Translate this page into:
Clinical Markers of Reperfusion in Patients with Acute Myocardial Infarction and Its Prognostic Significance
Corresponding Author: Anuj R Varma, Assistant Professor, Department of Medicine, Datta Meghe Institute of Medical Sciences, Wardha, Maharashtra, India, Phone: +919860500065 e-mail: anujvarma1985@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
How to cite this article: Varma AR, Chillawar S, Kamble TK, Acharya S. Clinical Markers of Reperfusion in Patients with Acute Myocardial Infarction and Its Prognostic Significance. Int J Recent Surg Med Sci 2016;2(2):90-95.
Abstract
Introduction:
Coronary artery disease (CAD) is a major cause of mortality worldwide. Thrombolysis in the treatment of acute myocardial infarction (AMI) is a landmark event in the management as it has changed the outcomes. Clinical signs after thrombolysis in AMI may have a better correlation with functional reperfusion than the isolated image of angiographic patency.
Aims and objectives:
To study successful clinical reperfusion (SCR) noninvasively using clinical markers of reperfusion. To evaluate the prognostic value of clinical markers of reperfusion in predicting early (30 days) prognosis after thrombolysis in AMI. To observe the effect of age, location of MI, presence of previous infarction, Killip's class at admission, and presence of clinical reperfusion assessed noninvasively on early (30 days) prognosis after AMI.
Materials and methods:
All the patients were thrombolyzed (using streptokinase). Successful clinical reperfusion was defined by the presence of at least two of the following criteria at 2 hours of starting treatment: (1) Significant relief of pain (50% or more), (2) 50% or more reduction in sum of ST segment elevation, (3) abrupt initial rise of creatine kinase MB (CK-MB) level, more than two-fold over upper normal or baseline values.
Results:
Duration of symptoms (min) mean ± SD was nearly the same in two groups (94.80 ± 13.68 vs 96.19 ± 17) but early thrombolysis resulted in better outcome (0.01 S, p < 0.05). killips class at admission (KAD) > OR = 2, n (%) led to worsened fate of thrombolysis. Death n (%) occurred in 7 (8.75%) patients with 1 (1.25%) from SCR (+) group and 6 (7.5%) from SCR (–) group (0.01 S, p < 0.05).
Conclusion:
It is concluded that Killip's class at admission of more than or equal to two and absence of SCR are the predictors of mortality after thrombolysis. Absence of SCR defines a group of patients with poorer prognosis after thrombolysis and in such patients alternative strategies of reperfusion should be considered.
Keywords
Coronary artery disease
Reperfusion
Streptokinase
Thrombolysis
INTRODUCTION
Coronary artery disease (CAD) is a major cause of mortality worldwide. It is predicted that CAD resulted in 1.46 million deaths, which is 14% out of a total of 10.3 million deaths in year 2004.1 Coronary heart disease is forecast to be the most common cause of death globally, including India, by 2020.2 Introduction of thrombolysis in the treatment of acute myocardial infarction (AMI) was a landmark event in the management of AMI as it has changed the outcomes after AMI.3,4 It has been convincingly demonstrated that early opening of infarct-related artery is associated with the limitation of the infarct size, preservation of left ventricular function, and better clinical outcome.5 Reduction in chest pain after thrombolysis has been shown to correlate with angiographically assessed patency and can be used as clinical marker of reperfusion.6 ST resolution after AMI is influenced by coronary artery status and achievement of early ST resolution is marker of reperfusion.7,8 Washout of creatine kinase MB (CK-MB), i.e., released from injured myocytes occurs after restoration of coronary artery patency. Hence rapid peaking of CK-MB after thrombolysis can be considered as marker of successful reperfusion.9 Because angiography is not available in every hospital, there is an increasing interest in simple noninvasive tests of patency assessment.10 Furthermore, clinical signs after thrombolysis in AMI may have a better correlation with functional reperfusion than the isolated image of angiographic patency.11
This opportunity was therefore undertaken to study the success of reperfusion using noninvasive clinical criteria of reperfusion and evaluate prognostic value of clinical markers of reperfusion in predicting short-term (30 days) outcome after AMI in rural setup. Our aim is to study successful reperfusion noninvasively using clinical markers and its prognostic value in predicting early (30 days) outcome after thrombolysis in AMI. We have also observed the effect of age, location of myocardial infarction (MI), presence of previous infarction, Killip's class at admission, and presence of clinical reperfusion assessed noninvasively on early (30 days) prognosis after AMI.
MATERIALS AND METHODS
Study Design
This prospective observational study was carried out in patients of AMI presenting within 6 hours of onset of chest pain, admitted in 20-bed ICU and ICCU of Acharya Vinoba Bhave Rural Hospital of Jawaharlal Nehru Medical College, Wardha in Central India from August 2010 to 2012. All the consecutive patient of AMI admitted in ICU were enrolled in this study, which has been approved by Ethical Committee of the Institute.
Patient Selection
Inclusion Criteria
Patients with H/O of acute onset of chest pain S/O of AMI (of duration less than 6 hours, lasting more than 20 minutes and not relieved by nitrates irrespective of their Killip's class12).
Twelve lead ECG within 6 hours of onset of chest pain S/O AMI in the form of ST elevation of at least 2 mm in contiguous precordial leads and 1 mm in two adjacent limb leads persisted more than 10 minutes after administration of nitrates.
Exclusion Criteria
Chest pain for more than 6 hours.
Left bundle branch block in the electrocardiogram before thrombolysis.
Those with the contraindication to thrombolysis (as per guidelines given by American College of Cardiology).
Age of patient more than 75 years.
Methods
All the patients were thrombolysed (using 1.5 million International Units (IU) of streptokinase in 100 mL normal saline over 60 minutes). After thrombolysis patients were divided into two groups based on success of thrombolysis ascertained using noninvasive criteria. Those with successful reperfusion were grouped into SCR (+) group and those without it were grouped into SCR (–) group. Both the groups were then followed for next 30 days and are compared. Successful clinical reperfusion was defined by presence of at least two of the following criteria at 2 hours of starting treatment.
Significant relief of pain (50% or more)
A total of 50% or more reduction in sum of ST segment elevation.
Abrupt initial rise of CK-MB level, more than two-fold over upper normal or baseline values.
Follow-up
Patients from both groups were followed up at 24 hours after thrombolysis and then on 7th day, 30th day, and thereafter if possible.
Statistical Analysis
By univariate analysis (chi-square test), the association of mortality rate with various clinical variable was analyzed. The comparison of baseline variables was made by Student's unpaired t-test, chi-square test for continuous and categorical variables respectively. A “p” value of less than 0.05 was considered statistically significant.
RESULTS
Among 80 cases studied, 60 (75%) were males and 20 (25%) cases were female. The male to female ratio was 3:1. The mean age of patients in the SCR (+) group was 55.7 ± 8.63 years, while mean age of patients from SCR (–) group was 54.71 ± 8.84 years (p = 0.95, NS). Baseline characteristics of our patients are shown in Table 1. There was no correlation between age and success of reperfusion. An analysis of risk factors for the CAD in the present work showed smoking as the commonest risk factor, being present in 56.25% of cases. Hypertension was the next common risk factor seen in 55% cases. Diabetes mellitus type 2 was present in 13.75% cases. Obesity was observed in 34 (42.5%) patients. Majority of patients have duration of chest pain between 61 and 180 minutes, i.e., in 31 (38.75%) patients, out of which 25 (31.25%) patients were in the SCR (+) group and 6 (7.5%) patients in the SCR (–) group. Moreover, 35 (43.75%) patients had chest pain ranging between 241 and 360 minutes in duration, out of which 15 (18.75%) patients were in the SCR (+) and 20 (25%) patients in the SCR (–) group. Mean chest pain duration in both the groups is nearly similar, however, early treatment resulted in better outcome in the form of reperfusion (t* 14.95, p = 0.01). It was observed that maximum, i.e., 62 (77.5%) patients were in Killip's class I at admission, out of which 42 (52.5%) patients were in the SCR (+) and 20 (25%) patients in the SCR (–) group. Eighteen (24%) patients (among Killip's II, III, and IV) out of 80 were in congestive cardiac failure at the time of admission, out of which 6 (7.5%) patients from SCR (+) and 12 (14%) patients from SCR (–) group. Majority of patients had anterior wall MI, i.e., 57 (71.25%) patients, out of which 32 (40%) patients from SCR (+) group and 25 (31.25%) patients from SCR (–) group. Location of MI did not affect fate of thrombolysis. Chi-square = 1.78, p-value = 0.40, NS, p > 0.05. Mean ejection fraction was 53.33 ± 10.15 in the SCR (+) group, while it was 41.59 ± 13.33 in the SCR (–) group (t = 4.605, p = 0.0001). The ejection fraction in the SCR (–) group was significantly less as compared to SCR (+) group.
| Variable | No. of cases | SCR (+) | SCR (–) | p-value |
|---|---|---|---|---|
| n | 80 | 48 | 32 | – |
| Age Mean ± SD | 66.54 | 55.70 | 54.71 | 0.62 NS, |
| ± 27.76 | ± 8.63 | ± 8.84 | p > 0.05 | |
| Sex (% Male) | 60 (75%) | 38 | 22 | 0.95 NS, p > 0.05 |
| (47.5%) | (27.5%) | |||
| Duration of symptoms (min) Mean ± SD | 99.80 | 94.80 | 96.19 | 0.01 S, p < 0.05 |
| ± 11.15 | ± 13.68 | ±17 | ||
| Previous infarct n (%) | 8 (100%) | 4 (50%) | 4 (50%) | 1.00 NS, p > 0.05 |
| Anterior MI n (%) | 67 (83.75%) | 32 (40%) | 25 (31.25%) | 0.40 NS, p > 0.05 |
| KAD > OR = 2 n (%) | 18 (22.5%) | 6 (7.5%) | 12 (15%) | 0.02 S, p < 0.05 |
| KAD = 4 n (%) | 2 (2.5%) | 1 (1.25%) | 1 (1.25%) | 1.00 NS, p > 0.05 |
NS: Nonsignificant
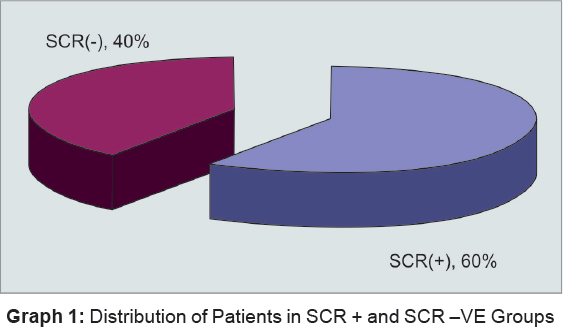
Successful clinical reperfusion defined by the presence of two or more of the three clinical criteria was present (SCR+) in 48 (60%) cases, while 32 (40%) cases did not have SCR (–) (Graph 1).
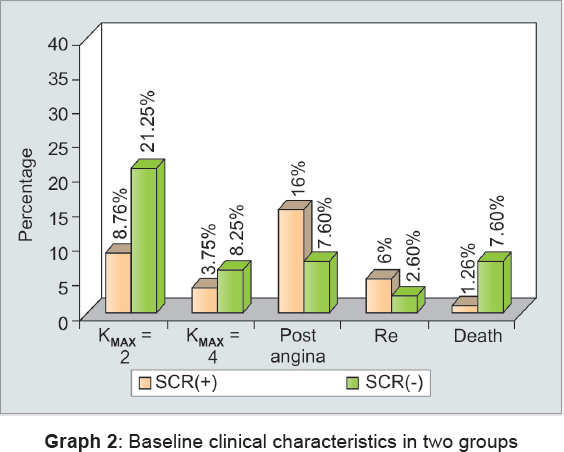
Out of 80 cases studied, 7 (8.75%) patients died within 30 days of thrombolysis. Significantly more deaths occurred in the SCR (–) group as compared to SCR (+) group (7.5 vs 1.25%, p < 0.05) (Table 2, Graph 2).
| Event | Overall | SCR (+) | SCR (–) | p-value |
|---|---|---|---|---|
| Killip's II or more n (%) | 24 (30%) | 7 (8.75%) | 17 (21.25%) | 0.01 S, p < 0.05 |
| Killip's MAX = IV n (%) | 8 (10%) | 3 (3.75%) | 5 (6.25%) | 0.51 NS, p > 0.05 |
| Post MI Angina n (%) | 18 (22.5%) | 12 (15%) | 6 (7.5%) | 0.07 NS, p > 0.05 |
| Re MI n (%) | 6 (7.5%) | 4 (5%) | 2 (2.5%) | 0.47 NS, p > 0.05 |
| Death n (%) | 7 (8.75%) | 1 (1.25%) | 6 (7.5%) | 0.01 S, p < 0.05 |
S: Significant; NS: Nonsignificant
ASSOCIATION OF CLINICAL VARIABLES AND MORTALITY RATE
By univariate analysis, Killip's class II or more at admission and absence of SCR (–) were significantly associated with death. Previous MI, anterior MI, age more than 65, however, were not significantly associated with death (Table 3).
| Variables | Chi-square | p-value | OR | 95% CI |
|---|---|---|---|---|
| KAD (≥2 vs 1) | 14.89 | 0.002 S, p < 0.05 | 1.68 | 0.96–2.95 |
| Absence of SCR | 6.68 | 0.010 S, p < 0.05 | 10.85 | 1.23–95.09 |
| Previous MI | 0.15 | 0.69 NS, p > 0.05 | 1.57 | 0.16–15.00 |
| Anterior MI | 0.92 | 0.69 NS, p > 0.05 | 0.37 | 0.04–3.3 |
| Age > 65 | 1.09 | 0.29 NS, p > 0.05 | 0.40 | 0.02–7.60 |
S: Significant; NS: Nonsignificant
Considering Killip's class at admission, mortality rate was lower in patients with class I than in those with Killip's class II or more at admission (p = 0.002). Absence of SCR was associated with higher mortality rate (odds ratio 10.85, 95% confidence interval 1.23–95.09, p = 0.010) (Table 3).
Coronary Angiography
Coronary angiography was possible in only 17 cases due to economic constraints. Twelve (70.59%) patients from SCR (+) group underwent coronary angiography, out of which 9 (52.94%) patients had TIMI grade III flow, while 3 (17.65%) patients had TIMI grade II flow in the infarct-related artery.
In the SCR (–) group, 5 (29.41%) patients underwent coronary angiography out of which 2 (11.76%) patients had TIMI grade II flow, 2 (11.76%) had grade I flow, and 1 (5.88%) had grade 0 flow in the infarct-related artery.
There was statistically significant difference in above two groups in terms of presence of TIMI grade II or III flow in relation to success of thrombolysis (chi-square value = 66.52, p-value < 0.0001).
DISCUSSION
Successful clinical reperfusion was observed in 48 (75%) cases and it was absent in 32 (25%) cases. Patients with successful reperfusion were grouped as SCR (+) group and those without it as SCR (–) group. French et al13 measured ST recovery, and CK-MB before and 60 minutes after commencing streptokinase in 107 patients. At 90 minutes, 56% of patients (95% CI 46–66) had TIMI-3 flow.
Barsottia14 proved prognostic value of noninvasive markers of coronary reperfusion compared to TIMI 3 flow in patients treated with primary angioplasty. Reperfusion was successful in 87.7% of the patients, and TIMI 3 flow was achieved in 87% patients.
Success of reperfusion reported in the present study using the clinical markers of reperfusion are in accord with those reported by previous studies that range from 50 to 88%.15
Our observation in regards to duration of chest pain are similar with findings of Fibrinolytic Therapy Trialist (FTT) Collaborative Group Study.16 Barsottia14 reported in their study no significant difference in duration of presentation, i.e., 4.8 ± 2.7 vs 4.07 ± 06 hours in the SCR (+) and SCR (–) group respectively.
Mean age of the population in this study was 57.40 ± 8.21 years. Youngest patient was 34 years old, while oldest patient had an age of 70 years. Gupta et al17 reported 138 patients with the age of patients ranging from 32 to 84 years with mean age of 62.8 years. The mean age of patients in the present study is comparable to that reported in the earlier studies.
In the present study, 60 (75%) males and 20 (25%) females were studied. The male to female ratio was 3:1. Moreover, Johanson et al18 worked on dynamic model forecasting myocardial infarct size before, during, and after reperfusion therapy by using some of the prognostic criteria's observed to have females is to male ratio 2.9:1. In the present study, the finding regarding male is to female ratio is similar to studies mentioned.
Killip's class II or more were present in 18 (22.5%) patients, out of these, 6 (7.5%) were from SCR (+) group and 12 (15%) patients were from SCR (–) group. There was significant difference in these two groups in terms of occurrence of Killip's class II or more (p = 0.02 S). Ipparaguirre et al6 reported 90.8% of their patients in Killip's class I at the time of admission. Cardiac failure at admission was present in 9.2% of patients with 5.2% of patients from SCR (+) group and 16.2% patients from SCR (–) group (p < 0.001). Thus cardiac failure at admission was more frequent in the SCR (–) group as compared to SCR (+) group.
Among the patients of anterior wall infarction, 32 (40%) patients were from SCR (+) group and 25 (31.25%) patients were from SCR (–) group (p = 0.99, NS). Thus the two groups did not differ in terms of occurrence of anterior infarction. Barsottia14 reported that anterior wall infarction was present in 47.2% of patients from SCR (+) group and 83.3% patients from SCR (–) group. Thus the two groups differ in terms of occurrence of anterior infarction (p < 0.05), however, this finding is dissimilar to the finding of present study.
In the present study, the SCR (+) group had mean left ventricular ejection fraction of 53.33 ± 10.15, which was significantly higher as compared to that in the SCR (–) group in which it was 41.59 ± 13.33. (p = 0.0001). The findings in the present study in terms of ejection fraction is similar to the studies reported by Ong et al,19 Silber et al,20 and Matetzky et al.21
Within 30 days of thrombolysis, 24 (30%) patients had heart failure, out of which 7 (8.75%) patients were in the SCR (+) group and 17 (21.25%) patients in the SCR (–) group. Thus, occurrence of heart failure was significantly more in the SCR (–) group as compared to SCR (+) group (p < 0.05).
| Event | Barsottia et al14 (%) | Ipparaguirre et al6 (%) | Matetzky et al21 (%) | Present study (%) | |
|---|---|---|---|---|---|
| Kmax>/=2 | Total | 16.6 | 15 | 4.32 | 30 |
| SCR (+) | NA | 10.5 | 3.7 | 8.75 | |
| SCR (–) | NA | 23.1 | 5.55 | 21.25 | |
| Kmax = 4 | Total | NA | 4.9 | NA | 10 |
| SCR (+) | NA | 0.5 | NA | 3.75 | |
| SCR (–) | NA | 12.8 | NA | 6.26 | |
| Post MI angina | Total | 16.02 | 16.8 | NA | 22.5 |
| SCR (+) | NA | 20.5 | NA | 15 | |
| SCR (–) | NA | 10.2 | NA | 7.5 | |
| Re MI | Total | 11.5 | 3 | 12.96 | 7.5 |
| SCR (+) | NA | 3.3 | 15.74 | 5 | |
| SCR (–) | NA | 2.5 | 3.7 | 2.5 | |
| Death | Total | 3.65% | 8.2 | 1.85 | 8.75 |
| SCR (+) | 0.79 | 3.8 | 0 | 1.25 | |
| SCR (–) | 22.2 | 16.2 | 2.77 | 7.5 |
Equal or higher occurrence of postinfarction angina and recurrence of MI in the group with SCR are comparable with the group without it in the present study as well as in the studies by Ipparaguirre et al,6 Matetzky et al,21 Simoons et al,22 The GUSTO investigators,23 and Barsottia.14
In the present study, the overall mortality was 7 (8.75%), out of which 1 (1.25%) patient in the SCR (+) group, while 6 (7.5%) patients in the SCR (–) group. Difference in the mortality in the two groups was statistically significant (p < 0.01). The finding of mortality rate in the present study, moreover, is comparable to that in the studies by Johanson et al,24 Matetzky et al,21 Corbalan et al,25 and Barsottia.14
Coronary angiography was possible in only 17 cases due to economic constraints. Twelve patients from SCR (+) group underwent coronary angiography. Out of these, 9 patients had TIMI grade III flow in the infarct-related arteries, while 3 patients had TIMI grade II flow in the infarct-related artery. In the SCR (–) group, 5 patients underwent coronary angiography with 2 patients having TIMI grade II flow, 2 having grade I flow, and 1 having grade 0 flow in the infarct-related artery. There was statistically significant difference in these two groups in terms of presence of TIMI grade II or III flow (p < 0.05).
These observations are similar to French et al13 and Barsottia14 suggesting higher TIMI flow in successfully reperfused patients, and thus explaining the importance of clinical markers of reperfusion.
CONCLUSION
The overall occurrence of SCR in the present study was 60%, while 40% patients did not have SCR. It is concluded that Killip's class at admission of more than or equal to two and absence of SCR were the predictors of mortality after thrombolysis. Mortality rate was very high in patients without SCR than in patients with SCR. It is further advocated that all patients of AMI who receive thrombolysis should be assessed at the end of 2 hours for these simple, noninvasive clinical markers of reperfusion. Absence of SCR defines a group of patients with poorer prognosis after thrombolysis and in such patients alternative strategies of reperfusion should be considered.
Source of support:
Nil
Conflict of interest:
None.
REFERENCES
- Prevalence of coronary artery disease in Asian Indians. Am J Cardiol. 1992;70(9):945-949.
- [CrossRef] [PubMed] [Google Scholar]
- Global burden of cardiovascular disease. Part II. Variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001;104(23):2855-2864.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary heart disease in South Asian communities. London: Health Education Authority; 1994.
- [Google Scholar]
- Factors that determine recovery of left ventricular function after thrombolysis in patients with acute myocardial infarction. Circulation. 1985;71(6):1121-1128.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic value of clinical markers of reperfusion in patients with acute myocardial infarction treated by thrombolytic therapy. Am Heart J. 1997;134(4):631-638.
- [CrossRef] [PubMed] [Google Scholar]
- Noninvasive detection of coronary artery patency using continuous ST-segment monitoring. Am J Cardiol. 1986;57(11):916-922.
- [CrossRef] [PubMed] [Google Scholar]
- Open infarct artery, late potentials, and other prognostic factors in patients after acute myocardial infarction in the thrombolytic era. A prospective trial. Circulation. 1994;90(4):1747-1756.
- [CrossRef] [PubMed] [Google Scholar]
- Usefulness of rapid initial increase in plasma creatine kinase activity as a marker of reperfusion during thrombolytic therapy for acute myocardial infarction. Am J Cardiol. 1988;62(1):20-24.
- [CrossRef] [PubMed] [Google Scholar]
- Long term prognostic importance of patency of infarct related coronary artery after thrombolytic therapy for acute myocardial infarction. Circulation. 1994;89(1):61-67.
- [CrossRef] [PubMed] [Google Scholar]
- Determination of infarct size in reperfusion therapy for acute myocardial infarction. Circulation. 1992;86(1):81-90.
- [CrossRef] [PubMed] [Google Scholar]
- Aggressive treatment of arrhythmias in acute myocardial infarction. Prog Cardiovasc Dis. 1968;10:483-498.
- [CrossRef] [PubMed] [Google Scholar]
- A score predicts failure of reperfusion after fibrinolytic therapy for acute myocardial infarction. Am Heart J. 2003;145(3):380-382.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic value of noninvasive markers of coronary reperfusion compared to TIMI 3 flow in patients treated with primary angioplasty. Rev Esp Cardiol. 2004;57(6):524-530.
- [CrossRef] [Google Scholar]
- Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomized trials of more than 1000 patients. Lancet. 1994;343(8893):311.
- [CrossRef] [Google Scholar]
- A study of biochemical markers of reperfusion early after thrombolysis for acute myocardial infarction. Indian J Clin Biochem. 2008;23(1):89-91.
- [CrossRef] [PubMed] [Google Scholar]
- Natural history of valvular aortic stenosis. Br Heart J. 1973;35(1):41-46.
- [CrossRef] [PubMed] [Google Scholar]
- Left ventricular function and rapid release of creatine kinase in acute myocardial infarction: evidence for spontaneous reperfusion. N Engl J Med. 1983;309:1-6.
- [CrossRef] [PubMed] [Google Scholar]
- The prognostic importance of two easily obtainable noninvasive markers after intravenous thrombolytic therapy in acute myocardial infarction. Isr J Med Sci. 1993;29(5):268-277.
- [Google Scholar]
- The distinction between coronary and myocardial reperfusion after thrombolytic therapy by clinical markers of reperfusion. J Am Coll Cardiol. 1998;32(5):1326-1330.
- [CrossRef] [PubMed] [Google Scholar]
- Improved survival after early thrombolysis in acute myocardial infarction. Lancet. 1985;2(8455):578-582.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of tissue plasminogen activator, streptokinase or both on coronary artery patency, ventricular function, and survival after acute myocardial infarction. N Engl J Med. ;1993N Engl J Med. ;329:1615-1622.
- [CrossRef] [PubMed] [Google Scholar]
- A dynamic model forecasting myocardial infarct size before, during, and after reperfusion therapy: an ASSENT-2. Eur Heart J. 2005;26:1726-1733.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic value of noninvasive markers of coronary reperfusion in patients with acute myocardial infarction treated with thrombolysis. Rev Med Chil. 1996;124(12):1423-1430.
- [Google Scholar]







