Translate this page into:
Evaluation of Effectiveness of Preemptive Intravenous Analgesics versus Postoperative TAP Block in Unilateral Inguinal Hernioplasty—A Prospective Randomized Double-Blind Clinical Trial
Address for correspondence Navya C. N., MBBS, MD, DNB, Department of Anesthesiology, SriMuthukumaran Medical College Hospital and Research Institute, Chennai 600069, Tamil Nadu, India (e-mail: drcn.navya@gmail.com).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim
The aim of this study was to compare the extent of analgesia in terms of duration of analgesia and requirement of postoperative analgesics with preemptive analgesia and transversus abdominis plane (TAP) block in patients undergoing inguinal hernioplasty.
Materials and Methods
Ninety male patients aged between 18 and 65 years of American Society of Anesthesiologists grades I and II undergoing open inguinal hernioplasty were randomly allocated to three comparable groups of 30 each. Control group (group C) received normal saline; preemptive group (group P) received inj. paracetamol, inj. diclofenac, and inj. Lignocaine; and TAP group (group T) received TAP block with 20 mL of 0.25% bupivacaine at the end of surgery. Parameters recorded were verbal numerical rating scale (VNRS) at rest at 4, 12, 24, and 48 hours and VNRS on movement at 12, 24, and 48 hours; heart rate and mean arterial pressure at 0, 4, 12, and 48 hours; time for first analgesic request; and total doses of analgesics consumed at 24 hours.
Results
Demographic data were comparable. VNRS on movement and number of doses of analgesics consumed at 24 hours were statistically less in group T (4.80 ± .761 hours); time for first request of analgesia was longer and this group had better patient satisfaction scores compared with other groups.
Conclusion
Both groups P and T provided better VNRS scores compared with group C. TAP block provided better VNRS scores on movement at 24 hours, lesser analgesic requirement, and better patient satisfaction score compared with other groups.
Keywords
preemptive analgesia
inguinal hernioplasty
postoperative analgesia
TAP block
Introduction
Around 75% of patients get inadequate or minimal pain alleviation after surgery.1 After surgery, untreated pain can limit a patient's ability to walk, as well as induce thromboembolism, myocardial ischemia, arrhythmia, and chronic pain.2
Continuous efforts have been made to successfully control postoperative pain. Multimodal pain management strategies, which include a mix of opioids (via systemic or neuraxial), nonsteroidal anti-inflammatory medications, and acetaminophen, as well as patient-controlled analgesia (PCA), are now utilized to manage pain following surgery. However, there are worries about the possibility of opioids being delivered systemically causing nausea, vomiting, sleepiness, and respiratory depression.3 There is a recent surge of interest in intravenous (IV) lignocaine for perioperative pain management, due to its nonrespiratory depression properties.
The transversus abdominis plane (TAP) block is a technique for blocking the sensory nerves of the anterior abdominal wall that has been utilized to alleviate discomfort in many cases following abdominal surgery.4
In the postoperative pain management of hernioplasty, various therapy approaches have been advised. The majority of them have been shown to be unreliable.3 To the best of our knowledge, there are many studies comparing different block strategies and the usage of multiple medications, but none of them compare the two. As a result, the goal of this prospective study was to see how effective preemptive multimodal analgesia (IV paracetamol, diclofenac, and lignocaine) and postoperative TAP block were on unilateral inguinal hernioplasty in terms of verbal numerical rating scale (VNRS) at rest and movement, first analgesic request, and total number of postoperative analgesics consumed and to compare the potential adverse effects such as postoperative hemodynamics, nausea, and vomiting.
Materials and Methods
After receiving Institutional Ethical Committee clearance, this prospective, double-blind, randomized clinical trial was registered in the Clinical Trial Registry of India with registration number CTRI/2021/07/035189 and conducted from July to December 2021. The clinical trial was performed in compliance with the Helsinki Declaration 2013's ethical criteria for medical research involving human beings. The study comprised 90 male patients aged between 18 and 65 years who were undergoing elective unilateral inguinal hernia surgery under general anesthesia and were of American Society of Anesthesiologists grade I and II. All patients gave written informed consent. During the preanesthetic examination, all of the patients were taught VNRS scoring. Patients with known allergies or hypersensitivity to study drugs or procedures, such as those with kidney/liver illness, asthma, obesity, ischemic heart disease, poorly managed hypertension/diabetes mellitus, or known allergies or hypersensitivity to research agents were excluded.
A computer-generated randomization table was used to assign patients to group C (control group), group P (preemptive), and group T (TAP block). An anesthesiologist who was not involved in data collection performed allocation concealment using sequentially numbered, coded, sealed envelopes that were decoded at the end of the trial.
Patients in group C received a 100 mL normal saline (NS) infusion, 3 mL saline injected in 100 mL NS, and 5 mL saline half an hour before surgery, as well as a unilateral TAP block with 20 mL saline at the end of operation to maintain double blinding. Inj. paracetamol 15 mg/kg in 100 mL NS infusion, inj. diclofenac 75 mg IV infusion, and inj. lignocaine 1 mg/kg diluted to 5 mL with NS 30 minutes before surgery, and TAP block with 20 mL saline at the end of operation were given to group P. Thirty minutes before surgery, group T had a 100 mL NS infusion, 3 mL of NS injected in crystalloid, and 5 mL of NS IV, as well as a TAP block with 20 mL of 0.25% bupivacaine at the end.
Preparation of study drugs: Thirty minutes before surgery, all patients received study drugs prepared in identical infusion bottles and syringes labeled as drug A, B, and C, which included drug A–100 mL NS with either 2 mL NS (group C and T) or paracetamol 15 mg/kg (group P), drug B–100 mL NS with 3 mL of NS (group C and T)/diclofenac 75 m (group P) for TAP block, patients received 20 mL of NS (groups C and P) or 20 mL of 0.25% bupivacaine (group T) in a 20 mL sterile syringe made under aseptic conditions and retained in the spinal tray at the conclusion of operation.
Patients were given oral alprazolam (0.5 mg) the night before surgery and were kept nil per oral for 6 hours. Upon entering the premedication area, an 18G IV cannula was placed for drug delivery, and all patients received IV pantoprazole (40 mg). The patients' baseline heart rate (HR), blood pressure, and oxygen saturation were attached to routine standard monitors such as continuous electrocardiography, noninvasive blood pressure, and pulse oximeter. All patients received their IV study medicines A, B, and C 30 minutes before surgery, according to their group allocation. Vitals were monitored every 5 minutes for 30 minutes before being transferred to operation theater, where the same standard monitors were set up and vitals were monitored according to minimum standard monitoring guidelines.
All patients were given IV glycopyrrolate (0.05 mg/kg), IV midazolam (0.03 mg/kg), and IV fentanyl (2 mg/kg). Following preoxygenation, patients were induced with propofol at 1 to 2 mg/kg until the loss of verbal responsiveness. Patients were sedated with IV vecuronium 0.1 mg/kg and ventilated for 3 minutes before being intubated with an appropriate diameter endotracheal tube. Patients were on maintenance with a 60:40 mixture of oxygen and nitrous oxide, as well as isoflurane and vecuronium. IV ondansetron 0.15mg/kg was given 30 minutes before surgery ended.
TAP block was administered by an experienced anesthesiologist at the end of operation under sterile aseptic measures. At the midaxillary line, a 23 G 2.5-inch needle was placed at the point of Petit's triangle. The needle was advanced in the coronal plane perpendicular to the skin along the resistance of the external oblique muscle and further into the plane between the external and internal oblique fascial layers, resulting in the first pop sensation. The needle was then advanced along the resistance of the internal oblique muscle. As the needle reached the plane between the internal oblique and the transverse abdominis muscle, a second pop was felt. After negative aspiration, drugs were delivered according to group allocation. Patients were extubated following reversal and transported to a postanesthesia care facility
With an Aldrette score of >9, the patients were discharged from the postanesthesia care unit (PACU). When patients complained of discomfort, and pain score >4, they were given inj. diclofenac, and if the pain score remained >4, they were given inj. tramadol.
Given a 80% power and a 95% confidence interval for detecting a 10% difference in total number of analgesic doses consumed in 24 hours, the minimum sample size required was 26 participants in each group, which was rounded up to 30 participants in each group after accounting for 10% dropouts. The data was entered into an excel sheet and analyzed with SPSS Version 20 (Statistical Package for Social Sciences). As needed, descriptive statistics such as mean, standard deviation, and proportions (percentage) were calculated. Analysis of variance, independent sample t-test, and chi-squared test were employed to evaluate the hypothesis. Statistical significance was defined as a p-value of less than 0.05.
An investigator who was blinded to group allocation assessed and collected data at the following time points in the PACU and postoperative ward (0= immediately after surgery in PACU and 4, 12, 24, and 48 hours after surgery in postoperative ward). At 12, 24, and 48 hours, all patients were asked to rate their pain at rest and during movement (knee flexion), as well as the presence of nausea and vomiting noted. At each time point, HR and mean arterial pressure (MAP) were assessed. A VNRS (0 = no pain, 10 = extremely severe pain) was used to assess pain severity. A patient satisfaction score (0 = highly displeased, 10 = entirely satisfied) was used to assess the patient's satisfaction with the pain treatment after 48 hours. The first analgesic request was recorded, as well as the total amount of analgesics consumed in 24 hours.
Results
►Fig. 1 shows the Consolidated Standards of Reporting Trials (CONSORT) diagram where 97 patients were assessed for eligibility and 90 patients were included and their results analyzed. The patient characteristics and duration of surgery were comparable between the groups as shown in ►Table 1.

- CONSORT 2010 flow diagram.
| Parameter | Group C | Group P | Group T | ANOVA | Group P vs. group T |
|---|---|---|---|---|---|
| Age | 46.50 ± 15.49 | 47.33 ± 13.72 | 47.93 ± 13.24 | 0.92 (NS) | 0.864 (NS) |
| ASA 1 | 4.4% | 5.6% | 4.4% | 0.91 (NS) | 0.718 (NS) |
| ASA 2 | 28.9% | 27.8% | 28.9% | ||
| Weight | 67.73 ± 6.807 | 66.70 ± 6.727 | 67.43 ± 5.964 | 0.81 (NS) | 0.657 (NS) |
| Height | 163.60 ± 7.76 | 164.07 ± 6.01 | 164.03 ± 7.84 | 0.96 (NS) | 0.985 (NS) |
| Duration of surgery | 117.33 ± 13.9 | 118.33 ± 12.68 | 117.50 ± 15.41 | 0.95 (NS) | 0.820 (NS) |
Abbreviations: ANOVA, analysis of variance; ASA, American Society of Anesthesiologists; NS, not significant.
Mean and standard deviation, percentage of total.
There was significant difference of VNRS at rest and on movement among the group till 24 hours and was comparable at 48 hours. On intercomparison between groups P and T, patients in group T had statistically lesser scores at rest till 12 hours (p-value = 0.000) and lower scores of VNRS on movement was till 24 hours (p-value = 0.040) (►Fig. 2).
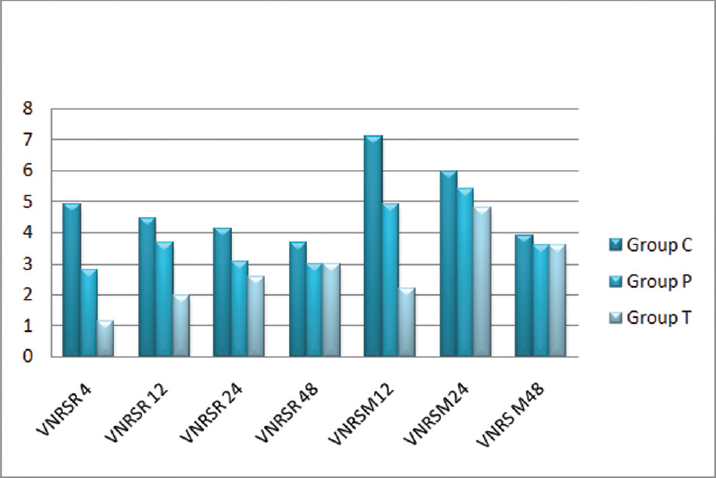
- Comparison of mean VNRS between the groups. VNRS, verbal numerical rating scale.
The time for first request of analgesia was significantly prolonged in group T (5.67 ± 0.9h) compared with others. The number of doses of analgesic administration was statistically lower in group T compared with group P and group C (►Table 2).
| Parameter | Group C | Group P | Group T | ANOVA | Group P vs. group T | |
|---|---|---|---|---|---|---|
| Time for first analgesic request in hours | 1.43 ± .504 | 3.60 ± 1.102 | 5.67 ± .994 | 0.000 (S) | 0.000 (S) | |
| Total number of analgesics consumed in 24 hours | 4.50 ± .509 | 3.57 ± .504 | 2.23 ± .430 | 0.000 (S) | 0.000 (S) | |
| Patient satisfaction score | 4 | 1.1% | 0.0% | 0.0% | 0.000 (S) | 0.000 (S) |
| 5 | 21.1% | 8.9% | 1.1% | |||
| 6 | 6.7% | 14.4% | 8.9% | |||
| 7 | 4.4% | 10% | 5.6% | |||
| 8 | 0.0% | 0.0% | 17.8% | |||
Abbreviations: ANOVA, analysis of variance; S, significant.
Data in mean and standard deviation and % total.
At the end of 48 hours, 63% of patients in group C had satisfaction score of 5 and the maximum score of 7 in 13% of patients. Forty-three percent of patients in group P had score of 6 and 30% had score of 7. Fifty-three percent of patients in group T had pain satisfaction scores of 8 (►Table 2). Four patients in group P complained of nausea and epigastric pain which was statistically significant. None of the patients had vomiting/itching. The postoperative mean HR and MAP were comparable between the groups.
Discussion
Preemptive analgesia is a treatment that begins before and continues throughout the surgical procedure to diminish the physiological effects of nociceptive transmission induced by the procedure. It has the potential to be more effective than identical analgesic medication given after surgery because of its “protective” effect on the nociceptive pathways. As a result, immediate postoperative pain may be decreased, and chronic pain development may be avoided.5,6
For preemptive analgesia, a variety of medications and procedures are employed.7,8 Concerns about opioid dangers in the postoperative phase have sparked a surge in interest in nonopioid analgesic adjuncts. The effects of a perioperative lignocaine infusion and a single dosage of lignocaine on postoperative pain have been studied.9–11 In this trial, a bolus dose of lignocaine was chosen for the group P, along with paracetamol and diclofenac.
The anterior rami of the lower six thoracic nerves (T6 – T12) and the first lumbar nerve innervate the skin, muscles, and parietal peritoneum of the anterior abdominal wall (L1). Between the transversus abdominus muscles and the internal oblique, terminal branches of these somatic nerves run through the lateral abdominal wall that constitute the TAP.12
Aweke et al13 used a preemptive paracetamol per os and intramuscular diclofenac combination and found that the time for first analgesic request was 103.01 ± 23.53 minutes, which was lower than our study of 3.60 ± 1.102. This is likely due to the route of administration, which decreased the bioavailability of the drugs, as well as the fact that they used fentanyl 50 µg intraoperatively, whereas we used fentanyl at higher dose. Furthermore, because lignocaine was given in conjunction with IV paracetamol and diclofenac in this trial, we observed a longer duration of analgesia.
Ibrahima et al14 discovered that TAP block with 30 mL bupivacaine (0.25%) gives excellent postoperative analgesia and greatly reduces the need for PCA fentanyl and pain scores in kidney transplant recipients after 24 hours. In the TAP block group, postoperative fentanyl requirements considerably reduced by 48% in the first 24 hours. In patients undergoing inguinal hernia repair, Aguirre-Ospina et al15 used 20 mL of 0.25% bupivacaine for TAP block. Pain and opiate use were lower in the intervention group than in the group C at 24 hours postoperatively, which is similar to our findings.
TAP block enabled effective hemodynamic control in the intraoperative period, provided effective pain control in the postoperative period, and decreased levels of the proinflammatory cytokines tumor necrosis factor-alpha and interleukin-1 in the first postoperative 24 hours, indicating immunomodulatory effect, according to Canakci et al,16 who used 20 mL of 0.5% bupivacaine.
VNRS scores in group P were lower in this study than in the group C, with a maximum score of 7 in 30% of patients and VNRS 6 in 43% of patients. The majority of the patients reported pain when moving. A total of 73% of patients received a score of 6 to 8. Patients in group P had a high rate of nausea and epigastric pain, which was treated with inj. pantoprazole and inj. ondansetron.
In group T, the VNRS scores were considerably lower. Despite the fact that participants in group T scored an 8 on postoperative day 1, practically all of them complained of visceral pain. However, in group T, the time taken to request first analgesic was longer, and the overall number of analgesic doses used in 24 hours was likewise much lower. In this study, we did not consider the visceral pain separately nor did we compare chronic pain. These two elements could be compared in future studies.
Conclusion
In comparison to the group C, preemptive analgesia and TAP block resulted in lower VNRS scores and higher patient satisfaction. Patients with TAP block had a longer duration of analgesia and a lower necessity for postoperative analgesia than the other groups. In the group P, nausea and epigastric pain were common side effects.
Financial Support
Nil.
Acknowledgments
Our sincere thanks to the OT staff, Department of Anaesthesiology.
Conflict of Interest
None declared.
References
- Pre- and post-operative patient\'s reactions to postoperative pain. Chungbuk Med J. 2007;17:182-189.
- [Google Scholar]
- Surgical stress: the role of pain and analgesia. Br J Anaesth. 1989;63(02):189-195.
- [CrossRef] [PubMed] [Google Scholar]
- Preoperative preemptive drug administration for acute postoperative pain: a systematic review and meta-analysis. Eur J Pain. 2016;20(07):1025-1043.
- [CrossRef] [PubMed] [Google Scholar]
- The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg. 2007;104(01):193-197.
- [CrossRef] [PubMed] [Google Scholar]
- Neuronal plasticity: increasing the gain in pain. Science. 2000;288(5472):1765-1769.
- [CrossRef] [PubMed] [Google Scholar]
- Preemptive analgesia–treating postoperative pain by preventing the establishment of central sensitization. Anesth Analg. 1993;77(02):362-379.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective double-blind randomised study of a new regimen of pre-emptive analgesia for inguinal hernia repair: evaluation of postoperative pain course. Eur J Surg. 2000;166(07):545-551.
- [CrossRef] [PubMed] [Google Scholar]
- Perioperative use of intravenous lidocaine. Anesthesiology. 2017;126(04):729-737.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of a single dose of lidocaine and ketamine on intraoperative opioids requirements in patients undergoing elective gynecological laparotomies under general anesthesia. A randomized, placebo controlled pilot study. Farm Hosp. 2016;40(01):44-51.
- [Google Scholar]
- Comparison of postoperative quality of recovery and pain relief with preoperative single-dose dexamethasone and lignocaine after laparoscopic cholecystectomy. Anesth Essays Res. 2018;12(03):630-635.
- [CrossRef] [PubMed] [Google Scholar]
- Transversus abdominis plane block: a cadaveric and radiological evaluation. Reg Anesth Pain Med. 2007;32(05):399-404.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of preemptive paracetamol, paracetamol-diclofenac & paracetamol-tramadol combination on postoperative pain after elective abdominal surgery under general anesthesia, Ethiopia: a randomized control trial study, 2018. BMC Anesthesiol. 2020;20(01):191.
- [Google Scholar]
- Efficacy of the transversus abdominis plane block using 30 ml bupivacaine 0.25% in reducing postoperative fentanyl requirements in renal transplant recipients. Ain-Shams Journal of Anaesthesiology.. 2017;10(01):258-263.
- [Google Scholar]
- Bloqueo del planotransversodel abdomen en herniorrafia inguinal. Ensayoclínicocontrolado. Rev ColombAnestesiol.. 2017;45:159-165.
- [CrossRef] [Google Scholar]
- Efficacy of ultrasound-guided Transversus Abdominis Plane (TAP) block in inguinal hernia surgery and the immunomodulatory effects of proinflammatory cytokines: prospective, randomized, placebo-controlled study. Braz J Anesthesiol. 2021;71(05):538-544.
- [CrossRef] [PubMed] [Google Scholar]







