Translate this page into:
Cast Index as a Tool for Predicting Re-displacement after Closed Reduction and Cast Immobilization in Forearm Fractures in the Pediatric Age Group

*Corresponding author: Dr. Atul Anand, Department of Orthopaedics, Gajra Raja Medical College, Gwalior, Madhya Pradesh, India. atulanand98765@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singhal V, Anand A, Nand AA, Priyadarshi S, Gupta VK. Cast Index as a Tool for Predicting Re-displacement after Closed Reduction and Cast Immobilization in Forearm Fractures in the Pediatric Age Group. Int J Recent Sur Med Sci. 2023;9:89-96. doi: 10.25259/IJRSMS-2022-10-8
Abstract
Objectives
Forearm fractures are very common in all age groups. 81% of forearm fractures happen in children aged above 5 years with the peak of incidence between 9 and 12 years in females and 12 and 15 years in males. In children aged >9 years, remodeling potential is low and re-displacement of fracture after cast application remains a complication (as high as 25%). Quality of casting is an important modifiable risk factor for fracture re-displacement, which can be measured using the Cast index. The purpose of our study was to find out if Cast index should be used as a standard protocol after reduction for assessment of quality of cast.
Material and Methods
A total number of 40 patients were selected from outpatient department and trauma center based on inclusion and exclusion criteria. These patients were treated with below elbow (B/E) or above elbow (A/E) cast application. Follow-up was done radiologically using the Cast index at 0, 1, and 4 weeks of cast application. Out of 40 patients, 2 patients were remanipulated at one-week follow-up.
Results
Out of 40 cases of pediatric forearm fracture, 30 (75%) cases were male and 10 (25%) were female. Twenty-seven (67.5%) cases belonged to the 5- to 8-year age group. The mean age was 8.4 ± 2.79 years in males and 6.9 ± 2.23 years in females. The mean Cast index of the whole study was 0.802 ± 0.147 (range 0.48–1.21). The mean Cast index for proximal, middle and distal levels was 0.74, 0.85 and 0.76, respectively.
Conclusion
Cast index is an excellent marker and gives us an analogy about the quality of cast in pediatric forearm fractures. With proper use, it can also be used as a guiding stick for young orthopedicians. Thus, regular use of Cast index should be encouraged in all orthopedic centers; especially for pediatric forearm fractures.
Keywords
Pediatric forearm fractures
Cast index
Re-displacement
Closed reduction
Introduction
Forearm fractures are very common in all age groups, especially distal forearm fractures. Distal radius fractures are the most common limb fractures in childhood[1] (20–30% of all limb fractures).[2] 81% of forearm fractures happen in children aged above 5 years with the peak incidence between 9 and 12 years in females and 12 and 15 years in males.[3] The mechanism of trauma is mostly falling on the outstretched hand. Closed fractures of distal forearm in children are often treated with closed reduction and immobilization Leukostasis in a well-fitting plaster cast in our country with satisfactory results in majority of the patients. Forearm fracture in children heals quickly and mild to moderate displacement gets corrected by itself due to remodeling,[4] but in children aged above 9 years remodeling potential is low and re-displacement of fracture remains a complication (as high as 25%).[3] Due to re-displacement, wrist and hand functions are severely compromised including range of movement at wrist joint and grip power of hand. Previous studies have declared the initial displacement of the fractures to be the most important risk factor for re-displacement.[3,5,6] Other factors may be distance of fracture from the physis, angulation of the fracture, poor cast molding, oedema resolution whilst in the cast and inadequate initial reduction. Quality of casting is an important modifiable risk factor for fracture re-displacement, which can be measured by use of casting indices. The first and simplest index to be described is the Cast index described by Chess et al.[7] It is calculated by measuring the internal LATERAL diameter of cast (excluding Padding) and dividing it by the internal antero-posterior (AP) diameter of the cast (excluding padding), both at the level of fracture. It is measured after closed reduction and cast application in the radiograph.
Recent studies have shown that a Cast index of over 0.8 carries a significant risk of re-displacement.[8] Cast index is not being used consistently in clinical practice. Before accepting any plaster after a manipulation of forearm fractures, a rapid assessment by surgeons could be a very useful practice.[9] Given the benefits of this index and its simplicity of calculation, the question to be asked is, should it be used as a standard protocol after reduction for assessment of quality of cast and whether the applied cast requires close monitoring or revision. The hypothesis of this study is that Cast index will come out to be a good index in the 5- to 16-year age group as far as risk of re-displacement is concerned after forearm fractures.
Material And Methods
Sample Size: A total number of 57 patients were selected from outpatient department and trauma center randomly. Ten patients were lost to follow-up due to COVID lockdown. Four patients were excluded because of lack of complete follow-up. Three patients were excluded because of improper initial reduction and were treated with intramedullary nailing. Hence, a total of 40 patients fulfilled the criteria and were finally assessed. Out of 40 patients, 2 patients were remanipulated at one-week follow-up. After application of a new cast, these remanipulated patients were not followed further for the study. Selection was based on some inclusion and exclusion criteria.
Inclusion Criteria
Mono-osseous closed forearm fracture in forearm.
Bi-osseous closed forearm fracture in forearm.
Age 5–16 years.
Trauma history not more than 10 days.
Patient giving consent for examination and follow-up.
Exclusion Criteria
Refusal to consent.
Age Less than 5 years and more than 16 years.
Suspected pathological fracture.
Comminuted/compound/segmental fracture.
Patients who did not complete follow-up.
Patients who did not have complete radiographic documentation.
Unsatisfactory/failed initial reduction.
Intra-articular fractures.
Physeal injuries.
Methods: After the approval of the institutional ethics committee (IEC) [77/IEC- GRMC/2019], the study was carried out between October 2019 and November 2021. Written informed consent was taken from the guardian before including the child in the study.
The intervention protocol followed for this study is depicted in the form of a flow chart in Figure 1. For reduction, the children were kept NIL PER ORAL for a minimum of 6 hours as per the requirement of anesthetists. Proper history, vitals and examination of various systems were done before taking the children for reduction in Operation theater (OT). All the cases requiring reduction were done in the operating room under short IV sedation. Local anesthesia was not used. After induction, the patients were positioned supine and the fracture was manipulated and reduced under image intensifier into acceptable anatomical reduction as per the acceptable reduction criteria already set for the study [Table 1].[10] After acceptable reduction was achieved, the reduction was immobilized using an above elbow or below elbow cast. The reduction was checked under image intensifier. The position of the forearm was kept in mid-prone position for distal 1/3rd and middle 1/3rd fractures and in supination for proximal 1/3rd fractures. The elbow was flexed to 90 degrees in above elbow casts. An arm sling/pouch was given to all the cases after drying up of the Plaster of Paris cast. All the casts were applied with Plaster of Paris as the casting material and cotton wool as the padding material. Extra padding was given at bony landmarks like wrist and elbow. Knuckles and thumb were kept free to allow finger movements and movement at metacarpo-phalangeal joints. Remoulding was done to attain the contour of the limb. If acceptable reduction was not achieved as per the set criteria, intramedullary nailing was done in them to achieve the reduction.
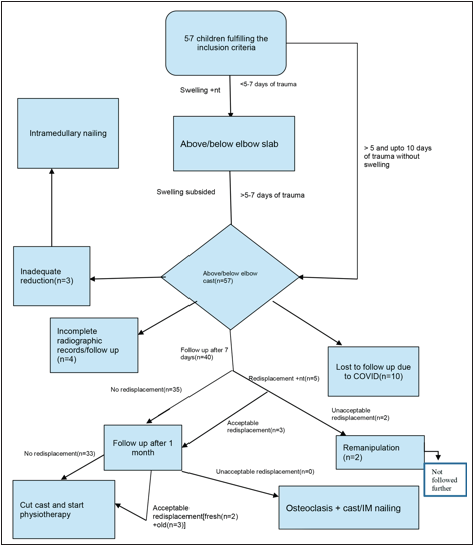
- Flow chart depicting the intervention protocols followed for this study.
| Patient age | Angulation | Bayonet apposition |
|---|---|---|
| Age 0–9 (0–8 girls, 0–10 boys) | <15° | Up to 1 cm |
| Age >9 (>8 girls, >10 boys) | <10° proximal/midshaft | Up to 1 cm |
| Age >9 (>8 girls, >10 boys) | <15° distal | Up to 1 cm |
Adapted from Noonan KJ, Price CT 1998 JAAOS
Once the cast hardened, true AP and true lateral x-rays were taken. While taking the x-ray, a 5-rupee coin with standard diameter of 23 mm[11] was placed alongside the forearm to standardize the calculations. The x-ray machine was kept perpendicular to the forearm so that the falling rays were perpendicular to the forearm. After giving proper post-casting care instructions, the patients were sent home and called for follow-up and radiographic imaging and calculation after seven days. Analgesics and calcium supplements were given to the patients.
Both the pre-reduction and immediate post-reduction x-rays were photographed on a view box and this photograph was then used to make the calculations [Figure 2]. The calculations were done with an application available on the android store by the name IMAGEMETER. Both the angles and the Cast index calculation in the immediate post-reduction were done using this application [Figures 3 and 4]. For standardizing the length calculation, the diameter of 5-rupee coin was used as a standard length of 23 mm.[11]
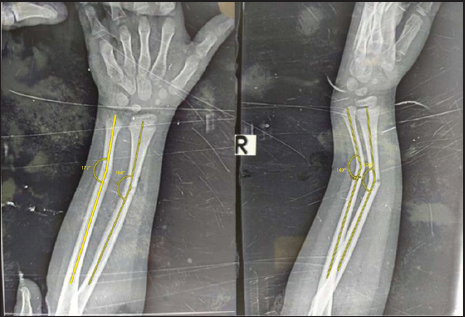
- Measurement of angulation in AP and lateral views pre-reduction.

- Calculating the Cast index just after reduction by measurements in AP and lateral view at the level of fracture.

- Calculating the angulation in AP and lateral view immediate post-reduction.
Re-displacement criteria were taken as an increase in angulation of >10 degrees in AP and/or lateral views or loss of adequate contact (at least one cortex in both AP and LATERAL views) between fracture fragments. The patients were then called for follow-up at the completion of one week of the cast [Figure 5]. If the re-displacement was too much to be accepted, remanipulation was done under image intensifier.

- Calculating the angulation in AP and lateral view at one week post-reduction.
Follow-up at one month consisted of addressing the problems and getting a new true AP and true lateral radiographs for calculation of degree of re-displacement, if any [Figure 6]. Calculations were again done using the same software. Re-displacement criteria remained the same. In the case of unacceptable re-displacement at this stage, osteoclasis or intramedullary nailing was kept as an option for correction of alignment.
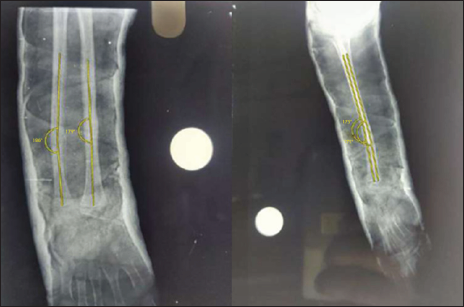
- Calculating the angulation in AP and lateral view at one month post-reduction.
Cast removal was done at one month and aided support to the forearm by crepe bandage was given for another two weeks. Meanwhile the patients were asked to carry out proper wrist and elbow physiotherapy. No functional outcomes were studied.
Mean Cast index in non-displaced and displaced groups was calculated and compared statistically.
Results
Out of 40 cases of pediatric forearm fracture, 30 (75%) cases were male and 10 (25%) cases were female. Majority of cases were male. Twenty-seven cases (67.5%) belonged to the 5- to 8-year age group, 7 (17.5%) belonged to the 9- to 11-year age group and 3 (7.5%) belonged to the 11–13 & >13-year age group, respectively. Majority of cases belonged to the 5- to 8-year age group. Out of 40 cases of pediatric forearm fracture, age group <7 years contained 7 females and 11 males, age group 8–10 years contained 2 females and 14 males, and age group > 10 years contained 1 female and 5 males. The mean age was 8.4 ± 2.79 years in males and 6.9 ± 2.23 years in females. In 17 (42.5%) cases, the left side was involved, whereas in 23 (57.5%) cases the right side was involved. Out of 40 cases of pediatric forearm fracture, 18 (45%) cases were distal 1/3rd fracture, 19 (47.5%) cases were middle 1/3rd fracture and 3 (7.5%) cases were proximal 1/3rd fracture. The mechanism of trauma in most of the patients was fall during play 28 (70%) followed by Road traffic accident (RTA) 7 (17.5%) followed by fall from bicycle 5 (12.5%) [Table 2].
| Non-Re-displacement group | Re-displacement group | p-value | |
|---|---|---|---|
| Number | 34 | 6 | |
| Age | 8.33 ± 2.80 | 6.57 ± 1.71 | 0.120 |
| Male:Female | 26:8 | 4:2 | 0.810 |
| Side (Right:Left) | 20:14 | 3:3 | 0.983 |
| Location of Fractures | |||
| Distal 1/3rd | 14 | 4 | 0.621 |
| Middle 1/3rd | 16 | 3 | |
| Proximal 1/3rd | 3 | 0 | |
| Type of Fractures | |||
| Single Bone | 16 | 3 | 0.787 |
| Both Bones | 17 | 4 | |
| Radius | 11 | 2 | 0.962 |
| Ulna | 5 | 1 | |
| Radius + Ulna | 17 | 4 | |
| Max. Angulation Shift in Antero-posterior | 4.36 ± 3.02 | 7 ± 6.06 | 0.012 |
| Max. Angulation Shift in Lateral | 4.24 ± 2.48 | 11.43 ± 1.62 | 0.000 |
| Mean Cast Index | 0.779 ± 0.124 | 0.910 ± 0.208 | 0.034 |
| Mean Cast index | Odds Ratio | ||
| >0.8 | 15 | 5 | 3 |
| £0.8 | 18 | 2 |
The mean Cast index of the whole study was 0.802 ± .147 (range 0.48–1.21). Ideal range for proximal 1/3rd fracture cannot be commented upon pertaining to the lesser number of cases with proximal 1/3rd fracture. Remanipulation was required in 2 (28.6%) of the total seven re-displacement cases. In our study, for the whole forearm, the value of Cast index > 0. 8 had sensitivity of 71 %, specificity of 55%, odds ratio of 3, negative predictive value of 90%, positive predictive value of 25% and accuracy of 58% for re-displacement evaluation [Tables 3 and 4]. The most common complication during the follow-up period was itching (22.5% cases), followed by cast breakage (5% cases). No other complications were noted. Post-cast cutting, the most common complication was wrist and elbow joint stiffness. P value < 0.05 was considered statistically significant.
| N | Mean cast index | Std. deviation | 95% confidence interval for mean | Minimum | Maximum | ||
|---|---|---|---|---|---|---|---|
| Lower limit | Upper limit | ||||||
| Distal 1/3rd | 18 | 0.76 | 0.10 | 0.71 | 0.81 | 0.54 | 0.97 |
| Middle 1/3rd | 19 | 0.85 | 0.17 | 0.77 | 0.93 | 0.48 | 1.21 |
| Proximal 1/3rd | 3 | 0.74 | 0.20 | 0.24 | 12.24 | 0.51 | 0.87 |
| Total | 40 | 0.80 | 0.15 | 0.76 | 0.85 | 0.48 | 1.21 |
| Measure | Mean cast index (>0.8) |
|---|---|
| Sensitivity | 71% |
| Specificity | 55% |
| Positive predictive value (PPV) | 25% |
| Negative predictive value (NPV) | 90% |
| False positive rate (FPR) | 45% |
| False negative rate (FNR) | 29% |
| Accuracy | 58% |
Discussion
In our study, out of the seven cases of re-displacement, five cases (71.4 %) occurred within one week of follow-up and only two cases (28.6%) occurred after two days of cast immobilization. The correlation between timing of re-displacement and re-displacement came out to be statistically significant (p = 0.01). Re-displacement is more likely to occur before the formation of a soft callus, which acts as a bridge to prevent further re-displacement. Only two (28.5%) out of the seven cases required remanipulation and both of these cases had redisplaced within one week of initial reduction. This further suggests that further re-displacement gradually decreases once the cast gets older leading to formation of soft callus and finally hard callus. Haddad et al.[12] found that experienced surgeons had lower rate of re-displacement. Arora et al.[13] and Yang et al.[14] found the correlation to be insignificant in their study. Seven patients (17.5%) showed re-displacement. Out of these 7, 2 patients (5% of total) required remanipulation. The re-displacement rate is comparable to studies by Malviya et al.[9] Alemdaroğlu et al.[6] Yang et al.[14] and Mazzini et al.[16]
All of these studies used different parameters of re-displacement unlike ours, so comparison with them is of no significance. The two patients that required remanipulation had re-displacement which was unacceptable as per our reduction criteria and hence were remanipulated and a new cast was applied with proper reduction. The mean Cast index of the whole study was 0.802 ± 0.147 (range 0.48–1.21). The mean Cast index in the non-re-displacement group was 0. 779 ± 0.124 (range 0.48–0.98) and in the re-displacement group, it was 0.910 ± 0.208 (range 0.54–1.21). The mean distribution of Cast index value among re-displacement group and non-re-displacement group was found to be statistically significant (p = 0.034) [Table 5]. Our study including the whole forearm and including both bones as well as isolated bone fracture shows that with increasing value of Cast index, the chances of re-displacement are more. All the cases with Cast index more than 1 got redisplaced.
| Previous studies | Mean cast index of non-re-displacement group |
|---|---|
| Sheikh et al.[19] (distal forearm) | 0.77 |
| Chess et al.[7] (distal forearm) | 0.72 |
| Turgut et al.[20] (distal radius) | 0.775–0.875 |
| Basavarajanna et al.[21] (middle 1/3rd forearm) | 0.75 |
| Malviya et al.[9] (distal forearm) | 0.72 |
| Ajmera et al.[18] (whole forearm) | 0.852 |
| Our study (whole forearm) | 0.779 |
Other Cast indices such as gap index[15–17] and three point index[6,17] have proven to be better than Cast index in some studies. But their calculation is very cumbersome and hence reduces their use in a trauma setting. Cast index, however, is very easy to calculate and analyze and has the potential of becoming an effective tool for checking the quality of forearm cast normally applied in pediatric closed forearm fractures. Singh S et al.[15] in their study proved the efficacy of using Cast index in decision-making even by senior consultants and registrars.
In our study, the mean Cast index for distal 1/3rd, middle 1/3rd and proximal 1/3rd level was 0.76 ± 0.10, 0.85 ± 0.16, 0.74 ± 0.19, respectively. In the study by Ajmera et al.,[18] this value was 0.80, 0.86 and 0.92, respectively. In the study by Sheikh et al.,[19] mean Cast index in distal ½ and proximal ½ was 0. 76 and 0.83, respectively.
The value of Cast index increases as we move from distal to proximal because of increase in muscle mass and hence change in cross-section of forearm from elliptical to cylindrical.
In our study, the mean shift in angulation in AP view in the re-displacement group was 7° ± 6.06. It was 4.36 ± 3.02 in the non-re-displacement group. The correlation between these two groups was significant (p = 0.012). Similarly, the mean shift in angulation in lateral view in the re-displacement group was 11.43° ± 1.62. It was 4.24 ± 2.48 in the non-re-displacement group. The correlation between these two groups was statistically significant (p = 0.000). Malviya et al.[9] in their study also found out the correlation to be statistically significant.
In our study, for the whole forearm, the value of Cast index 0.8 as a cut-off was taken and sensitivity of 71%, specificity of 55%, odds ratio of 3, negative predictive value of 90%, positive predictive value of 25% and accuracy of 58% suggests that Cast index 0.8 for forearm fracture is a landmark to predict re-displacement. In a study by Malviya et al.,[9] on distal 1/3rd radius fractures, the cut-off value 0.8 showed sensitivity of 48%, specificity of 88%, positive predictive value of 52.1%, negative predictive value of 83.5%, accuracy of 78% and odds ratio of 6.8. Alemdaroğlu et al.[6] in their study on distal radial fractures found the cut-off point of 0.8 to be 63.2% sensitive, 52.4% specific, with negative predictive value of 82.5% and positive predictive value of 28.6%. Arora et al.[13] in their study found the cut-off 0.81 for the whole forearm to be 69.2% sensitive, 76% specific and odds ratio of 9.
In our study the range of Cast index to include 95% of cases came out to be 0.76–0.85 for the whole forearm fracture, 0.71–0.81 for distal 1/3rd fracture and 0.77–0.93 for middle 1/3rd fracture. Ideal range for proximal 1/3rd fracture cannot be commented upon pertaining to the lesser number of cases with proximal 1/3rd fractures. This means if we keep our Cast index within this range, it is less likely to redisplace after initial reduction.[20,21]
With the advancement of surgical instruments, techniques, operation theater sterilization equipment, anesthesia, antibiotics, etc., focus of the surgeons is gradually shifting towards operating even those cases that can be conservatively treated. Because of this, even the young budding surgeons pay less heed to the reduction techniques, technique of cast molding, proper application of cast and proper use of casting materials. So, gradually the quality of cast has been coming down with the fading technique of proper casting and lack of interest in budding surgeons. However, surgeries are always bound to have complications, even though they provide early mobilization. Casting in children comes with lesser complications and results are on par with surgeries thus making them a better alternative compared to surgeries. That is why, learning to apply better quality of cast is very necessary for budding surgeons. Cast index can act as a guiding stick for such surgeons and hence its use must be encouraged on a regular basis.
Limitations of the study
The present study had limitations of sample size (only 40 patients) because of successive year lockdown due to COVID leading to lesser outpatient and emergency visits of patients, lesser number of proximal 1/3rd fractures, no functional outcomes were studied, no comparison between Plaster of Paris and synthetic casting materials was done, fracture site obliquity as a cause of re-displacement was not studied and single hospital selection of cases.
Scope of our article
The use of Cast index is not routinely done even by budding surgeons even though a number of studies have proven its simplicity and efficacy. Our study might contribute to the existing literature.
Conclusion
Cast index is an excellent tool to monitor the quality of cast and risk of re-displacement. Cast index gives us an analogy about the quality of cast in pediatric forearm fractures, so that a poorly applied cast can be monitored for re-displacement over the course of fracture healing. With proper use, it can also be used as a guiding stick for young surgeons for a better learning curve of cast application in pediatric forearm fractures. Thus, regular use of Cast index should be encouraged in all orthopedic centers, especially for pediatric forearm fractures.
Acknowledgement
None.
Ethical Approval
The authors declare that they have taken the Institutional Ethics Committee approval and the approval number is 77/IEC-GRMC/2019.
Declaration of patients consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Pediatric upper extremity injuries. Pediatr Clin North Am. 2006;53:41-67.
- [CrossRef] [PubMed] [Google Scholar]
- Limb fracture pattern in different pediatric age groups: A study of 3,350 children. J Orthop Trauma. 1993;7:15-22.
- [CrossRef] [PubMed] [Google Scholar]
- Displaced fracture of the distal radius in children: Factors responsible for redisplacement after closed reduction. J Bone Joint Surg Br. 2005;87:841-3.
- [CrossRef] [PubMed] [Google Scholar]
- Displaced paediatric fractures of the distal radius. Arch Orthop Trauma Surg. 2008;128:55-60.
- [CrossRef] [PubMed] [Google Scholar]
- Redisplacement after manipulation of distal radial fractures in children. J Bone Joint Surg Br. 1993;75:453-4.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors in redisplacement of distal radial fractures in children. J Bone Joint Surg Am. 2008;90:1224-30.
- [CrossRef] [PubMed] [Google Scholar]
- Short arm plaster cast for distal pediatric forearm fractures. J Pediatr Orthop. 1994;14:211-3.
- [CrossRef] [PubMed] [Google Scholar]
- Redefining the cast index: the optimum technique to reduce redisplacement in pediatric distalforearm fractures. J Pediatr Orthop. 2012;32:787-91.
- [CrossRef] [PubMed] [Google Scholar]
- Gap index: a good predictor of failure of plaster cast in distal third radius fractures. J Pediatr Orthop. 2007;16:48-52.
- [CrossRef] [PubMed] [Google Scholar]
- Forearm and distal radius fractures in children. J Am Acad Orthop Surg. 1998;6:146-56.
- [CrossRef] [PubMed] [Google Scholar]
- Compositional study of Indian five rupee coin by EDXRF technique. Int Rev Appl Eng Res. 2014;4:83-8.
- [Google Scholar]
- Forearm fractures in children: avoiding redisplacement. Injury. 1995;26:691-2.
- [CrossRef] [PubMed] [Google Scholar]
- Factors responsible for redisplacement of pediatric forearm fractures treated by closed reduction and cast. Indian J Orthop. 2018;52:536-47.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Redisplacement of diaphyseal fractures of the forearm after closed reduction in children: a retrospective analysis of risk factors. J Orthop Trauma. 2012;26:110-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cast and padding indices used for clinical decision making in forearm fractures in children. Acta Orthop. 2008;79:386-9.
- [CrossRef] [PubMed] [Google Scholar]
- Paediatric forearm and distal radius fractures: risk factors and re-displacement—role of casting indices. Int Orthop. 2010;34:407-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Factors affecting re-displacement in pediatric forearm fractures and the role of cast indices. Jt Dis Relat Surg. 2020;31:95.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Evaluation of cast index in predicting the outcome of pediatric forearm fractures. Orthopaedic Journal of MP Chapter. 2020;26:30-3.
- [Google Scholar]
- Cast index in predicting outcome of proximal pediatric forearm fractures. Indian J Orthop. 2015;49:398-402.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Analysis of the factors causing tight cast syndrome after closed reduction and casting of pediatric distal radius fractures. Acta Orthop Traumatol Turc. 2018;52:329-33.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Study of cast index in middle third fractures of both bones of forearm in children. Int Orthop. 2017;3:673-6.
- [Google Scholar]








