Translate this page into:
Clinical and Radiological Results of Minimally Invasive Two-Hole Dynamic Hip Screw Fixation of Stable Intertrochanteric Fractures: A Prospective Study of 50 Patients
*Corresponding author: Nadeem Ali, MS Orthopedics, Mughal Mohalla, Lalbazar, Srinagar, Jammu and Kashmir, 190023, India drnadeeem@gmail.com
How to cite this article: Dar FA, Iqbal Z, Lone AH, Ali N. Clinical and Radiological Results of Minimally Invasive Two-Hole Dynamic Hip Screw Fixation of Stable Intertrochanteric Fractures: A Prospective Study of 50 Patients. Int J Recent Surg Med Sci. 2024;10:S67-74. doi: 10.1055/s-0043-1761618
Abstract
Objectives
Intertrochanteric fractures are fractures of elderly population and are known for morbidity and mortality. Early stabilization with minimal surgical trauma is important for early mobilization to prevent recumbence-related complications.
Material and Methods
This prospective study was conducted on 50 stable intertrochanteric fractures that were managed by fixation with a small two-hole dynamic hip screw –(DHS) side plate using a minimally invasive technique. The surgical time, intraoperative blood loss, length of the skin incision, duration of hospital stay, time to full weight bearing and fracture union, and complications were recorded.
Results
The mean age of the patients was 60.2 years with 64% belonging to male sex. The mean operative time, average blood loss, and mean incision length were 35.6 minutes, 68.4 mL, and 3.7 cm, respectively. Time to bone healing ranged from 10 to 16 weeks (mean 13 weeks). Two patients had hip screw backout but that did not interfere with failure of fixation.
Conclusion
Stabilization of stable intertrochanteric fractures with two-hole DHS using minimally invasive approach is a viable option with negligible complication rate related to failure of small DHS side plate.
Keywords
DHS
DHS side plate
Hip screw
Intertrochanteric
INTRODUCTION
Intertrochanteric fractures are the most common fractures around the hip in the geriatric osteoporotic population accounting for significant morbidity as well as mortality. The incidence of these fractures is on a rise with increase in the life expectancy and the consequent osteoporotic elderly population.[1] The management of these fractures has been revolutionized with the introduction of dynamic hip screw (DHS) by Clawson in 1964.[2] Since then different types of implants including cephalomedullary nails have been introduced. Despite these developments DHS is still being considered a gold standard implant in intertrochanteric fractures.[3,4]
The main goal of an operating surgeon in intertrochanteric fractures is to achieve a stable fixation of the fracture as early as possible that will allow early mobilization and thus prevent complications of recumbence.[5] However, this cannot be done at the stake of limited body reserves that these elderly patients have. Nearly 90% of the patients with hip fractures are above 65 years of age and also have more than one associated medical comorbidity making them poor candidates for surgical intervention.[6] To minimize the quantum of trauma to the soft tissues, some surgeons started using a two-hole DHS side plate at the beginning of this century. Despite promising results, use of two-hole DHS did not gain much popularity. And the scientific research with use of two-hole DHS side plate is scanty in the literature.[7] Though there is a theoretical concern of loss of fixation of DHS side plate from the lateral femoral cortex when only two cortical screws are used which many surgeons may be afraid of, biomechanical studies conducted by McLoughlin et al. suggest two-hole side plate is as stable as a four-hole plate.[8] Moreover, a small two-hole side plate can be inserted percutaneously through a 3 to 4 cm skin incision making technique minimally invasive.
Since the use of two-hole plate in unstable intertrochanteric fractures is controversial, we planned this study of using a two-hole DHS in stable intertrochanteric fractures through a minimally invasive technique.
MATERIAL AND METHODS
This prospective study was conducted on 50 patients in the Department of Orthopaedics of our institute over a period of 3 years from November 2018 to October 2021. The intertrochanteric fractures were classified as per AO classification and those with stable fracture configuration (AO type 31 A1.1, 31 A1.2, 31A1.3 and 31 A2.1) were included in this study. Unstable fractures, compound fractures, pathological fractures, skeletal immaturity, poor skin condition, patients with multiple comorbidities, poly trauma patients, and patients with other associated fractures of the lower extremities were excluded from this study.
After admission, all the patients were evaluated clinically as well as radiologically and all the routine baseline investigations were ordered. Skin traction on the fracture side was applied and routine thromboprophylaxis as per the hospital protocol was started. On the day of surgery, intravenous prophylactic antibiotic (cefuroxime 1.5 g) was administered in the operating room half an hour before start of surgical procedure.
Surgical Procedure
After spinal anesthesia, the patient was kept in supine position on the traction table. Both feet were secured separately in traction boots or traction foot plates. Gentle traction was applied to fractured lower extremity with limb in external rotation, with reduction completed by internal rotation. As most of these fractures were minimally displaced and stable, reduction could be achieved by this simple maneuver. In case there was a sagittal plane deformity or a posterior sag of the distal fragment, correction was done by applying anterior force to the distal fragment before internal rotating the lower extremity. Reduction quality was assessed with fluoroscopy using Baumgaertner and Solberg criteria.[9] A good reduction displays normal or slight valgus neck shaft angle on anteroposterior view, less than 20 degrees neck shaft angulation on lateral view, and less than 4 mm displacement on either view.
After prepping and draping, a guide wire was inserted percutaneously approximately 1.5 cm below vastus ridge, and passed in the center of the neck and head under fluoroscopic control in both the views [Figure 1a and b]. The wire was advanced till it was 5 mm short of the joint line. Following this a longitudinal skin incision, usually 3 to 5 cm long, was made around the guide wire and progressed distally. After opening skin and subcutaneous tissue, fascia lata and vastus lateralis were split along their fibers up to bone along the direction of the skin incision. The length of the guide wire inside the bone was measured with the help of a measuring device and a hip lag screw of length 5 mm less than this measurement was selected for fixation. The angle between guide wire and lateral femoral cortex was measured on fluoroscopic image to select a proper angle of DHS side plate. A cannulated triple reamer adjusted to the chosen length of the lag screw was used to ream the bone over the guide wire, taking care to protect the surrounding soft tissue with the help of a tissue protector [Figure 1c]. The femoral head and neck were tapped and the selected hip screw was inserted across the fracture into neck and head of the femur over the guide wire [Figure 1d]. The soft tissue was retracted and a proper angled DHS plate was inserted in the wound in a reverse fashion with the barrel of the side plate away from the lateral cortex toward the surgeon [Figure 1e]. As soon as the plate was introduced, it was turned 180 degrees to engage the plate barrel over the screw. Once plate was seated well, two cortical screws were used to stabilize the side plate followed by placement of the compression screw in the hip screw [Figure 1f and 1g]. Wound was closed layer wise and antiseptic dressing was applied [Figure 1h]. Besides this operating time measured from skin incision to closure was recorded and intraoperative blood loss was measured with weight of blood-soaked gauze.
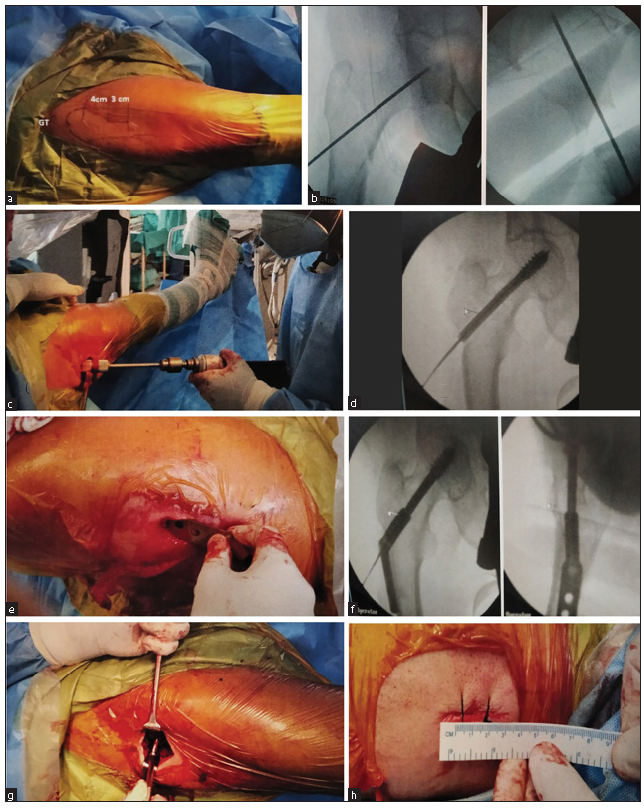
- Intraoperative images. (a) Prepping and draping. (b) Percutaneous placement of guide pin under fluoroscopic guidance. (c) Triple reaming over guide wire. (d) Hip screw inserted over guide pin. (e) Insertion of side plate with barrel facing surgeon. (f) Fluoroscopic image of seating of the dynamic hip screw plate. (g) Fixing side plate with cortical screws. (h) Final picture after closure of wound (3.5 cm in length).
Postoperative protocol
Anteroposterior and lateral radiographs were obtained the next day and the patient was mobilized and allowed to bear weight on the extremity as tolerated with the help of an ambulatory support. Range of motion exercises of hip, knee, and ankle were encouraged. Thromboprophylaxis was restarted 24 hours after the surgery and was continued for 2 weeks. Postoperatively patients were given one dose intravenous antibiotic followed by oral antibiotics for 3 days. All the patients were discharged by second day.
The patients were followed at 2 weeks for removal of stitches and then every monthly till union occurred. Final follow-up was done at 1 year. At each follow-up, the patient was evaluated for function, residual shortening, deformity, wound complication, and other complications like deep vein thrombosis. Radiological evaluation was done to check for union, collapse, screw backout, screw cutout, side plate backout, and other complications. The fracture was said to be united when full weight bearing was painless and there was no local fracture site tenderness and radiologically there was bridging of at least three out of four cortices on two orthogonal images [Figures 2 and 3]. The final functional assessment was done at 1 year using Harris Hip Score (HHS) and the results were graded on the basis of HHS as poor (score < 70), fair (score 70–79), good (score 80–89), and excellent (score 90–100).[10]

- Anteroposterior and lateral images of case No 10. (a) Preoperative radiographs. (b) Postoperative radiographs. (c) Radiographs at 1 year showing union and maintained neck shaft angles.

- Anteroposterior and lateral images of case No 30. (a) Preoperative radiographs. (b) Postoperative radiographs. (c) Radiographs at 1 year showing union and maintained neck shaft angles.
Statistical Methods
The recorded data was compiled and entered in a spreadsheet (Microsoft Excel) and the exported to data editor of SPSS Version 20.0 (SPSS Inc., Chicago, Illinois, United States). Continuous variables were expressed as mean ± standard deviation and categorical variables were summarized as percentages.
RESULTS
The age of the patients ranged from 35 to 85 years with a mean of 60.2 ± 14.5 years. Sixty four percent of the patients were males. Low-energy trauma like a slip or missing a step was the predominant mode of injury seen in 56% followed by fall from height in 32% cases. Hypertension was the most common associated comorbidity seen in 30%, cardiopulmonary ailments in 20%, and diabetes mellitus in 8% of the cases. AO type 31 A1.2 was the most common fracture configuration in our group seen in 44% of the patients that was followed by type 31 A1.1 in 40%, type 31 A2.1 in 12%, and type 31 A1.3 in 4% patients.
All the patients were operated within 3 days of admission with a mean time interval of 2.1 ± 0.47 days between admission and surgery. The operative time ranged from 25 to 60 minutes with a mean of 35.6 ± 7.34 minutes. The length of skin incision ranged from 3 to 5 cm with a mean of 3.7 ± 0.56 cm. The blood loss during the procedure ranged from 50 to 100 mL with a mean of 68.4 ± 12.39 mL. Majority of the patients (84%) were discharged on the first postoperative day and the remaining 16% patients on second day. By 14 weeks, all the patients had full weight bearing. Fifty six percent patients bore full weight within 8 weeks after intervention. The mean time to union was 13 ± 1.83 weeks and ranged from 10 to 16 weeks. Overall, the complication rate was 16%. Deep vein thrombosis was the most common complication seen in 8% (n = 4) patients. Infection in the postoperative period was seen in two patients. One patient had a superficial infection, while the other one had a deep infection that required re-exploration and debridement. Two patients (4%) had lag screw backout that lead to hardware symptoms and required removal of the hardware [Figure 4]. There was no case of screw cutout from the head or failure of side plate.

- Complication. (a) Postoperative anteroposterior and lateral radiograph. (b) Radiographs at final follow-up of 1 year showing union, well-maintained alignment with backout of hip screw.
At the final follow-up of 1 year, the HHS ranged from 71 to 100 with a mean of 91.7 ± 7.12. The results were excellent in 60%, good in 36%, and fair in 4% patients.
DISCUSSION
Fixation of intertrochanteric fractures using a DHS is a standard practice. The outcome of these fractures depends on multiple factors like age of the patient, degree of osteoporosis, associated comorbidities, fracture pattern (stable or unstable), time interval from injury to surgical intervention, postoperative rehabilitation, and stability of fixation.[11,12] The intertrochanteric fractures are unique in that they always unite because of broad cancellous and vascular opposing surfaces at the fracture site.[13] So, a stable fixation without disturbing the surrounding soft tissue using a minimally invasive approach is need of the hour in these fractures, especially in the elderly population who cannot withstand prolonged and complicated interventions. This is only possible if a DHS with a small two-hole plate can be used for fixing these fractures. But most of the orthopaedic surgeons will raise a question whether a two-hole side plate is sufficient for stabilization of fracture till union is achieved.
The initial biomechanical research regarding optimal length of DHS side plate in unstable intertrochanteric fractures was done by Yian et al. in 1997. They concluded three screws allowed favorable distribution of tensile force and adequate side plate fixation. However, they did not use a telescoping lag screw in their biomechanical study and concluded that using a telescoping or a sliding screw mechanism will further reduce the stress on the side plate screws and probably two screws are enough to bear the stress in these fractures.[14] Later in 2000, Mcloughlin et al. in their biomechanical study on cadaveric femurs found that strength and stiffness of a two-hole and four-hole side plate were comparable when used to fix unstable intertrochanteric fractures.[8] Rog et al. recently in 2017 demonstrated on a recreated AO type 31 A1 fracture in osteoporotic saw bone models that fixation with DHS using a two- or a four-hole side plate was comparable with respect to axial and torsional stiffness and load to failure.[15] Soni et al. in their systematic review on plate length in stable intertrochanteric fractures concluded that good quality randomized controlled studies are required in stable intertrochanteric fractures fixed with two- and four-hole DHS.[16] However, when the studies on two-hole DHS fixation though limited are dissected, the results favor the use of two-hole side plates. Our study was based on the results of these biomechanical as well as other clinical studies.
A relook in the literature could only trace five case series where a two-hole DHS plate fixation has been used [Table 1]. The initial work of using a two-hole side plate in intertrochanteric fractures is credited to Bolhofner et al. They showed promising results with an implant failure rate of 4.3%. Two of their patients had screw cutout from the head and one had dissociation of hip screw from the plate barrel that could not be related to short side plate. These complications may result from osteoporosis, improper placement of hip screw in head and neck, or due to unstable fracture pattern. Increasing the length of the side plate would not have prevented these failures. Inclusion of unstable fracture pattern in their study may be one of the factors responsible for these complications.[17] Verhosfstad and van der Werken published a retrospective study on 148 patients with stable intertrochanteric fractures, which is the largest series on the use of two-hole DHS till date. They had a hardware failure rate of 2.02% (n = 3). The failure was in the form of screw cutout in two patients secondary to poor position of hip screw in the head and plate breakage in one patient due to retrauma. There was no failure of the side plate or cortical screws holding the side plate.[18] DiPaola et al. in a small series of 13 patients had no issues of any hardware failure.[6] Laohapoonrungsee et al. in their series of 83 patients that included both stable and unstable fractures had hip screw cutout in two patients and side plate failure in two patients. Two patients where the side plate failed had unstable fracture configuration (AO type A2.2) as well as osteoporosis with Singh index of 2 and 3 respectively.[12] We in our study had excluded type A2.2 fractures because they are unstable and have chances of collapse and hardware failure. Riha et al. in their series of 32 patients, majority of whom had stable fracture configuration, had pull out of the plate from the femoral shaft in one patient secondary to fall from bed.[19] We in our series of 50 cases had no implant failure that may attributed to inclusion of only stable fracture patterns in our study and also taking care to place a proper sized hip screw in the center of the neck and head of proximal femur. However, we had two cases where there was backing out of hip screw, which gave hardware symptoms to the patient, but it did not interfere with healing of the fracture in a proper position. It may be due to simple backing out of the screw rather than backing out secondary to fracture site collapse.
Study |
No of patients |
# type S/US |
Incision length |
Operating duration |
Blood loss |
Union time |
Implant failure |
Other complications |
|---|---|---|---|---|---|---|---|---|
Bolhofner et al.[17] 1999 |
70 |
S = 58 US = 12 |
31 min |
77 mL |
15 wk |
3 (4.3%) |
– |
|
DiPaola et al.[6] 2004 |
13 |
S = 13 |
5 cm |
61 min |
41.9 mL |
13 wk |
None |
None |
Verhofstad et al.[18] 2004 |
148 |
S = 148 |
– |
– |
– |
– |
3 (2.02%) |
Wound hematomas (1.35%), infection (2.7%) |
Laohapoonrungsee et al.[12] 2005 |
83 |
S = 53 US = 30 |
– |
– |
– |
14.5 wk |
4 (4.82%) |
None |
Riha et al.[19] 2010 |
32 |
S = 30 US = 2 |
5.5 cm |
28 min |
– |
10 wk |
1 (3.1%) |
None |
Present |
50 |
S = 50 |
3.7 cm |
36.6 min |
68.4 mL |
13 wk |
None |
DVT (8%), infection (4%), hip screw backout (4%) |
Abbreviations: #, fracture; DVT, deep vein thrombosis; S, stable; US, unstable.
Use of a two-hole DHS significantly reduces the operating time to mean of 30.44 minutes from a mean of 51.45 minutes required for a four-hole side plate fixation.[16] Bolhofner et al. and Riha et al. had a mean operating time of 31 and 28 minutes in their series that is comparable to our 36.6 minutes.[17,19] The mean incision length in our patients had been 3.7 cm that is much smaller than that seen in other studies. Riha et al. had an average incision length of 5.5 cm in their study. This may be due to our minimally invasive approach in fixing these fractures.[19] Study by DiPaola et al. is the only work where minimally invasive technique had been used and the average incision length in their study was 5 cm.[6] The average blood loss of 68.4 mL in our patients is comparable to 77 mL of Bolhofner et al.[17] The time to radiological union in intertrochanteric fractures stabilized by a two-hole DHS is variable ranging from 6 to 16 weeks.[16] In our patients, it ranged from 10 to 16 weeks. From other studies, the mean healing time ranges from 10 to 15 weeks with 13 weeks for our study [Table 1].
The main problem with the use of short length plate that bothers orthopaedic surgeons is the risk of failure of the side plate that is held by two cortical screws that too in the osteoporotic bone. However, as we have gone through the scant literature that is available as well as from the experience from our series, using a two-hole side plate in stable intertrochanteric fractures is possible without any risk of failure of side plate from the distal fragment. Good results have even been seen with some unstable (AO type 31 A2.2) fractures. Besides this the minimally invasive technique has significantly reduced the operating time, intraoperative blood loss, amount of soft tissue dissection as well as the size of the surgical incision. All this aids in less postoperative need for blood transfusions and analgesic requirement that aids in early rehabilitation and early discharge from the hospital.[16]
The main drawback of this study is a small patient base. Randomized controlled trials comparing the results of two-hole plates with longer plates are need of the hour to come to conclusion and formulate guidelines for the optimal length of DHS side plate for intertrochanteric fracture fixation.
CONCLUSION
Two-hole DHS side plate is a safe and stable fixation device, without any risk of loss of its fixation from the femoral shaft when utilized for fixation of stable (AO type A1.1, A1.2, A1.3 and A2.1) intertrochanteric fractures. Using it in a minimally invasive manner further reduces the incision length, intraoperative blood loss, extent of soft tissue dissection as well as the surgical time interval that helps in early rehabilitation and early discharge form the hospital.
Acknowledgments
None.
Conflicts of Interest
None declared.
References
- Femoral Intertrochanteric Fractures of the Patients in the Emergency Department Due to Minor Falls: Special Consideration in the Middle-Old to Oldest-Old Patients. Ann Geriatr Med Res. 2019;23:125-32.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Trochanteric Fractures Treated by the Sliding Screw Plate Fixation Method. J Trauma. 1964;4:737-52.
- [CrossRef] [PubMed] [Google Scholar]
- Nail or Plate Fixation of Intertrochanteric Hip Fractures: Changing Pattern of Practice. A Review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am. 2008;90:700-7.
- [CrossRef] [PubMed] [Google Scholar]
- Type II Intertrochanteric Fractures: Proximal Femoral Nailing (PFN) Versus Dynamic Hip Screw (DHS) Arch Bone Jt Surg. 2016;4:23-8.
- [PubMed] [PubMed Central] [Google Scholar]
- Implant Options for the Treatment of Intertrochanteric Fractures of the Hip: Rationale, Evidence, and Recommendations. Bone Joint J. 2017;99-B:128-33.
- [CrossRef] [PubMed] [Google Scholar]
- Minimal Incision Technique Using a Two-Hole Plate for Fixation of Stable Intertrochanteric Hip Fractures. Orthopedics. 2004;27:270-4.
- [CrossRef] [PubMed] [Google Scholar]
- Fixation of AO-OTA 31-A1 and A2 Trochanteric Femur Fractures Using a Sliding Hip Screw System: Can We Trust a Two-Hole Side Plate Construct? A Review of the Literature. EFORT Open Rev. 2020;5:118-25.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Biomechanical Evaluation of the Dynamic Hip Screw with Two- and Four-Hole Side Plates. J Orthop Trauma. 2000;14:318-23.
- [CrossRef] [PubMed] [Google Scholar]
- Awareness of Tip-Apex Distance Reduces Failure of Fixation of Trochanteric Fractures of the Hip. J Bone Joint Surg Br. 1997;79:969-71.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic Arthritis of the Hip After Dislocation and Acetabular Fractures: Treatment by Mold Arthroplasty. An End-Result Study Using a New Method of Result Evaluation. J Bone Joint Surg Am. 1969;51:737-55.
- [PubMed] [Google Scholar]
- Risk Factors for Functional Outcomes of the Elderly with Intertrochanteric Fracture: A Retrospective Cohort Study. Orthop Surg. 2019;11:643-52.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Two-Hole Side-Plate DHS in the Treatment of Intertrochanteric Fracture: Results and Complications. Injury. 2005;36:1355-60.
- [CrossRef] [PubMed] [Google Scholar]
- A Prospective Study of the Functional Outcome of Intertrochanteric Femoral Fracture Managed with Short Proximal Femoral Nail. Int J Contemp Med Res. 2020;7:B9-B16.
- [Google Scholar]
- Optimal Side Plate Fixation for Unstable Intertrochanteric Hip Fractures. J Orthop Trauma. 1997;11:254-9.
- [CrossRef] [PubMed] [Google Scholar]
- A Biomechanical Comparison of the Two- and Four-Hole Side-Plate Dynamic Hip Screw in an Osteoporotic Composite Femur Model. J Orthop Surg (Hong Kong). 2017;25:2309499017717199.
- [CrossRef] [PubMed] [Google Scholar]
- Dynamic Hip Screw Plate Length in Stable Intertrochanteric Fracture Neck of Femur: A Systematic Review. Cureus. 2022;14:e23138.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Results of Intertrochanteric Femur Fractures Treated with a 135-Degree Sliding Screw with a Two-Hole Side Plate. J Orthop Trauma. 1999;13:5-8.
- [CrossRef] [PubMed] [Google Scholar]
- DHS Osteosynthesis for Stable Pertrochanteric Femur Fractures with a Two-Hole Side Plate. Injury. 2004;35:999-1002.
- [CrossRef] [PubMed] [Google Scholar]
- Internal Fixation of Pertrochanteric Fractures Using DHS with a Two-Hole Side-Plate. Int Orthop. 2010;34:877-82.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







