Translate this page into:
A Case of Primary EAC Cholesteatoma Extending into Antrum with Normal Middle Ear
*Corresponding author: Siddhartha Shrivastava, Department of ENT and Head & Neck Surgery, School of Medical Sciences and Research, Sharda University, Noida 201310, Uttar Pradesh, India. drsshrivastava@gmail.com
How to cite this article: Shrivastava S, Kalra R, Somyagupta S, Pathak VK, Nayak P, Shukla S. A Case of Primary EAC Cholesteatoma Extending into Antrum with Normal Middle Ear. Int J Recent Surg Med Sci. 2024;10:S91-5. doi: 10.1055/s-0043-1761458
Abstract
A cholesteatoma is a three-dimensional sac lined by keratinized squamous epithelium containing desquamated keratinized epithelial cell which secretes enzymes that have the tendency to expand and erode the bony structure underlying it and cause intracranial and extracranial complications. This cystic mass is in an abnormal location such as the middle ear, the petrous apex, or the external auditory canal (EAC). It is mostly found in the middle ear and rarely in the EAC. Here we have reported a rare case of unilateral primary EAC cholesteatoma with mild hearing loss in a middle-aged male.
We have reported a case of a 34-year-old male with complaints of right-sided ear discharge and right-sided decreased hearing for the last 5 to 6 years. On examination, right ear EAC was found to be dry, and a sac was observed in posterior wall extending to mastoid present with clear attic, and intact retracted tympanic membrane that was then followed by radiological evaluation to establish the diagnosis of EAC cholesteatoma. This was surgically treated and ear was cleared of all disease. Patient’s symptoms improved postoperatively.
Primary EAC cholesteatoma with disease-free middle ear is a rare finding and there is very less definitive literature available on the pathogenesis of the same.
Keywords
External auditory canal cholesteatoma
Normal middle ear
Middle-aged male
INTRODUCTION
The term “Cholesteatoma” was coined by Johannes Muller in 1838, whereas external auditory canal cholesteatoma (EACC) was first described in 1850 by Toynbee.[1]
A cholesteatoma is a three-dimensional sac lined by keratinized squamous epithelium containing desquamated keratinized squamous epithelial cell which secretes enzymes that have the tendency to expand and erode the bony structure underlying it and cause intracranial and extra cranial complications. This cystic mass is in an abnormal location such as the middle ear, the petrous apex, or the EAC. It is mostly found in the middle ear and rarely in the EAC.[2]
EACC can be primary, acquired secondary to trauma, surgery or chronic inflammation or arise spontaneously.[3] In primary EACC, keratin is derived from sac involving the bone of ear canal with bony fragments within and random deep keratin inside the lumen of ear canal usually with a normal tympanic membrane (TM).[4]
Patients with EACC are generally older and often present with unilateral disease with otorrhea, dull pain, and normal hearing or mild hearing loss in rare cases.[3] Primary EACC has been estimated as 1 in 1000 new otological cases, whereas bilateral cases account for 1 in 6 to 12 cases[5]
EACC should be differentiated from other condition such as keratosis obturans, benign necrotizing otitis externa, malignant necrotizing otitis externa, and medial canal fibrosis.
The hallmark of cholesteatoma on imaging is the homogenous, erosive soft tissue mass with scalloped bone in EAC that occurs predominantly in inferior and posterior EAC with flecks of bone within the lesion in 50% of the cases.[2]
There are two staging systems for EACC:
-
Based on preclinical disease (Nairn et al.)[6]
Stage I—Epithelial hyperplasia
Stage IIa/b—Periostitis hyperplasia with erythema (a) or denuded but not eroded bone(b)
Stage III—Canal wall erosion and bony sequestrum
Stage IV—Invasion into adjacent structures—Mastoid (M), skull base and sigmoid sinus (S), temporomandibular joint (J), facial nerve canal (F)[6]
-
Based on clinical and radiological finding (Shin et al.)[7].
Stage I—Limited to EAC.
Stage II—Invades the TM as well as ear canal.
Stage III—Creates a defect of EAC and involves the cortex of mastoid bone.
Stage IV—Involves areas beyond the temporal bone.
This classification also includes treatment suggested below:
With local care or canaloplasty
With canaloplasty and tympanoplasty
With above and mastoidectomy and canal wall reconstruction
With removal of cholesteatoma using various techniques.[7]
Here we have reported a case of unilateral stage III primary EACC with mild hearing loss in a middle-aged male.
CASE REPORT
A 34-year-old male presented to the ENT outpatient department of a tertiary healthcare center with complaints of right-sided ear discharge and right-sided decreased hearing for the last 5 to 6 years. The right-sided ear discharge was nonprogressive in nature, occurred intermittently, yellow in color, nonfoul smelling, nonblood stained, mucopurulent in consistency, scanty in amount with no relieving, or exaggerating factors.
There was accompanying right-sided decreased hearing that was gradual in onset, initially mild but later progressed to moderate, with no fluctuation in different head position.
There was no history of dizziness or increase in degree of hearing loss in crowded places. There was no history of pain, trauma, right ear surgery, ringing sensation in either ear, headache, associated diplopia, or facial pain. There was no history of nasal discharge, difficulty breathing, or any allergic symptoms. He did not have any history of fever or recent trauma. There was no history of any facial swelling or weakness. He had history of undergoing type III tympanoplasty under general anesthesia of left ear on 7/10/2020 that was uneventful.
On examination, he was average built, well hydrated, conscious, and oriented to time place and person. All his vitals were stable and there were no obvious findings that could be appreciated on systemic examination. On local examination, externally the preauricular, auricular, and postauricular regions were found to be normal and there were no malformations or tenderness bilaterally. Right ear EAC was found to be dry, with a sac observed in posterior wall extending to mastoid, with a clear attic. On otomicroscopic examination, intact TM was observed that was retracted and touched the incus but not adherent to it, pink colored, with no polyp or granulation, foreshortened handle of malleus (HOM) [Figure 1]. Facial nerve examination was normal. Fistula sign was negative. On tuning fork examination, Weber’s test was lateralized to left, Rinne’s test was positive with only 1,024 Hz bilaterally, ABC and Schwabach’ tests were same as examiner. Ophthalmology evaluation was done to assess the vision that was normal.

- Intact tympanic membrane with mild retraction.
Pure tone average showed minimal conductive hearing loss (CHL) of 25 dB (decibel) in right ear and mixed CHL in left ear of 35dB. Radiological imaging was done for further evaluation. High-resolution computed tomography scan of temporal bone clarified our findings. It showed soft tissue density within B/L middle ear cavity and mastoid air cell [Figures 2-4]. TM perforation on left and intact TM on right with paucity of B/L mastoid air cells were found.
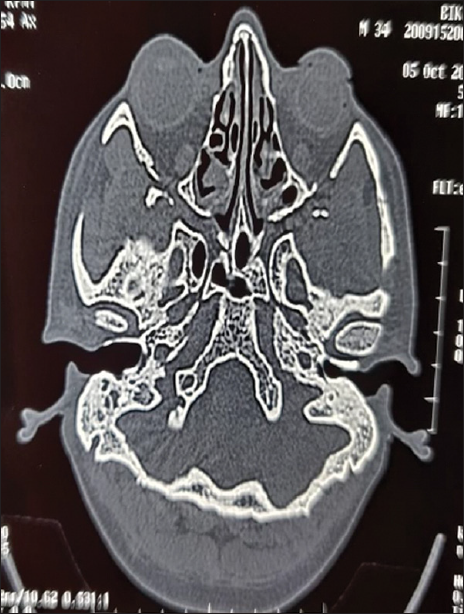
- High-resolution computed tomography temporal bone axial cut showing bony erosion posteriorly in external canal.
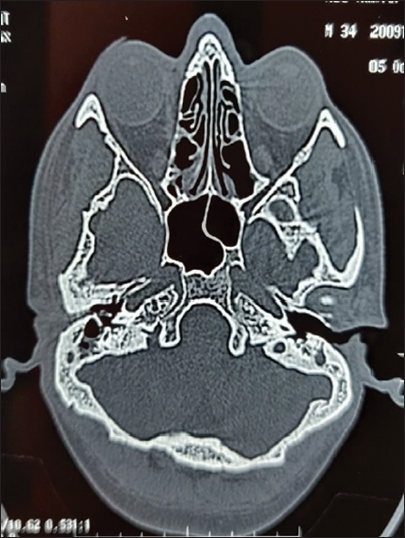
- High-resolution computed tomography temporal bone axial cut showing extent of external wall bony erosion inferiorly.
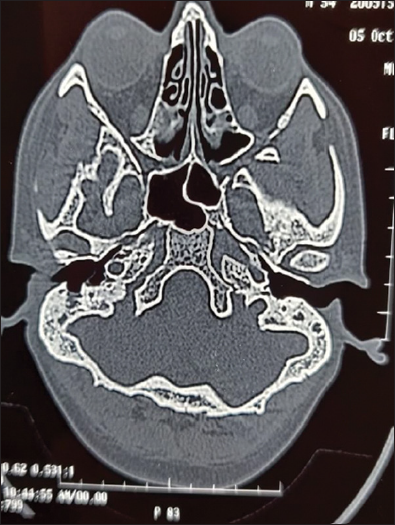
- High-resolution computed tomography temporal bone axial cut showing homogenous, erosive soft tissue mass with scalloped bone in external auditory canal (EAC) occurring predominantly in inferior and posterior EAC.
After diagnosis, the patient was taken up for right ear modified radical mastoidectomy with complete removal of EACC under general anesthesia after appropriate preanesthetic clearance [Figure 5].
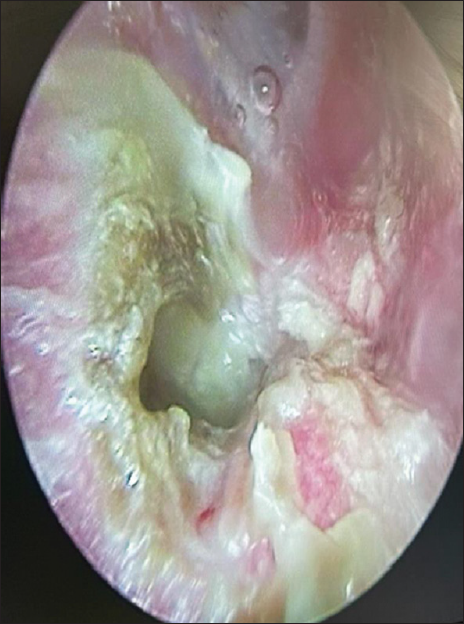
- Attic cleared of all disease.
Intraoperative findings
Cholesteatoma sac in posterosuperior part of EAC [Figure 6] extending into antrum with no disease in middle ear and intact ossicles. Sinus tympani was clear and facial recess was intact and clear. Facial ridge was lowered, facial bridge was drilled, and epitympanum was inspected and turned out to be clear. Hypotympanic air cells were also identified. Haemostasis was achieved and right ear mastoid dressing was done. Postoperatively, the patient’s symptoms were alleviated.
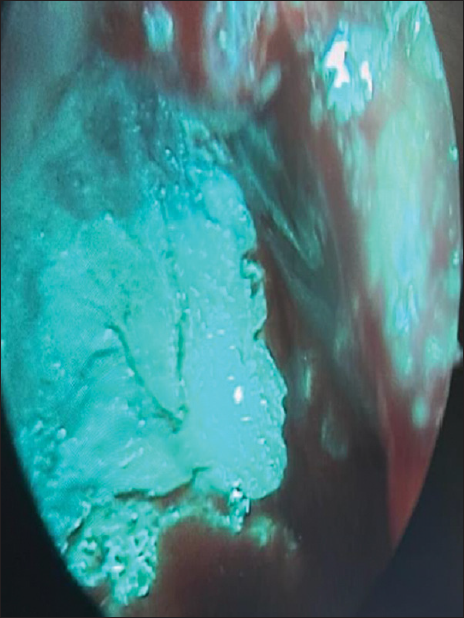
- Cholesteatoma flakes seen in the posterior sac of external auditory canal intra operatively after mastoid drilling.
DISCUSSION
EACC is responsible for 0.1 to 0.5% of otologic pathology. The etiology and pathogenesis are still poorly understood, but there are several theories about its origin, including localized periostitis, chronic inflammation of the EAC, failure in the epithelial cells clearance mechanisms, or the dehiscence of the petrotympanic fissure[2,8]
There is no exact frequency of recurrences reported in the literature so that long-term monitoring is recommended in all cases. By using open surgical techniques as wall-down mastoidectomy, microscopic exploration helps to detect early recurrence.
There are many reported series describing secondary cases of EACC but only a few reports of primary unilateral cholesteatomas.[3,9] Our patient was a primary case, as there was no history of previous ear disease, significant trauma, or surgery. Suggested risk factors for the development of primary EACC include the disruption of the local microcirculation by microtrauma from use of cotton swabs, smoking, or diabetes mellitus.[10]
EACC occurs more frequently among the elderly despite cases being reported in children and young adults.[11] Clinically, patients with EACC usually present with symptoms like chronic dull pain and otorrhea, but many patients can be amazingly silent or even asymptomatic.[3,12] Hearing loss is uncommon unless the cholesteatoma invades the middle ear or attic.
CONCLUSION
Primary cholesteatoma with normal middle ear is a rare finding and there is very less definitive literature available on the pathogenesis of the same. The true incidence of this disease is not known. Since clinical symptoms of EACC are not specific, it is, therefore, important to think about cholesteatoma when a patient presents with chronic otorrhea with intact TM. It is managed by surgical removal and repair of external canal and the precise limit of surgical removal is determined by the degree of bone necrosis and bony erosion and the surgeon’s judgment. Further work needs to be undertaken to determine the etiology and any relation to epithelial migration and vascular insufficiency.
References
- Specimens of Molluscum Contagiosum Developed in the External Auditory Meatus. Lond Med Gazzette. 1850;46:811.
- [Google Scholar]
- External Auditory Canal Cholesteatoma: Clinical and Imaging Spectrum. AJNR Am J Neuroradiol. 2003;24:751-6.
- [PubMed] [PubMed Central] [Google Scholar]
- The Pathologic Features of Keratosis Obturans and Cholesteatoma of the External Auditory Canal. Arch Otolaryngol. 1984;110:690-3.
- [CrossRef] [PubMed] [Google Scholar]
- Classification of the External Auditory Canal Cholesteatoma. Laryngoscope. 2001;115:455-60.
- [Google Scholar]
- Classification of External Auditory Canal Cholesteatoma by Computed Tomography. Clin Exp Otorhinolaryngol. 2010;3:24-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Keratosis Obturans and External Auditory Canal Cholesteatoma. Laryngoscope. 1980;90:383-91.
- [CrossRef] [PubMed] [Google Scholar]
- External Auditory Canal Cholesteatoma: Reassessment of and Amendments to Its Categorization, Pathogenesis, and Treatment in 34 Patients. Otol Neurotol. 2008;29:941-8.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric External Canal Cholesteatoma with Extensive Invasion into the Mastoid Cavity. Int J Pediatr Otorhinolaryngol. 2005;69:561-6.
- [CrossRef] [PubMed] [Google Scholar]








