it with Ex-Fix.
Union and weight bearing occurred statistically earlier in the SCP group. It can be due to more rigid fixation across the fracture site due to the better purchase of 8 cortices around both ends of fracture by locking screws. Twelve patients have to undergo repeat surgery in the form of bone grafting and fibular osteotomy for union to occur in the Ex-Fix group, which is almost 60% in our study. Most of the patients sustaining open tibia fractures belong to a younger age group, which amounts to one of the most productive age groups, especially in developing nations like India. Such patients need an operative modality that lets them go to work as early as possible and avoid any future complications.
However, the authors want to stress the principle that a good initial reduction in the first surgery is of paramount importance no matter whether Ex-Fix or SCP is applied, as it is very difficult to achieve a secondary reduction if the primary reduction is unsuccessful.
Our results are in accordance with a study by Xu et al., where patients in the Ex-Fix group had a higher incidence of postoperative infection, malunion and non-union, and need more healing time and time to union.
The economy plays a major role in fracture management, and in developing countries like India, it has a major psychosocial aspect. This institute, where the study is conducted, is situated in one of the poorest districts of India. Repeat surgeries and prolonged stays are associated with a loss of productive days, especially in the younger age group. Our study has shown a very low cost of surgery with the SCP group, which is mainly due to the fact that in 90% of the cases, supracutaneous plating was the final and definitive surgery. Around 60% of the cases required secondary fixation in the Ex-Fix group as compared to just one case in the supracutaneous group (p < 0.0001), which was a highly significant result.
Since tibial pilon is associated with fibula fractures also, depending on the wound site and contamination. The fibula was temporarily fixed with k wire/tens nail in open and contaminated fractures.
This is a major highlight of our study that our modality has all the benefits of Ex-Fix like low chances of intramedullary infection, quick surgical time, no knee pain and easy outdoor implant removal, while the drawbacks of Ex-Fix like non-union, loss of reduction, heavy apparatus are not seen with our method of Ex-Fix.
LCP, which is a 3.5-mm plate, can be easily worn over jeans or suits and does not interfere with the patient’s gait.
In a study done by Holbrook et al.,[13] he operated on 28 open tibial shaft fractures with Ex-Fix. Such patients had a very high rate of pin-track infections (21%), malalignment (11%), malunion (36%), delayed union (21%) and non-union (11%). The incidence of pin tract infection in our Ex-Fix group was 30%. Only one patient in the SCP group got a screw site infection.
The incidence of superficial and deep infection was similar in both groups, and this can be attributed to the injury itself, soft tissue injury, loss of blood supply at the fracture site, anatomical location and not only because of implant used.[14,15]
The AOFAS score, including pain and function score, was better in the SCP group as compared to the Ex-Fix group. This signifies a better functional outcome and better range of motion in patients operated on with SCP plating. According to Teeny–Wiss criteria, 18 patients (90%) had excellent/good outcomes in the SCP group, whereas 6 (30%) patients had good outcomes in the Ex-Fix group. Collinge et al.[16] reported that the secondary operation was the only variable that was associated with a poor functional outcome (60% in the case of our patients). This can be a reason for the poor functional outcome in the Ex-Fix group, as 12 patients had secondary surgery.
The radiological outcome using the Teeny–Wiss radiological score was better in the SCP group.
Cases of delayed union were seen in 30% of cases in the SCP group and 60% of cases in the LCP group. Near Schanz screws were removed in the Ex-Fix group, and near locking screws were removed in the SCP group, which allowed for dynamization and bone union.
In our study, no fixation loss or implant failure was encountered in the SCP group.
CONCLUSION
Highlighting the role of LCP in supracutaneous mode as a definitive and final surgery, thus reducing the financial and psychological implication of reoperations in open grade and tibial fractures that are seen in patients managed with Ex-Fix in the definitive mode or as an interval for secondary nailing, we recommend routine use of supracutaneous plating in such tibial fractures after thorough debridement and diligent handling of soft tissue.
Good AOFOAS, Teeny–Wiss scores show higher level of patient acceptance, satisfaction and better functional outcome in supracutaneous plating.
LIMITATION
A larger number of study participants with longer duration of follow-up is needed for more conclusive results.
Ethical approval
Ethical approval was not required.
Declaration of patients consent
Written informed consent was obtained from all patients and/or families.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The epidemiology of open fractures in adults. A 15-year review. Injury. 2012;43:891-7.
- [CrossRef] [PubMed] [Google Scholar]
- In brief: Gustilo-Anderson classification. Clin Orthop Relat Res. 2012;470:3270-4.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Erratum in Clin Orthop Relat Res 2012;470:3624. Erratum in: Clin Orthop Relat Res. 2019;477:2388.
- [Google Scholar]
- Damage control surgery – experiences from a level I trauma center. BMC Musculoskelet Disord. 2017;18:391.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A review of the management of open fractures of the tibia and femur. J Bone Joint Surg Br. 2006;88:281-9.
- [CrossRef] [PubMed] [Google Scholar]
- External fixation for type III open tibial fractures. J Bone Joint Surg Br. 1990;72:801-4.
- [CrossRef] [PubMed] [Google Scholar]
- Intramedullary nailing versus external fixation in Gustilo type III open tibial shaft fractures: a meta-analysis of randomised controlled trials. Strategies Trauma Limb Reconstr. 2016;11:1-4.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- External fixation with standard AO-plates: technique, indications, and results in 31 cases. J Orthop Trauma. 2003;17:61-4.
- [CrossRef] [PubMed] [Google Scholar]
- Supercutaneous plating: use of a locking compression plate as an external fixator. J Orthop Trauma. 2009;23:72-5.
- [CrossRef] [PubMed] [Google Scholar]
- A review of management of open fracture of tibia and femur. JBJS. 2006;3:281-9.
- [CrossRef] [PubMed] [Google Scholar]
- Planned external fixation to locked intramedullary nailing conversion for open fractures of shaft of femur and tibia. J Coll Physicians Surg Pak. 2005;15:133-6.
- [PubMed] [Google Scholar]
- A meta-analysis of external fixator versus intramedullary nails for open tibia fracture fixation. J Orthop Surg Res. 2004;9:75.
- [Google Scholar]
- Treatment of open fractures of the tibial shaft: ender nailing versus external fixation. A randomized, prospective comparison. J Bone Joint Surg Am. 1989;71:1231-8.
- [PubMed] [Google Scholar]
- Minimally invasive plating of high-energy metaphyseal distal tibia fractures. J Orthop Trauma 2007
- [CrossRef] [PubMed] [Google Scholar]








