Translate this page into:
Single versus Three Doses of Intraarticular Platelet-Rich Plasma Injection in Treatment of Early Osteoarthritis Knee Joint—A Prospective Comparative Study
*Corresponding author: Vishnu Jayaprakasan, MS, Sankaramangalam House, PO-Panniyanore, Thalassery, Kannur District, Kerala, India. vishjnambiar@gmail.com
Abstract
Background
Autologous platelet-rich plasma (PRP), which contains a pool of growth factors, appears to offer an easy solution for delivering multiple growth factors needed for tissue repair. The objective of the study is to compare between single versus three doses of intraarticular platelet-rich plasma injection in the treatment of early osteoarthritis knee joint.
Materials and Methods
A prospective comparative study was done on 100 patients with early osteoarthritis knee who were randomized into two groups in an alternating fashion—single-dose injection and triple-dose injection groups. PRP (5 mL) obtained by double-spin method was injected per knee and followed up at 1, 3, and 6 months and outcomes measured using WOMAC (Western Ontario and McMaster universities osteoarthritis index) and VAS (visual analog scale) scores.
Results
VAS scores showed a statistically significant difference in triple-dose group at all follow-ups. In WOMAC, such a difference was observed for stiffness subscore at all the follow-ups, but the pain subscore and total score showed an improvement only at the final follow-up with the functional assessment subscore showing no statistical difference at any follow-ups.
Conclusion
PRP injection appears to be effective in early symptomatic osteoarthritis with better clinical results using a triple-dose regimen.
Keywords
Platelet-rich plasma (PRP)
Osteoarthritis
Kellgren-Lawrence grading (K-L grade)
WOMAC
VAS
Introduction
Osteoarthritis (OA), commonly known as wear and tear arthritis, is a condition in which the protective cartilage on the ends of the bone forming a synovial joint wears down over time.[1] The word OA is a misnomer as primary event is not inflammation but degeneration due to which at a later stage secondary synovial inflammation can occur, and hence the word OA is more apt. OA is the most common type of arthritis in both developed and developing countries. About 9.6% of men and 18.0% of women above 60 years have symptomatic OA worldwide as per the World Health Organization (WHO). It is the second most common rheumatologic problem of our country and is the most frequent joint disease with a prevalence of 22 to 39%.[2] OA is the fourth leading cause of “years lived with disability” (YLD), accounting for 3.0% of total global YLDs and accounts for 6.8% of disability-adjusted life years worldwide.[3,4] Knee and hip joint replacement procedures account for 35% of the total arthritis procedures conducted during a hospitalization.[5] As per the WHO by 2030, the demand for total knee arthroplasties will increase up to 67%.[3,4]
OA has been studied in detail for more than a century now with the opinions regarding its cause changing from time to time. It has been established that no single cause leads to it and hence is considered to be of multifactorial origin. Current concepts revolve around the imbalance between proinflammatory cytokines (interleukin [IL]-1a, IL-1, and tumor necrosis factor-1) and anti-inflammatory cytokines (including IL-4, IL-10, and IL-1ra). This cytokine imbalance is thought to activate proteolytic enzymes, leading to the destruction of cartilage.[6]
Role of PRP in osteoarthritis
Platelet-rich plasma (PRP) is an autologous mixture of highly concentrated platelets (5–6 times the baseline with expected platelet counts of 6–10 lakhs per mm3).[7,8] PRP has also been found to have anti-inflammatory actions. The inflammatory cascade generated by members of cyclooxygenase family can be inhibited by anti-inflammatory mediators present in PRP. The role of different growth factors is illustrated in [Figure 1]. PRP has been the recent advancement in the management of early OA as a regenerative and ortho-biological tool. The safety and efficacy of PRP have been confirmed by previous studies.[7–10] Compared with hyaluronic acid, corticosteroids, autologous conditioned serum, and placebo, PRP has been found to have improved outcomes in recent studies.[8,10–13]
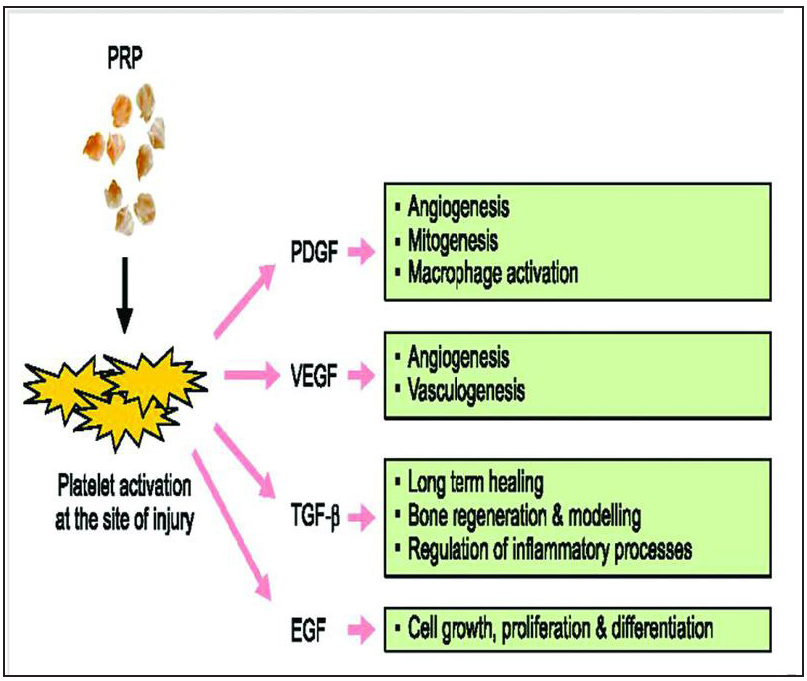
- Growth factors of platelet-rich plasma (PRP) with function. EGF, epidermal growth factor; VEGF, vascular endothelial growth factor; PDGF, platelet-derived growth factor; TGF-ß, transforming growth factor-beta.
Our aim in this study is to compare the efficacy between single injection versus three-time injection of PRP for OA treatment. We have opted for three doses of PRP as many recent studies have failed to find any significant difference in outcome between single-dose and double-dose PRP.[13,14]
Methods
A total of 124 consenting patients with early-stage OA who presented to Orthopedics Outpatient Department (OPD) at Netaji Subhash Chandra Bose Medical College, Jabalpur, Madhya Pradesh, between January 2020 and October 2021 were screened for the study out of which 100 were selected who qualified the inclusion criteria and were randomized into two groups—50 patients for single-dose injection and 50 for triple-dose injection, in an alternating fashion. The institutional ethical committee has reviewed and approved the above study in January 2020.
-
Age of the patient between 40 and 60 years with knee pain and swelling
-
Grade I and II
Exclusion criteria
-
Grade III and IV
-
Posttraumatic and intraarticular fracture knee
-
Patients with rheumatoid arthritis of knee joints
-
Hematological diseases (coagulopathies)
-
Active or sequelae of infections
-
Patients with immunosuppression
-
Severe cardiovascular diseases
-
Major axial deviation (varus more than 5 degrees, valgus more than 5 degrees)
-
Patients on therapy with anticoagulants and antiplatelets or use of nonsteroidal anti-inflammatory drugs within 5 days before blood extraction.
-
Patients with endocrinal and metabolic conditions(gout).
-
Contralateral knee joint in case of bilateral OA.
Methodology
Consent for Participation in Study: Each participant along with his/her attendant was informed regarding their inclusion in the study with consent form and patient information sheet. Each participant was explained in his/her language regarding his/her disease, investigation details, management protocol, alternative measures, anticipated outcome, and probable complications related to surgery. Participants were counseled for their compliance in regular follow-up.
Randomization: The research was done on an OPD basis. The subjects were assigned into single-dose and triple-dose category on an alternating basis, that is, subject 1 and every odd-numbered patient thereafter were given single dose of PRP, while subject 2 and every even-numbered patient thereafter were subjected to three doses of PRP. In bilateral conditions, the knee that comes under the inclusion criteria is selected.
Standard operating procedure for the preparation of PRP:
-
Place of collection—operation theater
-
Amount of blood collected—40 mL of venous blood was collected (gave around 5–7 mL of PRP after double spin)
-
Site—from the antecubital vein or femoral vein under strict aseptic precautions with an effort to avoid irritation and trauma to the platelets with the syringe
-
Vials used—multiple vacutainers or test tubes containing ethylenediaminetetraacetic acid as an anticoagulant.
-
Processing—The tubes were centrifuged at 3,000 rpm for 10 minutes to separate erythrocytes (soft spin), and at 5,000 rpm for 10 minutes to concentrate platelets (hard spin)—double-spin techniquE[11,12]
-
Extraction of PRP was done with the help of another syringe and the final PRP was loaded for injection in a 10 mL syringe.
Intraarticular injection of PRP
Position of the patient—supine.
Procedure—knee was scrubbed, painted, and draped with sterile towels.
With the patient’s knee in 45 to 90 degrees of flexion, lateral parapatellar soft spot was palpated.
Under strict aseptic conditions, 5 mL platelet concentrate was injected into the knee joint with an 18-gauge needle without local anesthetic.
Soon after injection, the knee joint was subjected to multiple cycles of range of motion.
For any possible side effects like dizziness, sweating or local reaction the patients were observed for another 30 minutes.
Postinjection protocol:
After the injection, patients were sent home with instructions to restrict the use of the leg for 24 hours and to use cold/ice therapy for knee if there was a pain. The only permitted medication throughout the study period was acetaminophen and that too only if needed (on SOS basis). Adverse effects like pain, swelling, redness, and infection were recorded at each follow-up visit. Weight bearing was permitted after 24 hours.
Administration schedule—single dose: day 0.
Triple injection—day 0, day 14, and day 30.
Follow-up single dose—at 1, 3, and finally at 6 months.
Triple dose—at 1, 3, and at 6 months after the third dose.
Outcome measurement—WOMAC (Western Ontario and McMaster universities OA index) and VAS (visual analog scale) scores.
The WOMAC consists of 24 items divided into three subscales. To suit the WOMAC score with Indian rural population, we had replaced the item getting in/out of a car with getting in/out of auto, and putting on/taking off socks with cleaning of ankles [Figure 2]. Each item of WOMAC score described in terms of none, mild moderate, severe, and extreme. These correspond to an ordinal scale of 0 to 4. Each component of the WOMAC score ranges between 0 to 20 for pain, 0 to 8 for stiffness, and 0 to 68 for functionality. A total WOMAC score was created by summing the items for all three subscales, ranging from 0 to 96. Outcome measured was quantified in percentage of improvement. The means of each parameter and total WOMAC score were calculated.

- Western Ontario and McMaster universities osteoarthritis index scoring.
VAS is a straight line with the left end of line representing no pain and right end of line representing worst pain [Figure 3]. There are four categories.
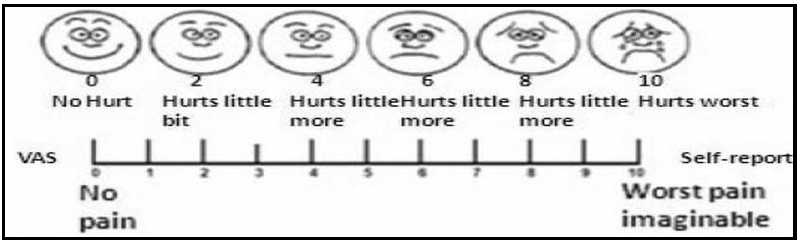
- Visual analog scale (VAS) scoring.
-
None (0)—no pain for activity.
-
Mild (1–3)—pain present occasionally while at work.
-
Moderate (4–6)—pain present but can continue with work.
-
Severe (7–10)—pain forces discontinuation of the work but can be resumed after rest.
Statistical analysis
Nonnumeric entries were coded numerically into nominal/ordinal distribution before analysis. Key for numerical coding was prepared (attached). The data obtained was analyzed using the Statistical Package for the Social Sciences (SPSS) 21.0 version. All continuous data was expressed in terms of the mean and the standard deviation of the mean. To assess the differences in the mean of the two groups, t-test was performed. The nonparametric Pearson’s chi-squared test was performed to investigate the relationships between grouping variables. For all these tests, p < 0.05 was considered significant.
Observations and Results
The basic demographic and patient variables are quoted in Table 1. Their distribution among both the limbs of the study was proven to be statistically insignificant (p > 0.05), thereby nullifying their distribution overall.
Variables |
Dosing schedule |
p-value (Pearson chi-squared tests) |
||||
|---|---|---|---|---|---|---|
Single dose, n (%) |
Triple dose, n (%) |
|||||
Age group |
40–50 |
9 |
18.0% |
11 |
22.0% |
0.617 |
50–60 |
41 |
82.0% |
39 |
78.0% |
||
Sex |
Female |
27 (54) |
54.0% |
28 |
56.0% |
0.841 |
Male |
23 (46) |
46.0% |
22 |
44.0% |
||
Religion |
Hindu |
45 |
90.0% |
46 |
92.0% |
0.603 |
Jain |
1 |
2.0% |
0 |
0.0% |
||
Muslim |
4 |
8.0% |
4 |
8.0% |
||
Side |
Left |
20 |
40.0% |
28 |
56.0% |
0.109 |
Right |
30 |
60.0% |
22 |
44.0% |
||
Kellgren-Lawrence grade |
I |
7 |
14.0% |
2 |
4.0% |
0.081 |
II |
43 |
86.0% |
48 |
96.0% |
||
Majority of the patients in our study belonged to age group 50 to 60 years (80%). Mean age of the study was 54.13 ± 5.24 years ranging from 40 to 60 years. Age distribution in both the groups was comparable with higher number of patients in 50 to 60 years group in both the limbs of the study (82 and 78%, respectively). p-Value using chi-squared test was 0.617 rendering the age factor insignificant. Of the 100 patients enrolled in the study, 55 were females and 45 were males. Sex distribution in both the groups was comparable with higher number of females in both the limbs of the study (54 and 56%, respectively). p-Value using chi-squared test was 0.841 rendering the gender factor insignificant.
In our study, right knee OA (52%) was more compared with left knee. Sixty percent of patients enrolled in single-dose regimen and 54% of patients in triple-dose regimen had right-sided OA. p-Value using chi-squared test was 0.109 rendering the factor statistically insignificant. Most of the patients in our study had grade II Kellgren-Lawrence OA of knee joint. The grades of OA in both the limbs were comparable with 86 and 96%, respectively, being grade II Kellgren-Lawrence. The chi-squared test showed a p-value of 0.081 rendering the factor statistically insignificant.
The mean height in our study was 161.95 ± 11.72 cm ranging from 144 to 185 cm. The mean weight in our study was 69.47 ± 8.72 kg ranging from 48 to 88 kg. In our study, majority of the patients were having high body mass index (BMI) of more than 25 kg/m2 constituting 61% of the study patients (with obese constituting 24% among them and the remaining 86% being overweight as per the WHO categories of obesity). The mean BMI was 26.81 ± 4.72 kg/m2 ranging from 17.24 to 41.28 kg/ m2.
Comparison Statistics: Outcome measurements were done using VAS and WOMAC scores between the two groups at 1, 3, and 6 months follow-up. To assess the differences in the mean of the two groups, t-test was performed. For all these tests, p < 0.05 was considered significant. The data are given in Table 2.
Variables with dosing schedule |
Mean |
SD |
t-value |
p-value |
|
|---|---|---|---|---|---|
Age (years) |
First dose |
54.36 |
5.20 |
0.44 |
0.66 |
Triple dose |
53.90 |
5.34 |
|||
Height (cm) |
First dose |
161.86 |
11.60 |
0.08 |
0.94 |
Triple dose |
162.04 |
11.98 |
|||
Weight (kg) |
First dose |
69.00 |
8.80 |
0.54 |
0.59 |
Triple dose |
69.94 |
8.71 |
|||
BMI (kg/m2) |
First dose |
26.71 |
5.07 |
0.21 |
0.83 |
Triple dose |
26.92 |
4.42 |
|||
VAS at 1 month postinjection |
First dose |
5.12 |
0.75 |
2.21 |
0.03 |
Triple dose |
4.78 |
0.79 |
|||
VAS at 3 months postinjection |
First dose |
4.70 |
0.68 |
4.08 |
0.001 |
Triple dose |
4.10 |
0.79 |
|||
VAS at 6 months postinjection |
First dose |
4.08 |
0.72 |
4.98 |
0.001 |
Triple dose |
3.40 |
0.64 |
|||
WOMAC pain score at 1 month |
First dose |
13.32 |
1.36 |
0.20 |
0.844 |
Triple dose |
13.26 |
1.66 |
|||
WOMAC pain score at 3 months |
First dose |
12.44 |
1.33 |
1.81 |
0.073 |
Triple dose |
11.96 |
1.32 |
|||
WOMAC pain score at 6 months |
First dose |
11.64 |
1.17 |
5.28 |
0.001 |
Triple dose |
10.38 |
1.21 |
|||
WOMAC stiffness score at 1 month |
First dose |
4.72 |
0.67 |
3.17 |
0.002 |
Triple dose |
4.32 |
0.59 |
|||
WOMAC stiffness score at 3 months |
First dose |
4.14 |
0.50 |
4.76 |
0.001 |
Triple dose |
3.56 |
0.70 |
|||
WOMAC stiffness score at 6 months |
First dose |
3.80 |
0.81 |
5.91 |
0.001 |
Triple dose |
2.86 |
0.78 |
|||
WOMAC functional score at 1 month |
First dose |
45.78 |
6.43 |
1.03 |
0.306 |
Triple dose |
47.48 |
9.77 |
|||
WOMAC functional score at 3 months |
First dose |
43.40 |
6.52 |
0.05 |
0.960 |
Triple dose |
43.48 |
9.24 |
|||
WOMAC functional score at 6 months |
First dose |
41.44 |
6.15 |
1.63 |
0.106 |
Triple dose |
38.96 |
8.83 |
|||
WOMAC total score at 1 month |
First dose |
63.82 |
7.21 |
0.68 |
0.501 |
Triple dose |
65.06 |
10.78 |
|||
WOMAC total score at 3 months |
First dose |
60.08 |
7.17 |
0.64 |
0.525 |
Triple dose |
59.00 |
9.58 |
|||
WOMAC total score at 6 months |
First dose |
56.88 |
6.56 |
3.00 |
0.003 |
Triple Dose |
52.20 |
8.88 |
|||
Abbreviations: BMI, body mass index; SD, standard deviation; VAS, visual analog scale; WOMAC, Western Ontario and McMaster universities osteoarthritis index.
Discussion
OA is the most common form of degenerative arthritis affecting elderly. Knee joint is the largest joint of the body. Being a weight bearing joint, it is prone to wear and tear and hence most commonly involved in OA. The targets of treatment for knee OA include controlling pain, minimizing physical limitations, increasing quality of life and if possible, stop progression of pathological process. Intraarticular injectables include corticosteroids, hyaluronic acid viscosupplementation, and autologous PRP. Of these PRP is thought to reverse the disease process and repair the degenerative cartilage in cases of early ongoing pathology and therefore has been studied in detail regarding its cellularity, growth factor contents, and its clinical efficacy in OA. Previous studies have already proved its efficacy, but lacunae in those studies exist regarding its standardized dosing, side effects, grades in which to be used efficiently and also the benefits of multiple dose injection as compared with single dose. In our study, we have aimed to answer some of these by assessing the efficacy of intraarticular injection of PRP in early OA (Kellgren-Lawrence grade I and II) and to compare the efficacy between single versus triple doses of PRP injection.
Both the groups were comparable on baseline characteristics of age, height, weight, BMI, preinjection VAS, and WOMAC scores. We used the double-spin technique to separate the PRP and infused it without any pretreatment. PRP (5 mL) was infiltrated under strict aseptic precautions through lateral parapatellar soft spot. The efficacy of PRP in reducing pain, stiffness, and physical function was assessed and scored on WOMAC index and VAS scores. Filardo et al.[8] used three injections of 5 mL volume each at 4 weeks interval and VAS and WOMAC scores were used to assess the outcome. Sooraj[9] et al. did a study on 70 patients having early OA using a single injection of 5 mL and WOMAC scores were used to assess the outcome. Patel et al.[10] did a study on 78 patients (156 knees) to compare the efficacy between single versus double dose of PRP the in treatment of early OA and WOMAC scores were used to assess the outcomes. Dilekci et al.[15] did a study with 210 patients to compare efficacy of single versus triple doses of PRP in the treatment of early OA and used VAS and WOMAC scores to assess the outcomes.
Outcome Assessment: VAS scores showed a significant difference between both the groups with the triple-dose therapy showing greater pain relief at 1 month (p < 0.05), at 3 months (p < 0.05), and at 6 months follow-up (p < 0.05), respectively, as compared with single-dose regimen.
Patel et al.[10] did a study to compare the efficacy between single versus double dose of PRP in the treatment of early OA and found that the VAS scores decreased from 4.54 to 2.16 in single dose and from 4.64 to 2.54 in double dose at 6 months follow-up with no statistically significant difference between them. Aziz[16] did a study in 174 patients who were divided into three groups—single-, double- and triple-dose therapy groups—and were evaluated using VAS, WOMAC, and International Knee Documentation Committee (IKDC) scores that were calculated before treatment, 6 and at 12 months after the last dose. They observed significant improvements in VAS scores (p < 0.001) in all three injection groups as compared with preinjection values, and comparison among the groups revealed that double and triple-dose regimens had more improvement as compared with single dose and no significant difference could be found between double and triple dose at 12 months post treatment.
Mean WOMAC pain scores of single-dose therapy at the end of 1, 3, and 6 months were 13.32 ± 1.36, 12.44 ± 1.33, and 11.64 ± 1.17, respectively, and for triple-dose therapy mean WOMAC pain scores were13.26 ± 1.66, 11.96 ± 1.32, and 10.38 ± 1.21, respectively. Statistically significant differences in pain were present only at the end of 6 months between the two groups (p < 0.05). Mean WOMAC stiffness scores of single-dose therapy at the end of 1, 3, and 6 months were 4.72 ± 0.67, 4.14 ± 0.50, and 3.80 ± 0.81 for single-dose therapy and 4.32 ± 0.59, 3.56 ± 0.70, and 2.86 ± 0.78 for triple-dose therapy. Statistically significant differences in stiffness were present at all the follow-ups between the two groups (p < 0.05). Mean WOMAC functional assessment scores of single-dose therapy at the end of 1, 3, and 6 months were 45.78 ± 6.43, 43.40 ± 6.52, and 41.44 ± 6.15 for single-dose therapy and 47.48 ± 9.77, 43.48 ± 9.24, and 38.96 ± 8.83 for triple-dose therapy. Statistically significant differences in functional assessment were NOT present at all the follow-ups between the two groups (p > 0.05). Mean WOMAC total scores at the end of 1, 3, and 6 months were 63.82 ± 7.21, 60.08 ± 7.17, 56.88 ± 6.56 for single-dose therapy and 65.06 ± 10.78, 59.00 ± 9.58, 52.20 ± 8.88 for triple-dose therapy. Statistically significant differences in WOMAC total scores were present only at 6 months follow-up between the two groups (p < 0.05). Vamshi et al.[14] did a study to compare the efficacy between single versus double dose of PRP in the treatment of early OA and found similar results with both the therapy. They, thus, concluded that both therapy regimens had only short-term effectiveness for relieving pain, stiffness and improving knee functions, and their effects were comparable that tend to taper off over time; hence, there was a need of staged injections over many months to sustain it. Huang et al.[17] did a study on 191 knees (127 patients) and compared the clinical results of single-dose, double-dose, and triple-dose regimens using VRS (visual rating scale), WOMAC, and IKDC scores. They found significant improvements in all scores after treatment as compared with pretreatment values (p < 0.05), and the parameters of VRS and WOMAC stiffness/pain/function score showed significant differences among the three groups in favor of triple-dose regimen (p < 0.05). Three dose groups had higher scores and more improvement at 12 months after treatment when compared with other groups. Aziz[16] did a study in 174 patients who were divided into three groups—single-, double- and triple-dose therapy groups—and were evaluated using VAS, WOMAC, and IKDC scores that were calculated before treatment, 6 months and at 12 months after the last dose. WOMAC scores showed significant improvements in multiple-dose therapy as compared with single dose, but no significant difference could be observed in between double- and triple-dose regimens. They concluded that single dose was less sufficient in creating a therapeutic effect and thus appropriate method would be at least two-dose therapy for the management of early OA. Dilekci et al.[15] did a nonrandomized comparative study to assess the effect of single versus triple injection of PRP in the treatment of early OA knee. They found that at 3 weeks there were significant differences between the two groups in all parameters except WOMAC pain and stiffness. At 6 weeks, they found significant differences between the two groups in all parameters except WOMAC pain. They thus concluded that there were better results with triple-dose regimen as compared with single dose in various subscores of WOMAC and overall WOMAC at 6 weeks postinjection.
Conclusion
Our study has revealed a consistent reduction in pain, stiffness, and overall improvement in functional status of the patients of early-stage OA who have been treated with PRP. The efficacy of triple dose over single dose was significant in certain domains of the morbidity scores especially the pain and stiffness, but the overall improvement in functional status was significant only at 6 months of follow-up. No major side effects were noted throughout the course. We can thus safely conclude that autologous PRP can be added to the armamentarium of an orthopaedic surgeon for the management of early stages of OA that can probably delay the progress of disease and thereby reduce the need for early surgeries. Further it offers an affordable alternative to other orthobiologicals that are very costly in comparison.
Conflicts of interest
None declared.
Source of support
Nil.
References
- Osteoarthritis(OA)|Arthritis|CDC.Cdc.gov. https://www.cdc.gov/arthritis/basics/osteoarthritis.htm Published 2022. Accessed June 8, 2022
- [Google Scholar]
- Osteoarthritis|NationalHealthPortalOfIndia(https://www.nhp.gov.in/disease/musculo-skeletal-bone-joints-/osteoarthritis) Accessed June 8, 2022
- [Google Scholar]
- Health Care Burden of Musculoskeletal Disease, 2001. World Health Organization: www.boneandjointdecade.org. Accessed June 8, 2022
- [Google Scholar]
- WHO-osteoarthritis chapter 6, subchapter 12 (https://www.who.int/medicines/areas/priority_medicines/Ch6_12Osteo.pdf) Accessed June 8, 2022
- [Google Scholar]
- Direct medical costs unique to people with arthritis. J Rheumatol. 1997;24:719-25.
- [PubMed] [Google Scholar]
- The pathophysiology of osteoarthritis: a mechanical perspective on the knee joint. PMR. 2012;4:S3-S9.
- [Google Scholar]
- Intra-articular platelet-rich plasma injections for knee osteoarthritis: an overview of systematic reviews and risk of bias considerations. Int J Rheum Dis. 2017;20:1612-30.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet-rich plasma vs hyaluronic acid to treat knee degenerative pathology: study design and preliminary results of a randomized controlled trial. BMC Musculoskelet Disord. 2012;13:229.
- [Google Scholar]
- Intra articular injection of platelet rich plasma in grade 1 and 2 knee osteoarthritis and assessment of functional outcome: a longitudinal interventional study. Int J Orthop (Hong Kong). 2020;6:557-60.
- [Google Scholar]
- Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am J Sports Med. 2013;41:356-64.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of autologous conditioned serum (ACS), platelet-rich plasma (PRP), hyaluronic acid (HA) and steroid for early osteoarthritis knee: a comparative analysis. Indian J Orthop. 2020;55:217-27.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The efficacy of autologous platelet rich plasma vs homologous platelet lysate in patients with early knee osteoarthritis. Int J Orthopaed Rheumatol. 2018;4:47-53.
- [Google Scholar]
- Multiple PRP injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: a randomized, double-blind, placebo-controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25:958-65.
- [Google Scholar]
- A prospective study of intra-articular injections of platelet rich plasma in early osteoarthritis knee joint. Int J Res Orthop. 2018;4:133-40.
- [Google Scholar]
- Effect of single or multiple injection of platelet-rich plasma in comparison with hyaluronic acid on knee osteoarthritis. Experiment Biomed Res. 2020;3:262-76.
- [Google Scholar]
- The effect of platelet rich plasma frequency on early stage knee osteoarthritis. Ege Tıp Bilimleri Dergisi. 2021;3:13-9.
- [PubMed] [Google Scholar]
- Short-term clinical results of intra-articular PRP injections for early osteoarthritis of the knee. Int J Surg. 2017;42:117-22.
- [CrossRef] [PubMed] [Google Scholar]







