Translate this page into:
Thyroid Malignancy in Multinodular Goiter: A Prevalence Study in a High-Volume Tertiary Care Center
*Corresponding author: Serbin Mohammed, MBBS, MS, Assistant Professor, Department of General Surgery, Government Medical College, Trivandrum 695011, Kerala, India. drserbin@yahoo.com
How to cite this article: Beena SL, Govindan U, Mohammed S. Thyroid malignancy in multinodular goiter: A prevalence study in a high-volume tertiary care center. Int J Recent Sur Med Sci, doi: 10.1055/s-0043-1761501
Abstract
Introduction
Goiter is one of the most common endocrine neoplasms found globally and its incidence varies in each country. Evaluation includes clinical, laboratory, radiological, and pathological tests to rule out malignancy. Surgery may be indicated in cases when the patient develops compressive symptoms, risks of malignancy, or cosmetic deformity. Thyroid malignancies account for only 1 to 2% of all malignancies. Irrespective of size, 9 to 13% of preoperative pathological evaluations revealed malignancy.
Objective
To study the prevalence of thyroid malignancy in patients presenting with multinodular goiter (MNG) undergoing thyroidectomy in the Department of General Surgery, Government Medical College, Thiruvananthapuram, India.
Material and Methods
This prevalence study was conducted in the Department of General Surgery, Government Medical College, Thiruvananthapuram, India, for a year, between March 2017 and February 2018. All patients with MNG undergoing thyroidectomy in the Department of General Surgery during this period were selected. A total of 651 patients were included in the study after obtaining informed consent.
Results
A total of 651 patients were studied, out of which 91 patients (13.9%) had malignancy. Among the total, 529 were females and 122 were males. Total malignancies reported were 91 and in those, males were around 31.9% and females around 68.1%. But when comparing incidence of malignancy in MNG, it was found to be higher in males (23.8%) than females (11.7%). Out of 91 patients with malignancy, 77 patients were found to have papillary carcinoma thyroid. Most of the papillary carcinoma thyroid occurred between 41 and 50 years of age, although it can occur in younger patients too. Palpable cervical lymphadenopathy is seen in 34 cases (37.4%) of thyroid malignancies.
Conclusion
Proportion of thyroid malignancy in MNG at Government Medical College, Thiruvananthapuram, is 13.9%. Females are more commonly affected than males. Papillary carcinoma is the most common differentiated malignancy associated. Cervical lymph nodal metastasis is seen in 37.4% of thyroid malignancies. The risk of malignancy in MNG should not be underestimated as significant numbers of patients with thyroid malignancies present with MNG.
Keywords
MNG
Multinodular goiter
Papillary carcinoma thyroid
Thyroid malignancy
Introduction
Goiter is one of the most common endocrine neoplasms found globally and its incidence varies in each country.[1] It was estimated to be around 5 to 10% during the life time and its frequency increases with age.[2] Thyroid nodules can be classified as solitary, dominant, and multinodular goiter (MNG).[3] MNG describes a thyromegaly with multiple nodules. Evaluation includes clinical, laboratory, radiological, and pathological tests to rule out malignancy. Surgery may be indicated in cases when the patient develops compressive symptoms, risks of malignancy, or cosmetic deformity.[4] Thyroid malignancies account for only 1 to 2% of all malignancies. But the incidence of malignancy was considered to be lower in MNG than solitary nodules, as studies have reported 5 to 7% incidence. Irrespective of size, 9 to 13% of preoperative pathological evaluations revealed malignancy.[5] Malignancy has also been reported in subclinical nodules detected by ultrasonography (USG) and also during autopsy.[2] The number of incidence may rise when occult carcinomas are taken into account. Worldwide increase in malignancy may be due to ionizing radiation and sensitive diagnostic tools.[6] Papillary carcinoma thyroid was the most common malignancy in majority of the studies.[7]
Objective
The objective of our study was to know the prevalence of thyroid malignancy in a high-volume tertiary care center in South India and also to determine the type of malignancy associated in different age groups by histopathology after total thyroidectomy in Government Medical College, Thiruvananthapuram.
Methodology
This prevalence study was conducted in the Department of General Surgery, Government Medical College, Thiruvananthapuram, India, for a year, between March 2017 and February 2018. Institutional ethics committee clearance was taken prior to the study. All patients with MNG above the age of 12 years undergoing thyroidectomy in the Department of General Surgery during this period were selected. A total of 651 patients were included in the study after obtaining informed consent. Negative consent for the study and age less than 12 years were the exclusion factors. Confidentiality of all participants was maintained. Questionnaires, case records, and histopathology reports were used to study individual cases. Using the data collected, proportion of malignancy in MNG was calculated. Various factors such as age, sex, and presence of cervical lymph nodes were also taken into account and their statistical association with thyroid malignancies was entered in structured data sheet, which includes all the variables, and analyzed using chi-square test.
Results
A total of 651 patients were studied with MNG in the Department of General Surgery, Government Medical College, Thiruvananthapuram, out of which 13.9% (91 patients) had malignancy and 86.1% (560 patients) had benign thyroid disease [Figure 1].
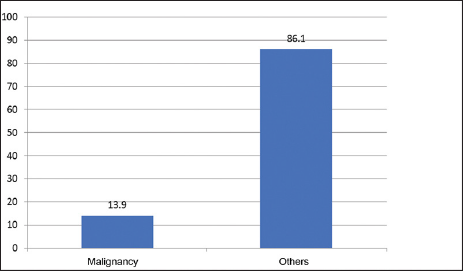
- Percentage distribution of malignant and benign cases in study population.
Among the 651 patients who were studied, 529 were females and 122 were males. Male: female ratio was calculated to be around 1:4 [Table 1].
Male (n = 122) |
Female (n = 529) |
Total (n = 651) |
||||
|---|---|---|---|---|---|---|
Thyroid lesions |
Frequency |
Percentage (%) |
Frequency |
Percentage (%) |
Frequency |
Percentage (%) |
Colloid goiter |
82 |
20.4 |
319 |
79.6 |
401 |
100.0 |
Thyroiditis |
11 |
6.9 |
148 |
93.1 |
159 |
100.0 |
Papillary carcinoma |
25 |
32.5 |
52 |
67.5 |
77 |
100.0 |
Follicular variant of papillary |
1 |
20.0 |
4 |
80.0 |
5 |
100.0 |
Follicular neoplasm |
2 |
28.6 |
5 |
71.4 |
7 |
100.0 |
Anaplastic/Medullary carcinoma |
1 |
50.0 |
1 |
50.0 |
2 |
100.0 |
From the above table, it is clear that there is a statistically significant association between gender and thyroid malignancies. Total malignancies reported were 91 and among those, males were around 31.9% and females 68.1%. But when comparing incidence of malignancy in MNG, it was found to be higher in males (23.8%) than females (11.7%).
Out of 91 patients with malignancy, 77 patients were found to have papillary carcinoma thyroid, followed by follicular carcinoma in 7 patients and follicular variants of papillary carcinoma in 5 patients. Others included one medullary carcinoma thyroid and one anaplastic carcinoma [Table 2].
Thyroid lesions |
Frequency (n = 651) |
Percentage (%) |
|---|---|---|
Colloid goiter |
401 |
61.6 |
Thyroiditis |
159 |
24.4 |
Papillary carcinoma |
77 |
11.8 |
Follicular variant of papillary |
5 |
0.8 |
Follicular carcinoma |
7 |
1.1 |
Anaplastic/Medullary carcinoma |
2 |
0.3 |
It was noted that there is a statistically significant association between thyroid malignancies and different age groups. Most of the papillary carcinoma thyroid occurred between 41 and 50 years of age, although it can occur in younger patients too. In our study, there were 3 patients aged between 13 and 20 years who were found to have papillary carcinoma with an incidence rate of 3.9% among malignancy. Follicular carcinoma and follicular variant of papillary carcinoma are commonly seen above 30 years of age. Others included one case of medullary carcinoma and one case of anaplastic carcinoma occurring in older patients between 61 and 70 years [Table 3 and Figure 2].
Thyroid lesions |
13–20 (y) |
21–30 (y) |
31–40 (y) |
41–50 (y) |
51–60 (y) |
61–70 (y) |
|---|---|---|---|---|---|---|
Count (%) |
Count (%) |
Count (%) |
Count (%) |
Count (%) |
Count (%) |
|
Colloid goiter |
15 (3.7) |
84 (20.9) |
202 (50.4) |
46 (11.5) |
40 (10.0) |
14 (3.5) |
Thyroiditis |
8 (5.0) |
24 (15.1) |
102 (64.2) |
20 (12.6) |
5 (3.1) |
0 (0.0) |
Papillary carcinoma |
3 (3.9) |
9 (11.7) |
20 (26.0) |
23 (29.9) |
17 (22.1) |
5 (6.5) |
Follicular variant of papillary |
0 (0.0) |
0 (0.0) |
1 (20.0) |
1 (20.0) |
1 (20.0) |
2 (40.0) |
Follicular neoplasm |
0 (0.0) |
0 (0.0) |
1 (14.3) |
1 (14.3) |
3 (42.9) |
2 (28.6) |
Others |
0 (0.0) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
2 (100.0) |
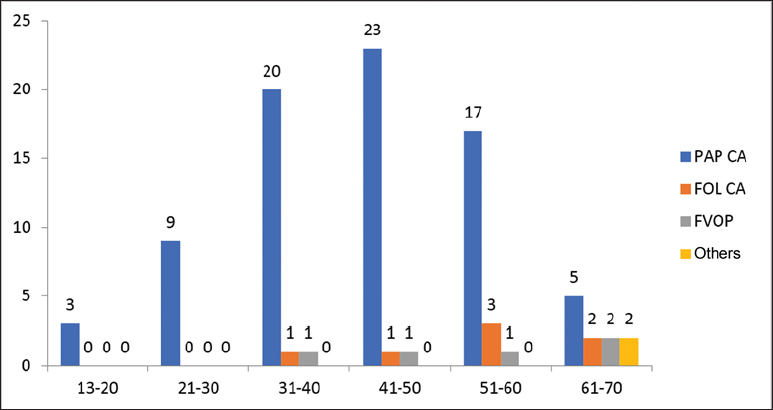
- Diagram representing age-wise distribution of thyroid malignancies in study population (x-axis: age interval; y-axis: percentage). FOL CA, Papillary Carcinoma; FVOP, Follicular Variant of Papillary Carcinoma; PAP CA, Follicular Carcinoma.
Palpable cervical lymphadenopathy is seen in 34 cases (37.4%) of thyroid malignancies. Out of 77 cases of papillary carcinoma thyroid, 29 cases are associated with lymph nodal metastasis (37.6%). Whereas for follicular carcinoma, out of seven cases only one case is associated with nodal metastasis. All five cases of follicular variant of papillary carcinoma are associated with cervical lymphadenopathy [Table 4].
Palpable cervical lymph nodes |
Frequency |
Percentage (%) |
|---|---|---|
No |
57 |
62.6 |
Yes |
34 |
37.4 |
Total |
91 |
100.0 |
Discussion
Goiter is the enlargement of the thyroid gland, and goiter having multiple distinct nodules in it is called MNG. Even though etiopathogenesis of MNG is not clear, mild iodine deficiency, impaired hormonal synthesis, increased iodine renal clearance, and increased immunoglobulins stimulating the thyroid have been considered to be the causative etiologies.[8]
MNG is detected in 4 to 7% of population by palpation and 30 to 40% by ultrasound of neck; incidence increases with age.[9-11] Almost 50% of palpable solitary nodules turn into MNG following ultrasound. Nodules less than 1 cm are barely palpable.[9,12] Unlike solitary nodules, MNG is thought to be a low risk for malignancy.[6] In any MNG with compressive symptoms, toxicity, and malignancy, surgery is the choice of management.[13]
Thyroid carcinomas are the most common endocrine tumors and its incidence varies around the world.[6] Papillary carcinoma is the most common malignancy documented.[7] The incidence of papillary carcinoma in MNG was 11.8% and among carcinoma was 84.6% in our study. This was consistent with most of the studies reported. In a review of literature by Vaisman et al in 2011, the authors reported 1.5 to 3% of malignancy in adolescence in the United States and Europe, which were similar to the findings in our study.[14] Any thyroid nodule should be viewed with suspicion if it is a dominant nodule with features such as rapid increase in size, hardness, irregularity, fixity along with cervical lymphadenopathy, recurrent laryngeal nerve palsy, male gender, and in extremes of ages.[6,15]
A high-frequency ultrasound of neck and fine needle aspiration cytology (FNAC) from the thyroid nodule are very much essential in the preoperative evaluation of MNG. The sonological findings suggestive of malignancy include microcalcification, irregular margins, complex echogenicity, local infiltration, and cervical nodal metastasis.[9] FNAC is a fast, inexpensive investigative tool to get cytological sample especially if done under USG guidance. Even though the specificity of FNAC is good, a negative sample does not exclude malignancy, especially for a clinically suspicious nodule.[9,13,16]
Papillary microcarcinoma is one subtype of papillary carcinoma that is 10 mm or less in greatest dimension. As per recent studies, micropapillary carcinoma if left untreated may progress similar to papillary carcinoma. Treatment is similar to papillary carcinoma, but it is very rarely diagnosed preoperatively and is commonly a histopathological finding after total thyroidectomy for MNG.[17-19]
Conclusion
From our study, we conclude that the risk of malignancy in MNG is not as low and it is quite significant. Prevalence of thyroid malignancy in MNG at Government Medical College, Thiruvananthapuram, is 13.9%. Females are more commonly affected than males. The highest frequency of benign thyroid lesions is found in the age group of 31 to 40 years and that of malignancy is between 41 and 50 years of age.
Papillary carcinoma is the most common differentiated malignancy associated with MNG. Cervical lymph nodal metastasis is seen in 37.4% of thyroid malignancies and is most commonly associated with papillary carcinoma thyroid.
Thus, the clinical importance of thyroid nodule is exclusion of malignancy. The risk of malignancy in MNG should not be underestimated as significant numbers of patients with thyroid malignancies present with MNG.
Acknowledgment
We would like to thank all the Surgeons at Department of General Surgery, Government Medical College, Thiruvananthapuram, for allowing us to analyze their cases.
References
- Evaluation and surgical treatment of solitary thyroid nodules. East Afr Med J. 1995;72:191-3.
- [PubMed] [Google Scholar]
- Minireview: discussion about the limit between normal thyroid goiter. Endocr Regul. 1999;33:39-45.
- [PubMed] [Google Scholar]
- The significance of nontoxic thyroid nodules. Final report of a 15-year study of the incidence of thyroid malignancy. Ann Intern Med. 1968;69:537-40.
- [CrossRef] [PubMed] [Google Scholar]
- Management of the solitary thyroid nodule. Oncologist. 2008;13:105-12.
- [CrossRef] [PubMed] [Google Scholar]
- Thyroid malignancy in multinodular goitre and solitary nodule. J R Coll Surg Edinb. 1995;40:310-12.
- [PubMed] [Google Scholar]
- Incidence of cancer in nodular goitres. Ann Acad Med Singap. 2007;36:241-3.
- [PubMed] [Google Scholar]
- The frequency of cold thyroid nodules and thyroid malignancies in patients from an iodine-deficient area. Cancer. 1987;60:3096-102.
- [CrossRef] [PubMed] [Google Scholar]
- Solitary thyroid nodule: diagnosis and management. Med Clin North Am. 1988;72:1177-211.
- [CrossRef] [PubMed] [Google Scholar]
- Solitary thyroid nodule. Comparison between palpation and ultrasonography. Arch Intern Med. 1995;155:2418-23.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of occult carcinoma in multinodular goiter using histopathological findings. Internet J Surg.. 2007;17:1-4.
- [Google Scholar]
- Thyroid carcinoma in children and adolescents-systematic review of the literature. J Thyroid Res. 2011;2011:845362.
- [CrossRef] [Google Scholar]
- Prevalence of malignancy in goitre–a review of 718 thyroidectomies. J Ayub Med Coll Abbottabad. 2009;21:134-6.
- [PubMed] [Google Scholar]
- The incidence of thyroid carcinoma in multinodular goiter: retrospective analysis. Acta Biomed. 2004;75:114-17.
- [PubMed] [Google Scholar]
- Thyroid cancer in toxic and non-toxic multinodular goiter. J Postgrad Med. 2007;53:157-60.
- [CrossRef] [PubMed] [Google Scholar]
- Thyroid papillary cancers: microcarcinoma and carcinoma, incidental cancers and non-incidental cancers - are they different diseases? Clin Endocrinol (Oxf). 2005;63:577-81.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment for microcarcinoma of the thyroid–clinical experience. Clin Nucl Med. 2007;32:279-81.
- [CrossRef] [PubMed] [Google Scholar]








