Translate this page into:
Profile of Upper Gastrointestinal Endoscopy Findings in Dyspeptic Patients
*Corresponding author: Althaf S. Ali, MBBS, MS, Department of General Surgery, Government T.D. Medical College, Vilayil Thekkethil, Venga P.O., Sasthamcotta, Kollam, Kerala, India. theheartpumps@gmail.com
Abstract
Background and Objectives
Dyspepsia is the commonest indication for upper gastrointestinal (UGI) endoscopy. This study was done to describe the UGI endoscopic findings and the risk factors like alcohol abuse, smoking, pan chewing, and drug intake and the endoscopic findings in patients with alarm symptoms.
Materials and Methods
This was an institution-based (Department of General Surgery at Government T.D. Medical College, Alappuzha) observational study (descriptive) on 250 dyspeptic patients who underwent UGI endoscopy for the duration of 1 year between November 2018 and October 2019.
Results
Among the patients, 130 were males and 120 were females. The mean age was 51.36 years. The majority were between 36 and 65 years (65.6%) of age. Precisely, 28.8% showed alarm symptoms. The commonest alarm symptoms were vomiting (26.8%), weight loss (7.6%), and gastrointestinal bleed (6.4%). Also, 237 (94.8%) patients had abnormal findings. The commonest abnormal findings included gastric erosions/erythema in 197 (78.8%), duodenal erosions/erythema in 69 (27.6%), and esophageal erosions/erythema in 56 (22.4%) patients. Substance use included smoking (29.6%), followed by alcoholism (27.2%) and pan chewing (14%). Dyspepsia along with alarm symptoms was seen in patients with malignant endoscopic findings. The commonest malignancy was stomach cancer (4.8%).
Conclusion
Dyspepsia was more common among males aged 36 to 65 years. Gastric, duodenal, and esophageal erosions/erythema were the commonest abnormal findings. Smoking and alcoholism were common in patients with dyspepsia. Malignant endoscopic findings were common in patients with alarm symptoms. UGI endoscopy is an effective and appropriate initial investigation to assess patients with dyspepsia.
Keywords
UGI endoscopy
dyspepsia
gastric
alarm symptoms
malignancy
Introduction
Dyspepsia with alarming features is thought to be associated with serious gastrointestinal (GI) diseases such as malignancy or ulcer.[1] Earlier, the diagnosis of upper gastrointestinal (UGI) tract was based on clinical and barium meal studies. Now the UGI endoscopy has a major role in both diagnosing and treating the UGI tract diseases effectively. Dyspeptic patients over 55 years of age, or those with alarm features, should undergo prompt esophago-gastro-duodenoscopy as it is the investigation of choice for evaluation of dyspepsia refractory to medical treatment and for dyspepsia with alarm symptoms. Advantage of negative endoscopy is that it reduces patient anxiety and increases patient satisfaction.[1]
This study was performed to know the pattern of various UGI diseases diagnosed with UGI endoscopy in the Department of General Surgery in a tertiary hospital and compare with similar studies in other parts of the world, and to describe the risk factors and alarming symptoms that help in early detection and treatment of UGI diseases, hence reducing the morbidity and mortality rate of uninvestigated dyspepsia.
Materials and Methods
The primary objective was to describe the esophageal, gastric, and duodenal endoscopic findings among patients undergoing UGI endoscopy for dyspepsia. The secondary objectives were to describe the endoscopic findings in patients with specific risk factors like alcohol abuse, smoking, pan chewing, and drug intake and to describe the endoscopic findings in patients with alarm symptoms such as vomiting, weight loss, GI bleed, dysphagia, odynophagia, and jaundice.
It was an institution-based observational study (descriptive) conducted in the General Surgery department of a tertiary teaching hospital for 1 year after getting approval from the Ethics Committee. Sample size, based on a study done by Shashikumar et al.,[5] which identified prevalence of gastric erosion/erythema or duodenal erosions/erythema as 28%, and using the formula Zα2PQ/L2, was calculated as 247. All patients undergoing UGI endoscopy in the Department of Surgery for dyspepsia were included. Patients <18 years, those with inadequate preparation, known malignancy, and acute conditions like UGI bleed, terminal illness, and high-risk comorbidity were excluded. Independent variables were age, sex, drug intake, addictions, and diet habits. Dependent variables included esophageal erosions/erythema grades 1 and 2, carcinoma esophagus, gastric erosion/erythema, polyp, carcinoma stomach, peptic ulcer, duodenal erosions/erythema, duodenal ulcer, and periampullary carcinoma. Patient details of history and examination findings were recorded as per proforma and endoscopy findings collected, entered in Microsoft Excel, and statistically analyzed using the software Statistical Package for the Social Sciences (IBM SPSS). Qualitative variables were entered as percentages and proportions.
Results
A total of 399 patients with dyspepsia had endoscopy, out of which 250 patients were included. Among them, 130 (52%) were males and 120 (48%) were females with a sex ratio of 1.08. Mean age was 51.36 years. Maximum patients were between 36 and 65 years of age, which accounted for 65.6%. Least numbers were between 18 and 25 (13%) and 76 and 85 (13%) years, as shown in [Figure 1].
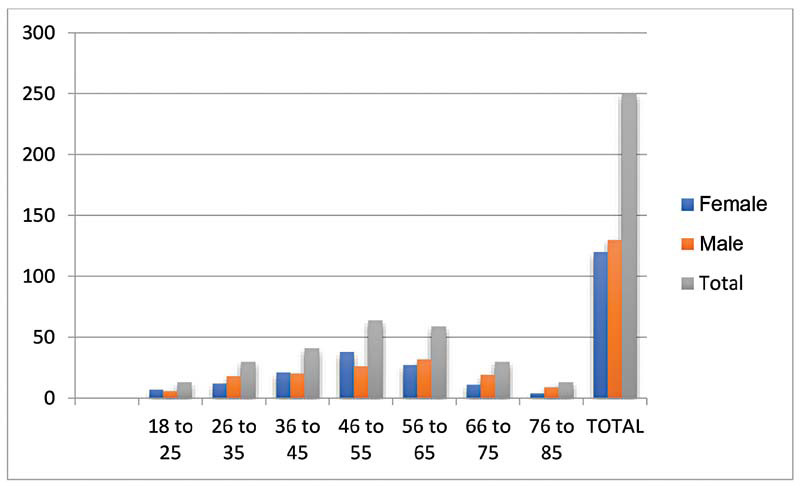
- Age- and sex-wise distribution of study subjects.
In this study, out of 250 patients, only 7 (2.8%) were vegetarians. Majority (243 [97.2%]) followed mixed diet habits. Majority of our subjects (206 [82.4%]) did not have a history of drug intake. Aspirin was used by 34 (13.6%) patients whereas 10 (4%) had used nonsteroidal anti-inflammatory drugs (NSAIDs). The most common alarm symptom was vomiting (67 [26.8%]), followed by weight loss (19 [7.6%]) and GI bleed (16 [6.4%]). Less common were dysphagia (9 [3.65%]), odynophagia (95 [2%]), and jaundice (1 [0.4%]). As detected in our study, 74 (29.6%) of the patients were smokers, 68 (27.2%) consumed alcohol, and 35 (14%) had a habit of pan chewing.
The positive endoscopic findings commonly observed were of mixed pattern (55.2%), involving different parts of the UGI tract. Mixed findings were more common in stomach and duodenum (64 [25.6%]); esophagus, stomach, and duodenum (41 [16.4%]); and esophagus and duodenum (5 [2%]). Isolated findings were commonly seen in stomach (78 [31.2%]) followed by esophagus (15 [6%]) and duodenum (6 [2.4%]). However, 13 (5.2%) patients showed normal findings.
Most common overall finding was gastric erosion/erythema in 197 (78.8%) of the subjects. Among the cases with gastric erosion/erythema, most common form was antral gastric erosion/erythema, which was seen in 190 (76%) subjects. Pangastric erosion/erythema was seen in 71 (28.4%) patients. Least common overall findings among different sites—gastroesophageal (GE) junction polyp (one patient) and periampullary carcinoma (one patient)—are detailed in [Table 1].
Site |
Findings |
n (%) |
|---|---|---|
Esophagus |
Barrett’s esophagus |
29 (11.6) |
Varices |
8 (3.2) |
|
Esophageal erosions/erythema |
56 (22.4) |
|
Esophageal polyp |
4 (1.6) |
|
Lax LES |
71 (28.4) |
|
Esophageal ulcer |
8 (3.2) |
|
Hiatus hernia |
27 (10.8) |
|
GE junction polyp |
1 (0.4) |
|
Carcinoma esophagus |
7 (2.8) |
|
Stomach |
Gastric erosion/erythema |
197 (78.8) |
Fundus gastric erosion/erythema |
76 (30.4) |
|
Body gastric erosion/erythema |
92 (36.8) |
|
Antral gastric erosion/erythema |
190 (76) |
|
Pyloric gastric erosion/erythema |
98 (39.2) |
|
Pangastric erosion/erythema |
71 (28.4) |
|
Gastric ulcer |
30 (12) |
|
Gastric polyp |
9 (3.6) |
|
Carcinoma stomach |
12 (4.8) |
|
Portal hypertension gastropathy |
3 (1.2) |
|
Duodenum |
Duodenal erosions/erythema |
69 (27.6) |
Duodenal polyp |
5 (2) |
|
Duodenal ulcer |
53 (21.2) |
|
Periampullary carcinoma |
1 (0.4) |
Abbreviations: GE, gastroesophageal; LES, lower esophageal sphincter.
Most common finding in esophagus was lax LES—lower esophageal sphincter—in 71 (28.4%) patients, followed by esophageal erosions/erythema in 56 (22.4%) patients. Least common finding in esophagus was GE junction polyp in one patient (0.4%). Carcinoma was seen in seven (2.8%) patients. The stomach finding was mostly antral gastric erosion/erythema (76%). Least common was portal hypertension gastropathy in three patients (1.2%). Carcinomatous lesions in stomach were seen in 12 (4.8%), which was the most commonly visualized malignant lesions in our study. The most common finding in duodenum was duodenal erosions/erythema in 69 (27.6%) patients. Least common was duodenal polyp in five (2%) patients. Periampullary carcinoma was seen in one patient.
Alcohol intake was statistically significant in esophageal varices, lax LES, carcinoma esophagus, pangastric erosion/erythema, gastric ulcer, carcinoma stomach, and duodenal erosions/erythema in this study. Smoking was found to be statistically significant in esophageal varices, lax LES, carcinoma esophagus, carcinoma stomach, and duodenal erosions/erythema. Pan chewing was statistically significant in hiatus hernia (the pan chewing might have simply aggravated the dyspepsia in patients with pre-existing hiatus hernia, making the patient seek medical help and finally ending up doing an endoscopy to reveal a hiatus hernia) and periampullary carcinoma [Table 2].
Findings |
Alcohol |
Smoking |
Pan use |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Y |
N |
Chi square |
p-Value |
Y |
N |
Chi square |
p-Value |
Y |
N |
Chi square |
p-Value |
|
Barrett’s esophagus |
8 |
21 |
1.659 |
0.198 |
6 |
23 |
0.003 |
0.003 |
5 |
24 |
3.807 |
0.051 |
Varices |
6 |
2 |
17.099 |
<0.05 |
7 |
1 |
21.746 |
21.746 |
1 |
7 |
0.227 |
0.633 |
Esophageal erosions/erythema |
44 |
14 |
1.41 |
0.235 |
15 |
43 |
0.983 |
0.983 |
7 |
51 |
1.699 |
0.192 |
Esophageal ulcer |
1 |
7 |
0.215 |
0.643 |
3 |
5 |
1.314 |
1.314 |
2 |
6 |
3.245 |
0.072 |
Lax LES |
7 |
64 |
6.578 |
<0.05 |
7 |
64 |
4.227 |
4.227 |
4 |
67 |
2.19 |
0.139 |
Hiatus hernia |
4 |
23 |
0.315 |
0.575 |
6 |
21 |
0.019 |
0.019 |
7 |
20 |
13.216 |
<0.05 |
Carcinoma esophagus |
4 |
3 |
6.936 |
<0.05 |
5 |
2 |
10.876 |
10.876 |
1 |
6 |
0.387 |
0.534 |
Pangastric erosion/erythema |
20 |
51 |
5.702 |
<0.05 |
16 |
55 |
0.106 |
0.106 |
2 |
69 |
3.619 |
0.057 |
Gastric ulcer |
12 |
18 |
5.909 |
<0.05 |
10 |
20 |
2.26 |
2.26 |
1 |
29 |
0.84 |
0.359 |
Carcinoma stomach |
6 |
6 |
8.038 |
0.05 |
9 |
3 |
21.84 |
21.84 |
1 |
11 |
0.002 |
0.965 |
Duodenal erosions/erythema |
20 |
49 |
6.477 |
<0.05 |
21 |
48 |
4.865 |
4.865 |
6 |
63 |
0.063 |
0.802 |
Duodenal ulcer |
12 |
41 |
0.65 |
0.42 |
11 |
43 |
0.008 |
0.008 |
3 |
50 |
0.5 |
0.479 |
Periampullary carcinoma |
0 |
1 |
0.232 |
0.63 |
0 |
1 |
0.27 |
0.27 |
1 |
0 |
11.546 |
<0.05 |
Abbreviations: LES, lower esophageal sphincter; N, no; Y, yes.
Alarm symptoms were statistically significant in hiatus hernia, carcinoma esophagus, carcinoma stomach, and periampullary carcinoma [Table 3].
Site |
Findings |
Alarm symptoms |
Chi square |
p-Value |
|
|---|---|---|---|---|---|
Yes |
No |
||||
Esophagus |
Barrett’s esophagus |
3 |
26 |
0.177 |
0.674 |
Varices |
2 |
6 |
1.102 |
0.294 |
|
Esophageal erosions/erythema |
7 |
51 |
0.036 |
0.849 |
|
Esophageal ulcer |
1 |
7 |
0.001 |
0.979 |
|
Lax LES |
7 |
64 |
1.26 |
0.262 |
|
Hiatus hernia |
7 |
20 |
4.672 |
<0.05 |
|
Carcinoma esophagus |
5 |
2 |
22.178 |
<0.05 |
|
Stomach |
Pangastric erosion/erythema |
12 |
59 |
1.494 |
0.222 |
Gastric ulcer |
6 |
24 |
0.062 |
0.803 |
|
Carcinoma stomach |
9 |
3 |
43.692 |
<0.05 |
|
Duodenum |
Duodenal erosions/erythema |
9 |
60 |
0.005 |
0.943 |
Duodenal ulcer |
5 |
48 |
0.683 |
0.409 |
|
Periampullary carcinoma |
1 |
0 |
6.84 |
<0.05 |
|
Abbreviation: LES, lower esophageal sphincter.
Discussion
Initial endoscopy in management of dyspepsia leads to significant improvement in symptoms, quality of life, and reduction in use of proton pump inhibitors.[2] Endoscopy helps in early detection of carcinoma in cases of dyspepsia.[3] In the present study, out of 250 subjects, 130 were males and 120 females. Majority were in the age group of 36 to 65 years (65.6%). Least were among 18 to 25 (13%) and 76 to 85 (13%) years. Only seven of the patients were vegetarians. Majority (82.4%) did not give a history of drug intake. Aspirin was used by 13.6%, and 4% took NSAIDs. Also, 12.8% had alarm symptoms. Most common alarm symptom was vomiting (26.8%), followed by unintentional weight loss (7.6%) and GI bleed (6.4%). Furthermore, 5.29.6% were smokers, 27.2% consumed alcohol, and 14% had a habit of pan chewing. Positive endoscopic findings were commonly observed in mixed pattern (55.2%), involving different parts of the UGI tract. Isolated findings were commonly seen in stomach (31.2%), followed by esophagus (6%) and duodenum (2.4%). However, 5.2% of them showed normal endoscopic findings. Mixed findings were more common in stomach and duodenum (25.6%). Most common overall finding was gastric erosion/erythema (78.8%). Most common esophageal finding was lax LES (28.4%) followed by esophageal erosions/erythema (22.4%). Most common finding in stomach was antral gastric erosion/erythema (76%). Most common finding in duodenum was duodenal erosions/erythema (27.6%). Carcinoma stomach was seen in 4.8%, carcinoma esophagus in 2.8%, and periampullary carcinoma was seen in 0.4% patients. Alarm symptoms were statistically significant in hiatus hernia, carcinoma esophagus, carcinoma stomach, and periampullary carcinoma.
Outcome of endoscopic finding in dyspepsia with alarm symptoms was 12.8% whereas it was 8% as reported by Sumathi et al.[2] In both studies, incidence of normal endoscopic findings is more in patients with dyspepsia without alarm symptoms. In our study, incidence of malignancy is more in patient with dyspepsia along with alarm symptoms. Our findings are compared with those of other authors as depicted in [Table 4].
Site |
Findings |
Resent study |
Antony and Vijayasarathy[4] |
Shashikumar et al.[5] |
Shrestha et al.[6] |
|---|---|---|---|---|---|
Esophagus |
Barrett’s esophagus |
11.6% |
0.2% |
– |
0.04% |
Varices |
3.2% |
0.6% |
– |
0.7% |
|
Esophageal erosions/erythema |
22.4% |
4.4% |
4% |
10.04% |
|
Esophageal polyp |
1.6% |
– |
– |
0.04% |
|
Lax LES |
28.4% |
16.1% |
17.1% |
– |
|
Esophageal ulcer |
3.2% |
– |
– |
– |
|
Hiatus hernia |
10.8% |
9% |
3% |
3.82% |
|
Carcinoma esophagus |
2.8% |
0.7% |
5.4% |
– |
|
Stomach |
Gastric erosion/erythema |
78.8% |
51.1% |
28% |
41.6% |
Gastric ulcer |
12% |
4.3% |
2.2% |
2.14% |
|
Gastric polyp |
3.6% |
– |
– |
0.04 |
|
Carcinoma stomach |
4.8% |
2.3% |
4.9% |
– |
|
Portal hypertension gastropathy |
1.2% |
0.1% |
– |
2.1% |
|
Duodenum |
Duodenal erosions/erythema |
27.6% |
22% |
– |
2.38% |
Duodenal polyp |
2% |
– |
– |
0.09% |
|
Duodenal ulcer |
21.2% |
2.6% |
2.8% |
4.67% |
|
Periampullary carcinoma |
0.4% |
0.1% |
– |
– |
Abbreviation: LES, lower esophageal sphincter.
Conclusion
It is concluded that UGI endoscopy is a very useful initial investigation to evaluate dyspepsia, especially when associated with alarm symptoms. Males underwent endoscopy more than females for evaluation of dyspepsia. Dyspepsia with alarm symptoms when evaluated often revealed malignant findings. Smoking and alcoholism was found to be major risk factors for dyspepsia.
Acknowledgment
I express my heartfelt thanks and gratitude to my respected teacher, Dr. V. Anilkumar, Professor and Head of the Department of General Surgery, and Dr. Mohandas, previous Head of the Department, for allowing me to select this topic and for their constant encouragement and valuable advice throughout the course of this study without whose help this work would not have been possible. I am extremely thankful to my guide Dr. Ramlal R.V., Associate Professor, Department of Surgery, for his expert guidance, constant supervision, and affectionate support, which has been invaluable for the successful completion of this study.
I would like to thank all Unit Chiefs of General Surgery department, Government Medical College, Alappuzha, for helping me with the clinical material for this study.
I extend my sincere gratitude to my seniors, dear friends, and juniors for their support.
I also thank staff in our department for all the timely help they provided.
I thank all the patients for their consent.
I thank the Almighty for never letting me waver from the right path.
Conflict of interest
None declared.
References
- Guidelines for the management of dyspepsia. Am J Gastroenterol. 2005;100:2324-37.
- [CrossRef] [PubMed] [Google Scholar]
- Appropriateness of indications for diagnostic upper gastrointestinal endoscopy in India. Singapore Med J. 2008;49:970-6.
- [PubMed] [Google Scholar]
- The role of endoscopy in dyspepsia. Gastrointest Endosc. 2007;66:1071-5.
- [CrossRef] [PubMed] [Google Scholar]
- Trends and patterns of diagnosis by upper GI endoscopy in dyspeptic patients: a retrospective study. IAIM. 2016;3:132-9.
- [Google Scholar]
- Pattern of upper gastrointestinal diseases: an audit of 1000 cases based on endoscopic findings from a tertiary care hospital in Mysore. Int Surg J.. 2018;5:2412-6.
- [Google Scholar]
- Upper gastrointestinal endoscopy findings in patient presenting with dyspepsia. J Patan Acad Health Sci.. 2015;2:19-22.
- [Google Scholar]








