Translate this page into:
Medial Malleolar Fracture Management—A Comparative Study of Radiological Outcome between Open Reduction Internal Fixation and Closed Reduction Percutaneous Fixation
*Corresponding author: Sagar Venkataraman, MS, Associate Professor, Department of Orthopaedics, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research (SDUAHER) University, Kolar, Karnataka, India. drsagarnaik86@gmail.com
Abstract
Background
Medial malleolus fracture is commonly seen nowadays in orthopaedic practice. There are different modalities of treatment based on fracture pattern and socioeconomic status. Undisplaced fracture can be managed by cast application. Various surgical modalities of treatment are available in treating medial malleolus fracture like tension band wiring, cancellous screw or cortical screw fixation, plate fixation, Kirschner wire, and suture anchors. The purpose of our study was to evaluate radiological outcome of medial malleolus fracture managed with open reduction internal fixation and closed reduction percutaneous fixation.
Materials and Methods
Our study included 67 patients who met inclusion criteria and were divided into two groups. Group 1 included 52 patients with medial malleolar fractures cases and were treated with open reduction and internal fixation either by cancellous screw fixation or tension band wiring. Other 15 patients in group 2 were treated by closed reduction and internal fixation with cannulated cancellous screw. All postoperative patients were evaluated at 1st month, 2nd month, 3rd month, 6th month, and 1 year. We evaluated patient clinically and radiological union of fractures.
Results
In our study out of 67 patients there was male preponderance and average age was 46.55 years. Right-side fractures were more compared with left-side fractures. Most common mode of injury was road traffic accident. Transverse fracture pattern was more in number in our study. Average union time in group 1 was 13.46 weeks and group 2 is 15.14 weeks. Fracture union was 96.15% in group 1 and in group 2 was 93.33%.
Conclusion
In our study, average radiological union time in patients treated with open reduction internal fixation was early compared with percutaneous fixation. This could be due to direct visualization of fracture site and good approximation of fracture fragments in open reduction internal fixation technique.
Keywords
Cancellous screw
Medial malleolus
Open reduction
Percutaneous fixation
Tension band wiring
Introduction
Medial malleolus fractures are commonly seen nowadays.[1,2] There is increase in incidence following road traffic accident, twisting injury to ankle, assault, and fall from height. Medial malleolus fracture can present as isolated medial malleolus fracture or in combination with bimalleolar fracture, trimalleolar fracture, and pilon fracture. There are different modalities of treating medial malleolus fracture based on fracture pattern. Most of undisplaced isolated medial malleolus fracture can be treated conservatively in the form of below knee cast application.[3,4]
Unstable medial malleolus fracture or bimalleolar fracture is commonly managed by operative management.[5] Various surgical modalities have been described in literature for management of medial malleolus fracture. Various implants used in medial malleolus fracture fixation include cancellous screw,[6] tension band wiring,[7] plate fixation,[8] and suture anchors[9] have been used in medial malleolus fracture fixation. Surgical procedures can be open reduction internal fixation or closed reduction percutaneous fixation. In open reduction procedure, fracture site is exposed, fracture fragment is directly visualized, and fracture fragment is reduced and fixed with commonly used implants like partially threaded or fully threaded cancellous screw, tension band wiring, and plate fixation. But at times there are chances of wound complication and soft tissue damage.[10] In percutaneous approach, these complications are less but theoretically compared with open reduction; there may be inadequate anatomic reduction due to lack of direct fracture visualization. Some studies have shown that even in unstable medial malleolus fractures percutaneous screw fixation is excellent technique.[11,12]
The purpose of our study was to evaluate radiological outcome of medial malleolus fracture managed with open reduction internal fixation and closed reduction percutaneous fixation.
Materials and Methods
Study was conducted in tertiary referral hospital after obtaining ethical clearance from institution. Our study was retrospective study and study period was 2 years. Total 67 patients who met inclusion criteria were included in the study and were divided into two groups.
In group1, patients treated with open reduction internal fixation of medial malleolus fracture were included. In group 2, patients treated with closed reduction percutaneous fixation were included.
Group 1 consisted of 52 patients and group 2 consisted of 15 patients. We included isolated medial malleolus fracture and bimalleolar fractures cases in our study. All the cases were operated by trained orthopaedic surgeons. We referred back case sheets, operative notes, and data of each patient.
Surgical technique: Open reduction and internal fixation
In open reduction technique, medial malleolus fracture was exposed with longer incision over fracture site, fracture was reduced by direct visualization, and based on intraoperative findings, fracture comminution and fracture fragments were reduced and fixed with either cannulated cancellous screw or tension band wiring technique. Fracture reduction was confirmed by intraoperative fluoroscopy.
Surgical technique: closed reduction and internal fixation
In closed reduction technique, fracture site was not exposed; using clamps or reduction methods, fracture was reduced, which was confirmed with intraoperative fluoroscopy; small incision was made below medial malleolus to pass guidewire, over that cannulated cancellous screw was inserted and fracture reduction was confirmed by fluoroscopy. In bimalleolar fracture cases, lateral malleolus fracture was fixed with plate.
Postoperative protocol
Sutures were removed on postoperative day 14. Patients were evaluated at 1st month, 2nd month, 3rd month, 4th month, 5th month, 6th month, and 1 year [Figures 1–6]. Immediately postoperative ankle was immobilized with below knee slab for 2 weeks, after suture removal slab was converted to below knee cast for another 4 weeks. Partial weight bearing on operated limb with the help of walker support and ankle mobilization was started after 6 weeks from surgery. Full weight bearing was started at the end of 3 months as pain tolerated by the patients. If there was delay in fracture union, then weight bearing was delayed by another 2 to 4 weeks
Inclusion criteria
Patients’ age group >18 years.
All patients with closed displaced isolated medial malleolus fracture and bimalleolar fracture.
Open fracture Gustilo Anderson type I.
Exclusion criteria
-
Pathological factures.
-
Nonunion.
-
Associated neurovascular injury.
-
Crush injury of ankle and foot.
-
Medial malleolus fracture patient medically unfit for surgery.
Results
In our study, mean age for group 1 and group 2 was 44.44 years and 48.66 years, respectively. There was male preponderance in both groups. Among causes of injury, road traffic accident was major cause in both groups. Side distribution right side was affected more compared with left side. Transverse fracture was more in both groups [Table 1].
Group 1 (open reduction internal fixation) |
Group 2 (closed reduction percutaneous fixation) |
p-value |
|
|---|---|---|---|
n = 52 |
n = 15 |
||
Age at surgery (y) |
44.4 (10.8) |
48.7 (14.4) |
0.221 |
|
Gender |
|||
Female |
2 (3.8%) |
6 (40.0%) |
<0.001 |
Male |
50 (96.2%) |
9 (60.0%) |
|
Side affected |
|||
Right |
28 (53.8%) |
8 (53.3%) |
0.972 |
Left |
24 (46.2%) |
7 (46.7%) |
|
|
Mode of injury |
|||
RTA |
37 (71.1%) |
10 (66.7%) |
0.059 |
Fall from height |
7 (13.5%) |
1 (6.7%) |
|
Slip and Fall |
8 (15.4%) |
2 (13.3%) |
|
Twisting injury |
0 |
2 (13.3%) |
|
|
Type of fracture |
|||
Transverse |
30 (57.7%) |
8 (57.1%) |
0.958 |
Oblique |
16 (30.8%) |
4 (28.6%) |
|
Vertical |
6 (11.5%) |
2 (14.3%) |
|
|
Type of injury |
|||
Closed |
47 (90.4%) |
13 (86.7%) |
0.917 |
Open |
5 (9.6%) |
2 (13.3%) |
|
|
Associated lateral malleolus injury |
|||
Present |
6 (11.5%) |
6 (40.0%) |
0.011 |
Absent |
46 (88.5%) |
9 (60.0%) |
Abbreviation: RTA, road traffic accident.
Clinical outcome among groups, in which excellent results were seen in (84.6%) in group 1 and (73.3%) in group 2, was not statistically significant. Average union time in group 1 and group 2 was 13 weeks and 16 weeks, respectively, which was statistically significant [Table 2].

- Immediate postoperative X-ray of open reduction internal fixation with cannulated cancellous screw fixation.
Statistical Analysis
Data was entered in Microsoft Excel and analyzed using EpiData Analysis software (Epidata Association, Odense, Denmark). Categorical variables such as gender, type of fracture, mode of injury, associated injury and outcomes such as radiological nonunion, presence of complications, and clinical outcomes were summarized as proportions (percentages). These proportions were compared between open reduction internal fixation and closed-reduction percutaneous fixation groups using chi-squared test. Continuous variable such as age of the patient was expressed as mean (standard deviation) and compared using unpaired t-test. Time for fracture healing was expressed as median (interquartile range) and was compared between the two groups using Wilcoxon rank sum test. A p-value less than 0.05 was considered statistically significant.
Discussion
In our study, we compared results of open reduction internal fixation (group 1) of medial malleolus fracture with closed reduction percutaneous fixation (group 2). Our primary objective was to evaluate radiological outcome between two groups. In group 1, average union time was 13 weeks and in group 2, average union time was 16 weeks and was statistically significant. Weinraub et al’s[13] study result showed that union of medial malleolus fracture at 8 weeks in open reduction internal fixation group was 92.4% and in closed reduction percutaneous fixation group was 71.9%. Weinraub et al’s[13] study also reported that delay in fracture union in percutaneous fixation group was soft tissue or periosteum interposition. They noted that in open reduction internal fixation soft tissue interposition was noted in 93.3%. In our study also, we found that there was periosteum interposition at medial malleolus fracture site in open reduction internal fixation, but we could not quantify percentage of cases in which periosteum interposition was seen due to lack of data inoperative notes. Theoretically in open reduction and internal fixation approach, fracture site is exposed and on direct visualization if periosteum interposition is seen it can be removed and fracture ends can be approximated well. Although in closed reduction and percutaneous approach intraoperative fluoroscopy confirmed satisfactory reduction, in subsequent follow up X-ray there was loss of reduction that resulted in delayed union in one patient and nonunion in one patient in group 2. In open reduction and internal fixation, delayed union was seen in one patient and nonunion was seen in two patients. Superficial skin infection was seen in six patients in group 1 and in two patients in group 2. Ankle stiffness was seen in three patients in group 1 and nil in group 2. There were no complications observed in 80% of study participants in group 1 and in group 2 no complications observed in 73% of study participants [Figure 7]. There was statistically not significant difference in both groups.
In our study, cannulated cancellous screw was used in 62.69% cases and tension band wiring was used in 37.31% compared with Ebraheim et al[14] study in which overall screws were used in 58.58%, tension band wiring construct used in 27.92%, plate in 6.3%, and Kirschner-wires in 7.2%. Based on fracture pattern, overall transverse fracture pattern was more that constituted 58%, compared with Ebraheim et al’s study[14] and Andrew et al’s study[15] where in transverse fracture accounted 75 and 58.58%, respectively.
Limitation of Study
Our sample size was small. Study was retrospective; here there would have been selection bias among surgeons in choosing patients for open reduction internal fixation and closed reduction percutaneous fixation and group was not controlled. There was heterogeneous study group involving isolated medial malleolus fracture, bimalleolar fracture, comorbidities in study group, and skin condition around ankle also important in comparing functional outcome between groups. Since there were heterogeneous group, functional outcome was not comparable between two groups. So, we have compared only radiological outcome in our study.
Scope of Our Article
There is dilemma in the existing literature which treatment method is better for medial malleolus fracture management. Our study might contribute to the existing literature.
Conclusion
In our study, open reduction and internal fixation technique showed better results in terms of radiological union compared with closed reduction percutaneous fixation. Our study concludes with current literature that in case satisfactorily reduction is not achieved intraoperative with closed reduction percutaneous technique, then we need to open fracture site, reduce fracture, and fix the fracture fragment to get better results in terms of radiological union of medial malleolus fracture.
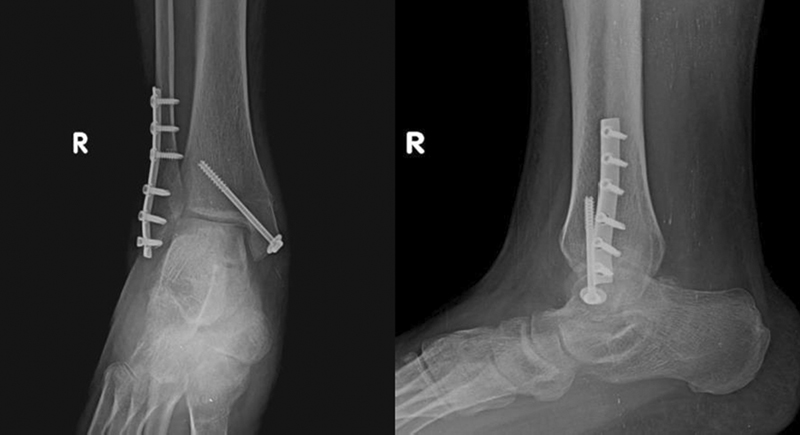
- Eight weeks postoperative X-ray of open reduction internal fixation with cannulated cancellous screw fixation.

- Immediate postoperative X-ray of open reduction internal fixation with tension band wiring.
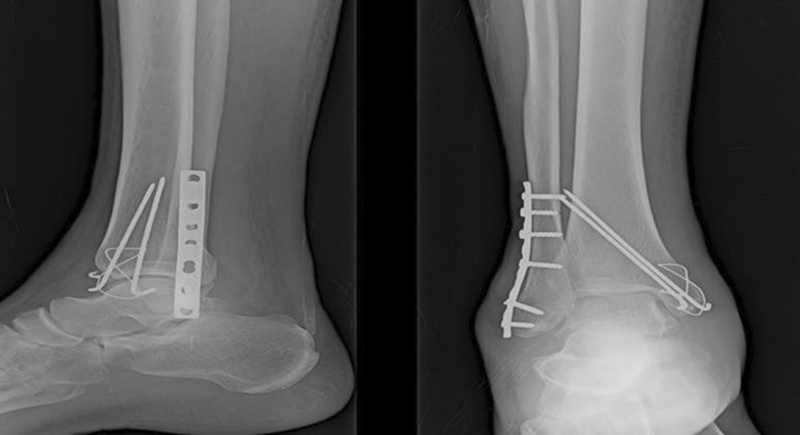
- Ten weeks postoperative X-ray of open reduction internal fixation with tension band wiring.

- Two weeks postoperative X-ray of closed reduction internal fixation with cannulated cancellous screw fixation.

- Sixteen weeks postoperative X-ray of closed reduction internal fixation with cannulated cancellous screw fixation.
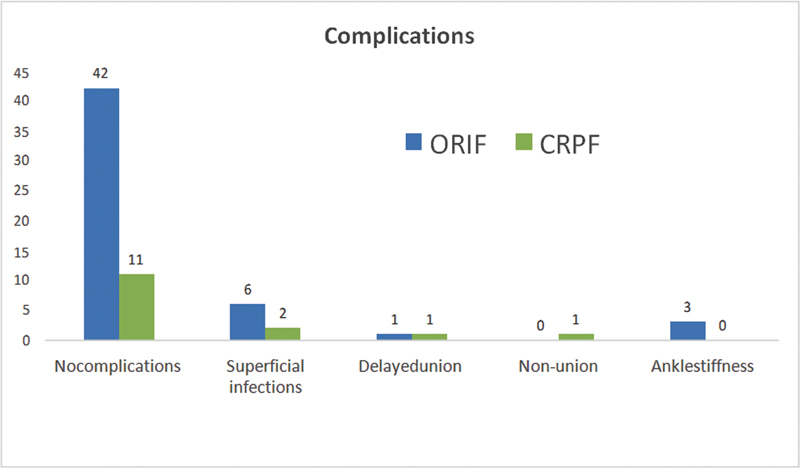
- Comparison of complications. CRPF, closed reduction percutaneous fixation; ORIF, open reduction internal fixation.
|
Group 1 (open reduction internal fixation) n = 52 |
Group 2 (closed reduction percutaneous fixation) n = 15 |
p-value |
|
|---|---|---|---|
Radiological union |
|||
Nonunion |
2 (3.8%) |
1 (6.7%) |
0.642 |
Median (IQR) time for union in weeks |
13 (12–16) |
16 (12–18) |
0.048 |
Complications |
|||
No complications |
42 (80.8%) |
11 (73.3%) |
0.533 |
Complication present |
10 (19.2%) |
4 (26.7%) |
|
Superficial infection |
6 (11.5%) |
2 (13.3%) |
|
Delayed union |
1 (1.9%) |
1 (6.7%) |
|
Nonunion |
2 (3.8%) |
1 (6.7%) |
|
Ankle stiffness |
3 (5.8%) |
0 |
Abbreviation: IQR, interquartile range.
Acknowledgments
None.
Conflict of interest
None declared.
Source of financial support
None.
References
- Epidemiology of osteoporotic ankle fractures in elderly persons in Finland. Ann Intern Med. 1996;125:975-8.
- [CrossRef] [PubMed] [Google Scholar]
- Adult ankle fractures–an increasing problem? Acta Orthop Scand. 1998;69:43-7.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of ankle fractures: non-operative and operative treatment. Clin Orthop Relat Res 1979:111-119.
- [PubMed] [Google Scholar]
- Conservative treatment of isolated fractures of the medial malleolus. J Bone Joint Surg Br. 2007;89:89-93.
- [CrossRef] [PubMed] [Google Scholar]
- Medial malleolus: Operative Or Non-operative (MOON) trial protocol - a prospective randomised controlled trial of operative versus non-operative management of associated medial malleolus fractures in unstable fractures of the ankle. Trials. 2019;20:565.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Lag screw fixation of medial malleolar fractures: a biomechanical, radiographic, and clinical comparison of unicortical partially threaded lag screws and bicortical fully threaded lag screws. J Orthop Trauma. 2012;26:602-6.
- [CrossRef] [PubMed] [Google Scholar]
- Tension band fixation of medial malleolus fractures. J Orthop Trauma. 1992;6:464-8.
- [CrossRef] [PubMed] [Google Scholar]
- Antiglide plating of vertical medial malleolus fractures provides stiffer initial fixation than bicortical or unicortical screw fixation. Clin Biomech (Bristol, Avon). 2016;31:29-32.
- [CrossRef] [PubMed] [Google Scholar]
- Technical tip: fixation of medial malleolar fractures using a suture anchor. Foot Ankle Int. 2009;30:68-9.
- [CrossRef] [PubMed] [Google Scholar]
- Soft tissue problems in ankle fractures treated surgically. A prospective study of 154 consecutive closed ankle fractures. Injury. 2003;34:928-31.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous screw fixation of unstable ankle fractures in patients with poor soft tissues and significant co-morbidities. Foot Ankle Surg. 2017;23:16-20.
- [CrossRef] [PubMed] [Google Scholar]
- Miniarthrotomy assisted percutaneous screw fixation for displaced medial malleolus fractures - a novel technique. J Clin Orthop Trauma. 2014;5:252-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Comparison of medial malleolus fracture healing at 8 weeks after open reduction internal fixation versus percutaneous fixation: a retrospective cohort study. J Foot Ankle Surg. 2017;56:277-81.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of surgical techniques of 111 medial malleolar fractures classified by fracture geometry. Foot Ankle Int. 2014;35:471-7.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of open reduction and internal fixation versus closed reduction percutaneous fixation for medial malleolus fractures. J Am Acad Orthop Surg. 2017;1:e048.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]








