Translate this page into:
Video Laryngoscopy as a Screening Tool for Laryngeal Changes in Chronic Smokers and Alcoholics
*Corresponding author: R. B. Namasivaya Navin, MBBS, MS ENT, Department of Otorhinolaryngology, Chettinad Academy of Research and Education, Chettinad Hospital and Research Institute, Chennai 603103, Tamil Nadu, India. navin.rajasekar@gmail.com
How to cite this article: Prabakaran S, Gowthame K, Namasivaya Navin RB, Raghvi A, Rajasekaran S. Video laryngoscopy as a screening tool for laryngeal changes in chronic smokers and alcoholics. Int J Recent Sur Med Sci, doi: 10.1055/s-0043-1761619
Abstract
Aim and Objectives
The main aim of this study was to identify the evolving, early changes, premalignant and malignant lesions of larynx among smokers, and alcoholics by video laryngoscopy and to correlate the duration, frequency, and amount of smoking and alcohol with spectrum of symptoms presented and laryngeal morphology.
Methods and Methodology
This study was prospective study done on a total of 165 patients who attended the department of otorhinolaryngology, at a tertiary care center in South India with various ENT complaints. Patients who were above 18 years of age from both sexes and gave history of smoking and alcohol consumption were included in this study irrespective of their complaints. All these patients underwent video laryngoscopy, which helped in early diagnosing various laryngeal lesions and screening tool for development of laryngeal lesions. Following diagnosis, patients were treated accordingly with lifestyle modifications and abstinence from smoking and alcohol. The primary outcome measure is screening for laryngeal morphology and secondary outcome measures are identifiable laryngeal benign and malignant lesions among smokers and alcoholics who required appropriate treatment.
Results
There was a significant association between the type of lesion and age group, type of lesion and smoking, and type of lesion and alcohol when compared with nonsmokers and non-alcoholics. As the pack years and amount of alcohol consumption increased, there was a significant increase in the severity and association of lesions.
Conclusion
We were able to diagnose a large number of laryngeal lesions that helped in the early detection of premalignant and malignant lesions and their early treatment. The patients who were diagnosed with premalignant and malignant changes underwent microlaryngeal excision of the lesion and were in close follow-up to detect any recurrence.
Keywords
Larynx
Smoking
Alcohol
Voice change
Introduction
Video laryngoscopy is commonly used most reliable, less expensive tool to visualize the upper airway.[1] It is an office-based procedure and useful in detecting benign, premalignant, early malignant lesions, its extent and secondary tumor in the larynx.
Among head and neck malignancies, carcinoma of the larynx is the most common malignancy, affecting mainly men.[2] The most common age of developing malignancy is above 60 years. There are many risk factors for laryngeal carcinoma among which tobacco smoking and alcohol ingestion are the independent risk factors in the development of laryngeal malignancy. It also directly correlates to the duration and amount of smoking and alcohol intake.
This prospective study was done to detect the early laryngeal lesions by doing video laryngoscopy among smokers and alcoholics.
Aim
To identify the evolving, early changes, premalignant and malignant lesions of larynx among smokers and alcoholics by video laryngoscopy.
Objectives
To correlate the duration, frequency and amount of smoking and alcohol, with spectrum of symptoms presented and laryngeal morphology.
Materials and Methodology
This study was a prospective study and was performed on patients who attended the department of otorhinolaryngology, at tertiary care center, with various ENT complaints, who were above 18 years of age from both sexes, and who gave history of smoking and alcohol consumption. The mean age of study, median, standard deviation and standard error of mean for age, smoking and alcohol were calculated and tabulated [Table 1]. Patients below 18 years of age, who were diagnosed with carcinoma larynx and secondaries of larynx, nonsmokers, and nonalcoholics, were excluded from the study. One-hundred sixty-five patients who attended ear, nose, throat outpatient department (ENT OPD) were included in the study if they were chronic smokers and alcoholics, irrespective of whether they had complaints related to throat and larynx. A tabulation was done for frequency of complaints that showed 40.61% without complaints, 31.52% with gastroesophageal reflux disease (GERD), 3.64% with foreign body sensation in throat, 4.85% with dysphagia, and 19.39% with voice change [Table 2].
Age |
Smoking pack years |
Alcohol amount |
|
|---|---|---|---|
Mean |
51.38 |
7.68 |
328.06 |
Standard deviation |
16.407 |
5.983 |
179.067 |
Median |
54.00 |
5.00 |
300.00 |
Standard error of mean |
1.277 |
0.466 |
13.940 |
The mean age of study, median, standard deviation, and standard error of mean for age, smoking, and alcohol were calculated and tabulated.
Complaints |
Number |
Percentage |
|---|---|---|
No complaints |
67 |
40.61 |
Gastritis, heartburn |
52 |
31.52 |
Foreign body sensation throat |
6 |
3.64 |
Dysphagia |
8 |
4.85 |
Voice change |
32 |
19.39 |
A tabulation was done for frequency of complaints that showed 40.61% without complaints, 31.52% with GERD, 3.64% with foreign body sensation in throat, 4.85%with dysphagia, and 19.39% with voice change.
After obtaining informed consent, detailed history of tobacco smoking and alcohol consumption, its duration, frequency, and amount were taken. Thorough clinical examinations including general and systemic examination along with ENT examination were performed.
After ruling out hypertensive, cardiac issues, and allergic history, local anesthetic, 10% lignocaine, was sprayed over the posterior pharyngeal wall to prevent gag reflex and discomfort of endoscopy. Rigid endoscope (75 degrees) was used to assess laryngeal status. Laryngeal structures like supraglottis, glottis, subglottis, and hypopharynx were assessed. The video laryngoscopic findings were recorded and correlated with duration, frequency, and amount of alcohol intake and smoking.
Results
The mean age of study, median, standard deviation, and standard error of mean for age, smoking, and alcohol were calculated and tabulated. [Table 1]. A tabulation was done for frequency of complaints that showed 40.61% without complaints, 31.52% with GERD, 3.64% with foreign body sensation in throat, 4.85% with dysphagia, and 19.39% with voice change [Table 2]. About 85.45% of patients underwent conservative management, while the remaining 14.55% underwent microlaryngeal excision of the lesions [Table 3]. Type of lesion and age group was correlated that shows a significant association between the type of lesion and age group with more lesions occurring in age group of 31 to 70 where there is more prevalence of smoking, alcoholism or both (p-value = 0.000) [Table 4]. There was not much significance there in association of gender and the lesions assessed [Table 5]. Type of lesion and duration of symptoms were correlated in which we found that there is more chronicity of symptoms in gastroesophageal reflux disease (GERD)/laryngopharyngeal reflux (LPR), while other lesions show duration less than 3 months [Table 6]. There is significant p-value of 0.000 seen showing that there is association between type of lesion and smoking when compared with nonsmokers. Ninety-six patients under less than 5 years category and the 48 patients under more than 5 years category were diagnosed with various lesions of larynx. Six patients had malignant changes at the initial assessment [Table 7]. Type of lesion and smoking pack years were calculated which shows there is significant association between type of lesion and smoking pack years (p-value = 0.000). Patients under category of 0 to 5 smoking pack years mostly were normal or presented with GERD/LPR. As the pack years increase, there is a significant increase in the severity and association of lesions, either benign, premalignant, and malignant [Table 8]. Type of lesion and alcohol consumption were correlated with patients who consumed alcohol for longer duration showed an increase in the lesions observed. The 102 patients under less than 5 years category and the 42 patients under more than 5 years category were diagnosed with various lesions of larynx [Table 9]. Type of lesion and amount of alcohol intake were correlated that shows there is a statistically significant association between type of lesion and amount of alcohol consumed (mL). Patients who consumed lesser amount of alcohol daily (upto360ml) mostly were normal or presented with GERD/LPR. As the quantity of alcohol consumption increases, there is a significant increase in the severity and association of lesions, benign, premalignant, and malignant (p-value = 0.000; [Table 10]). Type of lesion and synergistic effect of smoking and alcohol were correlated that revealed a significant value (p-value 0.000), thus proving the presence of synergistic action of smoking and alcohol in various benign and malignant lesions observed. In patients having substance abuse more than 5 years, 26 patients diagnosed with benign lesions were under close follow-up for the detection of malignancy, along with the 105 patients under less than 5 years category [Table 11].
Treatment |
Number |
Percentage |
|---|---|---|
Conservative |
141 |
85.45 |
MLS |
24 |
14.55 |
Abbreviation: MLS, microlaryngeal surgery.
Note: About 85.45% of patients underwent conservative management, while the remaining 14.55% underwent microlaryngeal excision of the lesions.
Age group |
Total |
||||||||
|---|---|---|---|---|---|---|---|---|---|
11–20 |
20–30 |
31–40 |
41–50 |
51–60 |
61–70 |
71–80 |
81–90 |
||
Type of lesion |
|||||||||
1_Normal |
0 |
14 |
23 |
8 |
10 |
13 |
3 |
0 |
71 |
2_GERD/LPR |
1 |
7 |
5 |
9 |
11 |
10 |
10 |
0 |
53 |
3_Reinke’s edema |
0 |
0 |
0 |
0 |
1 |
1 |
0 |
2 |
4 |
4_Vocalnodule |
0 |
0 |
0 |
0 |
4 |
3 |
0 |
0 |
7 |
5_Vocalpolyp |
0 |
0 |
1 |
2 |
1 |
2 |
0 |
0 |
6 |
6_Keratosis |
0 |
0 |
1 |
0 |
6 |
0 |
0 |
0 |
7 |
7_Leukoplakia |
0 |
0 |
1 |
2 |
0 |
3 |
1 |
0 |
7 |
8_CA/Pro.Growth |
0 |
0 |
0 |
0 |
0 |
3 |
3 |
0 |
6 |
9_VCgranuloma |
0 |
0 |
0 |
0 |
1 |
0 |
1 |
0 |
2 |
10_Papilloma |
0 |
0 |
0 |
0 |
1 |
0 |
1 |
0 |
2 |
Total |
1 |
21 |
31 |
21 |
35 |
35 |
19 |
2 |
165 |
p-Value = 0.000.
Type of lesion: Age group shows a significant association between the type of lesion and age group with more lesions occurring in age group of 31 to 70 where there is more prevalence of smoking, alcoholism or both type of lesion.
Sex |
Total |
||
|---|---|---|---|
Female |
Male |
||
Type of lesion |
|||
1_Normal |
20 |
51 |
71 |
2_GERD/LPR |
15 |
38 |
53 |
3_Reinke’s edema |
0 |
4 |
4 |
4_Vocalnodule |
1 |
6 |
7 |
5_Vocalpolyp |
3 |
3 |
6 |
6_Keratosis |
3 |
4 |
7 |
7_Leukoplakia |
3 |
4 |
7 |
8_CA/Prolif.Growth |
0 |
6 |
6 |
9_VCgranuloma |
1 |
1 |
2 |
10_Papilloma |
0 |
2 |
2 |
Total |
46 |
119 |
165 |
p-Value = 0.456; not much significance. There in association of gender and the lesions assessed.
Duration |
Total |
|||
|---|---|---|---|---|
Less than 3 mo |
More than 3 mo |
No complaints |
||
Type of lesion |
||||
1_Normal |
0 |
4 |
67 |
71 |
2_GERD/LPR |
0 |
53 |
0 |
53 |
3_Reinke’s edema |
4 |
0 |
0 |
4 |
4_Vocalnodule |
7 |
0 |
0 |
7 |
5_Vocalpolyp |
6 |
0 |
0 |
6 |
6_Keratosis |
7 |
0 |
0 |
7 |
7_Leukoplakia |
7 |
0 |
0 |
7 |
8_CA/Prolif.Growth |
6 |
0 |
0 |
6 |
9_VCgranuloma |
2 |
0 |
0 |
2 |
10_Papilloma |
2 |
0 |
0 |
2 |
Total |
41 |
57 |
67 |
165 |
p-Value = 0.000.
Type of lesion—duration: The table shows that there is more chronicity of symptoms in GERD/LPR, while other lesions show duration less than 3 months.
Smoking |
Total |
|||
|---|---|---|---|---|
Less than 5 y |
More than 5 y |
No smoking |
||
Type of lesion |
||||
1_Normal |
58 |
2 |
11 |
71 |
2_GERD/LPR |
34 |
15 |
4 |
53 |
3_Reinke’s edema |
0 |
4 |
0 |
4 |
4_Vocalnodule |
2 |
5 |
0 |
7 |
5_Vocalpolyp |
1 |
5 |
0 |
6 |
6_Keratosis |
1 |
6 |
0 |
7 |
7_Leukoplakia |
0 |
7 |
0 |
7 |
8_CA/Prolif.Growth |
0 |
6 |
0 |
6 |
9_VCgranuloma |
0 |
2 |
0 |
2 |
10_Papilloma |
0 |
2 |
0 |
2 |
Total |
96 |
54 |
15 |
165 |
p-Value = 0.000.
Smoking: There is significant p-value showing that there is association between type of lesion and smoking when compared with nonsmokers. Ninety-six patients under less than 5 years category and the 48 patients under more than 5 years category were diagnosed with various lesions of larynx. Six patients had malignant changes at the initial assessment.
Smoking pack years |
Total |
|||||
|---|---|---|---|---|---|---|
0–5 |
6–10 |
11–15 |
16–20 |
26–30 |
||
Type of lesion |
||||||
1_Normal |
61 |
8 |
0 |
2 |
0 |
71 |
2_GERD/LPR |
34 |
11 |
1 |
7 |
0 |
53 |
3_Reinke’s edema |
0 |
2 |
0 |
2 |
0 |
4 |
4_Vocalnodule |
3 |
4 |
0 |
0 |
0 |
7 |
5_Vocalpolyp |
2 |
4 |
0 |
0 |
0 |
6 |
6_Keratosis |
1 |
4 |
0 |
2 |
0 |
7 |
7_Leukoplakia |
0 |
3 |
0 |
3 |
1 |
7 |
8_CA/Prolif.Growth |
0 |
2 |
0 |
4 |
0 |
6 |
9_VCgranuloma |
0 |
1 |
0 |
1 |
0 |
2 |
10_Papilloma |
0 |
0 |
1 |
1 |
0 |
2 |
Total |
101 |
39 |
2 |
22 |
1 |
165 |
p-Value = 0.000.
Type of lesion—smoking pack years: This table shows there is significant association between type of lesion and smoking pack years. Patients under category of 0–5 smoking pack years mostly were normal or presented with GERD/LPR. As the pack years increase, there is a significant increase in the severity and association of lesions both benign, premalignant and malignant.
Alcohol |
Total |
|||
|---|---|---|---|---|
Less than 5 y |
More than 5 y |
No alcohol |
||
Type of lesion |
||||
1_Normal |
61 |
2 |
8 |
71 |
2_GERD/LPR |
35 |
15 |
3 |
53 |
3_Reinke’s edema |
0 |
4 |
0 |
4 |
4_Vocalnodule |
2 |
5 |
0 |
7 |
5_Vocalpolyp |
4 |
2 |
0 |
6 |
6_Keratosis |
0 |
7 |
0 |
7 |
7_Leukoplakia |
0 |
5 |
2 |
7 |
8_CA/Prolif.Growth |
0 |
6 |
0 |
6 |
9_VCgranuloma |
0 |
2 |
0 |
2 |
10_Papilloma |
0 |
2 |
0 |
2 |
Total |
102 |
50 |
13 |
165 |
p-Value = 0.003.
Type of lesion—alcohol: Patients who consumed alcohol for longer duration showed an increase in the lesions observed. The 102 patients under less than 5 years category and the 42 patients under more than 5 years category were diagnosed with various lesions of larynx.
Alcohol amount |
Total |
|||||
|---|---|---|---|---|---|---|
0–180 |
181–360 |
361–540 |
541–720 |
721–1000 |
||
Type of lesion |
||||||
1_Normal |
11 |
53 |
5 |
1 |
1 |
71 |
2_GERD/LPR |
5 |
36 |
7 |
3 |
2 |
53 |
3_Reinke’s edema |
0 |
1 |
1 |
1 |
1 |
4 |
4_Vocalnodule |
0 |
4 |
1 |
1 |
1 |
7 |
5_Vocalpolyp |
0 |
3 |
2 |
1 |
0 |
6 |
6_Keratosis |
0 |
3 |
2 |
2 |
0 |
7 |
7_Leukoplakia |
2 |
1 |
4 |
0 |
0 |
7 |
8_CA/Prolif.Growth |
0 |
3 |
2 |
0 |
1 |
6 |
9_VCgranuloma |
0 |
1 |
1 |
0 |
0 |
2 |
10_Papilloma |
0 |
0 |
1 |
1 |
0 |
2 |
Total |
18 |
105 |
26 |
10 |
6 |
165 |
p-Value = 0.000.
Type of lesion—alcohol amount This table shows there is a statistically significant association between type of lesion and amount of alcohol consumed (mL). Patients who consumed lesser amount of alcohol daily (up to 360 mL) mostly were normal or presented with GERD/LPR. As the quantity of alcohol consumption increases, there is a significant increase in the severity and association of lesions, benign, premalignant, and malignant.
Smoking and alcohol |
Total |
|||
|---|---|---|---|---|
Less than 5 y |
More than 5 y |
No synergism |
||
Type of lesion |
||||
1_Normal |
51 |
1 |
19 |
71 |
2_GERD/LPR |
38 |
8 |
7 |
53 |
3_Reinke’s edema |
2 |
2 |
0 |
4 |
4_Vocalnodule |
4 |
3 |
0 |
7 |
5_Vocalpolyp |
6 |
0 |
0 |
6 |
6_Keratosis |
2 |
5 |
0 |
7 |
7_Leukoplakia |
0 |
5 |
2 |
7 |
8_CA/Prolif.Growth |
0 |
6 |
0 |
6 |
9_VCgranuloma |
2 |
0 |
0 |
2 |
10_Papilloma |
0 |
2 |
0 |
2 |
Total |
105 |
32 |
28 |
165 |
p-Value = 0.000.
Type of lesion—Smoking and alcohol: There is a significant value, thus proving the presence of synergistic action of smoking and alcohol in various benign and malignant lesions observed. In patients having substance abuse more than 5 years, 26 patients diagnosed with benign lesions were under close follow-up for the detection of malignancy, along with the 105 patients under less than 5 years category.
Statistical analysis
Mean and standard deviation (SD) was calculated for continuous variables, and percentage was calculated for categorical variables. Chi-squared test was used to assess the statistically significant difference. SPSS version 20 was used and p-value <0.05 was considered significant.
The mean age is 51.38 with a SD of 16.407. The mean smoking pack years is 7.68 with a SD of 5.983 and median of 5; the mean alcohol amount is 328.06 with a SD of 179.06 and median of 300 [Table 1]. The most common complaints are gastritis, heart burns (31.52%); and 40.61% of patients were asymptomatic [Table 2]. About 85.45% of cases were managed conservatively [Table 3]. On applying chi-squared test, there is significant difference between type of lesion and age, duration of complaints, smoking, smoking pack years, alcohol, alcohol amount and smoking, alcohol synergism. On applying chi-squared test, there is no significant difference between type of lesion and sex.
Discussion
Laryngeal cancer stands one among the most commonly occurring malignancies in the fifth and sixth decade of life more among smokers and alcoholics. Alcohol and smoking have a synergistic effect on one another.[3] In this study, we identified that smokers and alcoholics were more likely to experience GERD, benign lesions such as vocal cord polyp, Reinke’s edema [Figure 1], vocal nodule [Figure 2] premalignant lesions such as keratosis and leukoplakia, and malignant lesions such as laryngeal malignancy [Figure 3] as the number of years of substance abuse increased [Tables 4 and 5].
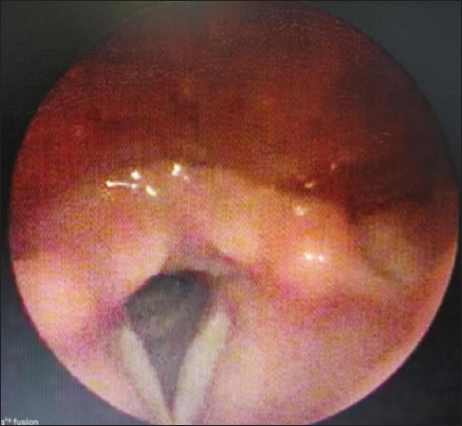
- Left vocal cord Reinke’s edema.

- Bilateral vocal cord nodule.

- Proliferative growth right vocal cord.
A by-product of alcohol named acetaldehyde damages cells locally, lowers T cell count, inhibits DNA repair enzyme activity, and increases the mucosal absorption of cigarette carcinogens. Alcohol also damages the liver, results in nutritional deficiencies, and compromises the immune system.[4] According to several research, moderate alcohol use (>1 to 4 drinks per day) is associated with a 1.5-fold higher risk. Heavy alcohol consumption (more than 4 drinks/day) is linked to a 2.5-fold increase in mortality. An average drink in the United States has approximately 14 g of pure alcohol in it, which is equivalent to 12 ounces (355 mL) of regular beer, 5 ounces (150 mL) of wine, or 1.5 ounces (45 mL) of spirit. Binge drinking on five or more days in a month is considered heavy drinking. According to a study by Islami et al, there is a 10-fold increase in risk for alcoholics compared with nonalcoholics and occasional drinkers.[5]
Most of the patients in this study fell into the category of daily alcohol use of up to 360 mL, and while they had a variety of complaints, the majority of them had either normal findings or GERD and LPR. An increased incidence of benign, premalignant, and malignant lesions was observed in patients who consumed more alcohol than 360 mL per day. Similar to this, we multiply the number of packs of cigarettes smoked each day by the number of years smoked to calculate the risk of smoking, keeping in mind that one pack of cigarettes comprises 20 cigarettes. This is used to determine the likelihood of acquiring lung and laryngeal cancer. According to a study conducted by Hashibe et al,[6] drinking alcohol has a multiplicative effect on smoking cigarettes.
Patients who fell into the category of 0 to 5 smoking pack years in this study were typically normal or had GERD/LPR. The severity and connection of benign, premalignant, and malignant lesions significantly increased with the pack years (Table 8). In addition to asbestos exposure, nicotine and alcohol use are other important risk factors for laryngeal cancer.[7]
According to studies done by Hocevar et al, excessive smoking causes the vocal cord mucosa to become dry and affects voice quality by triggering an inflammatory response that can result in chronic laryngitis, keratosis, and leukoplakia,[8-10] and alcohol consumption induces the vasodilation and edema of vocal cord mucosa. When compared with nonalcoholics, studies by Hedberg et al and Kjaerheim et al demonstrate that regular alcohol consumption has an independent link with benign laryngeal mucosal illness and raises the risk of malignant lesions of the larynx.[11–13] More significantly, rather than being independent, these behavioral issues are interrelated. When it comes to preventing, treating, and rehabilitating voice disorders, an examination of combined behavioral hazards may more accurately reflect the characteristics of the demographic group.[14] This study demonstrates that GERD/LPR symptoms are more chronic, whereas other lesions have durations of less than 3 months [Table 6].
The oldest method for examining the larynx, laryngopharynx, performing head and neck oncology operations, taking tissue samples from lesions, and performing microlaryngeal surgeries is direct laryngoscopy. Its drawbacks include the need for general anesthesia and the difficulty in obtaining the appropriate view of the airway due to previous radiation therapy, cervical spondylosis, obesity, and trismus. The flexible fiberoptic endoscopes, video laryngoscopes, and indirect laryngeal examination are the most frequently utilized procedures. The GlideScope (Verathon, Bothell, Washington, United States), C-MAC (KarlStorz, Tuttlingen, Germany), and King Vision are a few brands of video laryngoscopes that are frequently utilized (Ambu, Ballerup, Denmark). These video laryngoscopes enable to capture the results by combining an LED light source with a high-resolution video camera that is mounted to a monitor.[15] Stroboscopy can be used in conjunction with flexible fiber-optic laryngoscopy. With the use of this method, specific locations can be examined in more depth, and any lesion that is found can be captured on camera. This way the patients will have a better understanding of the disease process when they are shown the video recordings.[16]
It is also shown that transnasal flexible digital video laryngoscopes were shown to be safe and well tolerated. Additionally, it has been demonstrated that transnasal flexible digital video laryngoscopes are secure and well-tolerated. They benefit from great early diagnostic precision and a sizable reduction in diagnostic workup and treatment time. Office-based biopsy employing flexible digital video laryngoscopy is a safe, affordable, and efficient method of taking a biopsy and determining a histopathological diagnosis in cases of suspected laryngeal, oropharyngeal, or hypopharyngeal cancer. Thus, it significantly reduces the time needed for diagnostic testing in patients with laryngeal, oropharyngeal, or hypopharyngeal cancer and eliminates the requirement for a rigid laryngoscopy under general anesthesia.[17] In this study, all patients who were chronic smokers and alcoholics, who attended ENT OPD, underwent video laryngoscopy irrespective of whether they had complaints in throat or larynx.
Once a laryngeal pathology has been identified, it needs to be properly evaluated and managed. Laryngeal diseases can also be treated with CO2 LASER. Surgery performed for vocal cord lesions frequently might cause excessive scarring and voice loss. Premalignant laryngeal lesions have a significant likelihood of recurrence and malignant development even after first surgical therapy. The likelihood of developing cancer increases with higher degrees of dysplasia.[18] The use of high-dimensional video laryngoscopy in conjunction with narrow band imaging (NBI) permits earlier and more accurate for diagnosis of premalignant lesions, according to recent research by Vilaseca et al, Irjala et al, and Azam et al.[17–19]
It is now challenging for less experienced centers to use this technology because it is operator-dependent. This method also has a rather high learning curve and is limited by innate problems like subjectivity in interpretation, attention, and visual inspection skills. Thus, our study demonstrates that video laryngoscopy is a straightforward, affordable office treatment that is capable of quickly detecting laryngeal abnormalities.[19,20] We were able to identify a lot of laryngeal lesions when video laryngoscopy was employed as a screening technique for all persistent smokers and drinkers regardless of their complaints. As a result, it aided in the early detection and prevention of cancer as well as the development of early treatment options for individuals with laryngeal lesions. These individuals received advice on changing their lifestyles, quitting drinking, and using tobacco, and 32 of these patients underwent microlaryngeal excision of the lesion [Table 3].
Ninety-six patients in less than 5 years and 48 patients in more than 5 years of smoking who were diagnosed with various lesions of larynx were under close monitoring and follow-up [Table 7]. One-hundred two patients in less than 5 years and 42 patients in more than 5 years of alcohol consumption who were diagnosed with various lesions of larynx were under close monitoring and follow-up [Table 9]. This study shows there is a statistically significant association between type of lesion and amount of alcohol consumed (mL). Patients who consumed lesser amount of alcohol daily (up to 360 mL) mostly were normal or presented with GERD/LPR. As the quantity of alcohol consumption increases, there is a significant increase in the severity and association of lesions, benign, premalignant, and malignant [Table 10]. There is a significant value thus proving the presence of synergistic action of smoking and alcohol in various benign and malignant lesions observed. In patients having substance abuse more than 5 years, 26 patients diagnosed with benign lesions were under close follow-up for the detection of malignancy, along with the 105 patients under less than 5 years category [Table 11]. These patients were advised abstinence from smoking, lifestyle modifications, multivitamin supplementation, voice rest, speech therapy, and treatment of underlying cause.
Conclusion
Thus, by doing a screening video laryngoscopy for all smokers and alcoholics whether or not they had symptoms, we were able to detect benign and premalignant laryngeal lesions early. These patients were taken for microlaryngeal excision, and based on histopathological report, they will be treated accordingly and timely intervention can be done. So, this study shows that good prognosis may be attainable if biopsy is done early and this is of importance for therapeutic decisions during early stages of the tumor development or carcinoma in situ. Literature shows that in Western countries, the glottis is the most common subsite for laryngeal cancer. But in underdeveloped and developing countries like India, the supraglottis has been reported to be the most prevalent subsite and occurs in patients in sixth decade of life. So, these patients must be followed upon a regular basis and must be counselled for cessation of smoking and alcohol. Lifestyle modifications like reduction in caffeine consumption, cessation of smoking, alcohol consumption, increased exercise time, balanced healthy diet including fruits, and vegetables must be advised.
Conflict of interest
None declared.
References
- Videolaryngoscopy. Int J Crit Illn Inj Sci. 2014;4:35-41.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Smoking, alcohol drinking and cancer risk for various sites of the larynx and hypopharynx. A case-control study in France. Eur J Cancer Prev. 2004;13:165-72.
- [CrossRef] [PubMed] [Google Scholar]
- Scott-Brown’s Otorhinolaryngology and Head and Neck Surgery: 3 volume set CRC Press: Boca Raton, Florida; 2018 Jul 17
- [Google Scholar]
- Stell & Maran’s Textbook of Head and Neck Surgery and Oncology CRC Press: Boca Raton, Florida; 2011.
- [Google Scholar]
- Alcohol drinking and laryngeal cancer: overall and dose-risk relation–a systematic review and meta-analysis. Oral Oncol. 2010;46:802-10.
- [CrossRef] [PubMed] [Google Scholar]
- Contribution of tobacco and alcohol to the high rates of squamous cell carcinoma of the supraglottis and glottis in Central Europe. Am J Epidemiol. 2007;165:814-20.
- [CrossRef] [PubMed] [Google Scholar]
- The joint effect of asbestos exposure, tobacco smoking and alcohol drinking on laryngeal cancer risk: evidence from the French population-based case-control study, ICARE. Occup Environ Med. 2016;73:28-33.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for voice quality after radiotherapy for early glottic cancer. Radiother Oncol. 2009;93:524-29.
- [CrossRef] [PubMed] [Google Scholar]
- Hoarse voice in adults: an evidence-based approach to the 12 minute consultation. Clin Otolaryngol. 2009;34:54-58.
- [CrossRef] [PubMed] [Google Scholar]
- Hoarseness in adults AmFam Physician2009;80:363–370.16. AnC. Functional Dysphonia and Voice Therapy. Seoul, South Korea: Med-book; 2004.17
- [Google Scholar]
- Alcoholism and cancer of the larynx: a case-control study in western Washington (United States) Cancer Causes Control. 1994;5:3-8.
- [CrossRef] [PubMed] [Google Scholar]
- Laryngeal pathologies in older Korean adults and their association with smoking and alcohol consumption. Laryngoscope. 2013;123:429-33.
- [CrossRef] [PubMed] [Google Scholar]
- Utility of videolaryngoscopy for diagnostic and therapeutic interventions in head and neck surgery. Am J Otolaryngol. 2020;41:102284.
- [CrossRef] [PubMed] [Google Scholar]
- Laryngeal cancer: diagnosis and preoperative work-up. Otolaryngol Clin North Am. 2008;41:673-95. , v
- [CrossRef] [PubMed] [Google Scholar]
- Digital video laryngoscopy and flexible endoscopic biopsies as an alternative diagnostic workup in laryngo pharyngeal cancer: a prospective clinical study. Ann Otol Rhinol Laryngol. 2018;127:770-6.
- [CrossRef] [PubMed] [Google Scholar]
- The risk and interval to malignancy of patients with laryngeal dysplasia; a systematic review of case series and meta-analysis. Clin Otolaryngol. 2010;35:364-72.
- [CrossRef] [PubMed] [Google Scholar]
- Usefulness of office examination with narrow band imaging for the diagnosis of head and neck squamous cell carcinoma and follow-up of premalignant lesions. Head Neck. 2017;39:1854-63.
- [CrossRef] [PubMed] [Google Scholar]
- Pharyngo-laryngeal examination with the narrow band imaging technology: early experience. Eur Arch Otorhinolaryngol. 2011;268:801-6.
- [CrossRef] [PubMed] [Google Scholar]
- Deep learning applied to white light and narrow band imaging videolaryngoscopy: toward real-time laryngeal cancer detection. Laryngoscope.
- [Google Scholar]
- Histologic classification and grading of malignancy in carcinoma of the larynx. Acta Radiol Ther Phys Biol. 1973;12:1-8.
- [CrossRef] [PubMed] [Google Scholar]







