Translate this page into:
Minimally Invasive Osteosynthesis in Elderly Osteoporotic Proximal Humerus Fractures Using J-Nailing Technique
Address for correspondence Akshay Babarao Ingale, MBBS, MS, DNB, Plot No. 34, Pathan Layout, Sambhaji Nagar, Nagpur 440022, Maharashtra, India (e-mail: koolakshay22@gmail.com).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction
Proximal humerus fractures in the osteoporotic elderly population are increasing and difficult to treat. Treatment in proximal fracture fixation in elderly has changed from absolute stability to relative stability that preserves soft tissue and vascularity, thereby improving clinical outcomes.
Aims and Objectives
This study aimed to evaluate the clinical outcome of proximal humerus fractures in osteoporotic patients using minimally invasive J-nailing technique.
Methods and Materials
A prospective observational study was done on 25 patients with proximal humerus fractures belonging to Neer's classification type 2 and 3 operated between May 2018 and June 2020 in the department of orthopaedics in tertiary health care center and treated by multiple intramedullary blunt Kirschner wires (J-nailing technique). The patients were followed up at 2, 6, 12, and 36 weeks. At the end of follow-up, clinical outcome was assessed using Neer's scoring system.
Results
Treatment of proximal humerus fractures with J-nailing technique in the elderly population has shown promising results both in terms of function and radiology. Mean union time was 13.48 weeks with a standard deviation of 1.19 weeks. We did not find any significant difference in union time between patients with fracture type 2-part and 3-part. However, there was a significant difference in Neer's scoring between patients with fracture types two-part and three-part.
Conclusion
Proximal humerus fracture fixation using minimally invasive techniques with J-nailing is an effective method of stabilization in elderly osteoporotic population, yielding good mechanical alignment, protecting rotator cuff muscles, preserving blood supply and predictable union rates with good clinical results.
Keywords
J-nailing
proximal humerus fractures
elderly
Introduction
Proximal humerus fractures are common in the elderly population and often faced by treatment dilemmas. Proximal humerus fractures are the third most common nonvertebral osteoporotic fractures in population aged above 65 years predominantly affecting females.1,2 Age-related osteoporosis and domestic fall play an important risk factor for proximal humerus fractures. Other risk factors include diminished vision and hearing, decreased cognitive ability, and comorbidity.3 Fractures debilitate otherwise a fit elderly group who contributes to the society.4 Therefore, conservative approach severely makes such population dependent and affects the quality of life. However, recent studies suggest a minimally invasive approach would result in better clinical outcome. Due to extensive soft tissue dissection, poor purchase of screws in head and tuberosity osteoporotic fragments, crushing of bones at the time of injury, the results of open reduction, and plating are disastrous. With minimally invasive approach, relative stability can be achieved that maintains vascularity and soft tissue integrity. Favorable results of arthroplasty in other joints have not been replicated in shoulder; hence, literature with arthroplasty in the shoulder is continuously expanding.5 Although various treatment modalities have been described in literature, none have shown a clinically favorable outcome as compared with nonoperative methods.6
Our study aimed at managing osteoporotic two-part and three-part proximal humerus fractures in the elderly population with minimally invasive J-nailing technique and studying clinical as well as the radiological outcome.
Materials and Methods
An observational prospective study was done that involved proximal humerus fractures belonging to Neer's two-part and Neer's three-part fracture in an elderly patient aged above 60 years. Among fracture types 13 belonged to two-part fracture and 12 belonged to three-part fracture. The sample size involved patients attending our casualty services between May 2018 and June 2020.
There were 16 female and 9 male patients with age ranging from 60 to 81 years. Approval of the hospital ethics committee was sought. Inclusion criteria were closed unstable proximal humerus fractures belonging to Neer's two-part and three-part fracture sustained within 2 weeks without neurovascular injury in an elderly patient aged above 60 years. The exclusion criteria were compound, pathological fractures, patients with Neer's four-part fracture and fracture-dislocation of the proximal humerus, and patients with previous injuries that who already compromised function. The comorbidities in each patient were taken into account as the study was dealing with elderly patients. Charlson comorbidity index (CCI) was noted for each patient (►Table 1).
| Scorea | Comorbid condition |
|---|---|
| 1 | Myocardial infraction |
| Congestive heart failure | |
| Cerebral vascular disease | |
| Peripheral vascular disease | |
| Dementia | |
| Chronic obstructive pulmonary disease | |
| Connective tissue disease | |
| Peptic ulcer disease | |
| Mild liver disease | |
| Age | |
| 2 | Diabetes |
| Hemiplegia | |
| Moderate/several renal disease | |
| Diabetes with end-organ damage | |
| Any solid tumor | |
| Leukemia | |
| Lymphoma | |
| 3 | Moderate/several liver disease |
| 6 | Metastatic solid tumor |
| Acquired immunodeficiency syndrome |
a1 point is added to patients aged between 41 and 50 years, 2 points for those aged between 51 and 60 years, 3 points for those aged between 61 and 70 years, and 4 points for those 71 years or older.
Fractures were assessed with anteroposterior and axillary view radiographs of the shoulder and on computed tomography when feasible. A thorough history and clinical examination were done for the patient. Other associated injuries were noted. Plain radiographs of the involved limb with adjoining joint were taken. The patient was operated after written informed consent and anesthesia clearance.
The patient was admitted 1 day prior to surgery and discharged 2 days after the procedure.
The patient was operated under general or regional anesthesia in the supine position with sandbag underneath the injured extremity with the affected limb on a sidearm post. Image intensifier was brought from the headend to get good-quality orthogonal views. A 1.5 to 2.5 cm longitudinal skin incision is taken in subdeltoid region anterolaterally. After soft tissue dissection deep down to the bone, the first entry hole is made with 2.5 to 3.0 mm Kirschner wires (K-wires) at an oblique angle to gain entry into the medullary canal. Three separate entry holes are made in a configuration that avoids stress riser (►Fig. 1). The tips of K-wire 2.5 mm or 3.0 mm are cut and made blunt to avoid penetration. The blunt tips of K-wire are bent in required configuration, brought up to fracture and then the reduction maneuver is done. The reduction maneuver consists of traction abduction and external rotation of shoulder that counteracts deforming forces. The tuberosity fracture fragments and varus angulation of head are manipulated using percutaneous K-wire if required. All the wires are hammered rather than drilling that prevents back out. The wires are directed into areas of maximum bone density and fanned out. One intramedullary wire is directed to support the calcar region endosteally. The K-wires are cut plied bent and buried under the skin. Additional percutaneous K-wires may be placed to fix tuberosity fragments. Postoperatively, the patient is placed in a shoulder immobilizer for 6 weeks.7

- Multiple intramedullary Kirschner wire (K-wire) on a bone model depicting configuration of K-wires to avoid stress riser.
Injection Cefotaxim was administered for 2 days and discharged on postoperative day 2. Passive closed chain movements of the shoulder are started within 7 to 10 days of surgery. Active-assisted and active range of motion exercises are encouraged at 4 weeks as per patient's tolerance to pain and cooperation. The patient is followed up for radiographic evidence of healing. Pins are removed after consolidation on plain radiographs. Neer's scoring system was used for the assessment that includes 35 points for pain, 30 for function, 25 for range of motion, and 10 for anatomy. A score of 90 to 100 points was considered excellent; 80 to 90 points was considered satisfactory; 70 to 79 points was considered unsatisfactory; and seventy points or less was considered failure8 (►Table 2).
| Functional | |
|---|---|
| Pain | Scores |
| No pain | 35 |
| Slight, occasional, no compromise in activity | 30 |
| Mild, no effect on ordinary activity | 25 |
| Moderate, tolerable, makes concessions | 15 |
| Marked, serious limitations | 5 |
| Totally disabled | 0 |
| Function | |
| Strength–normal | 10 |
| Good | 8 |
| Fair | 6 |
| Poor | 4 |
| Trace | 2 |
| Zero | 0 |
| Reaching–top of head | 2 |
| Mouth | 2 |
| Belt buckle | 2 |
| Opposite axilla | 2 |
| Brassiere hook | 2 |
| Stability–lifting | 2 |
| Throwing | 2 |
| Pounding | 2 |
| Pushing | 2 |
| Hold overhead | 2 |
| Range of motion | |
| Flexion–180 degrees | 6 |
| 170 degrees | 5 |
| 130 degrees | 4 |
| 100 degrees | 3 |
| 80 degrees | 2 |
| < 80 degrees | 1 |
| Abduction–180 degrees | 6 |
| 170 degrees | 5 |
| 140 degrees | 4 |
| 100 degrees | 3 |
| 80 degrees | 2 |
| < 80 degrees | 1 |
| Extension–45 degrees | 3 |
| 30 degrees | 2 |
| 15 degrees | 1 |
| < 15 degrees | 0 |
| External rotation–60 degrees | 5 |
| 30 degrees | 3 |
| 10 degrees | 1 |
| < 10 degrees | 0 |
| Internal rotation–90 degrees | 5 |
| 70 degrees | 4 |
| 50 degrees | 3 |
| 30 degrees | 2 |
| < 30 degrees | 0 |
| Anatomy (rotation, angulation) | |
| None | 10 |
| Mild | 8 |
| Moderate | 4 |
| Marked | 0 – 2 |
| Results | |
| 90 – 100 points | Excellent |
| 80 – 89 points | Satisfactory |
| 70 – 79 points | Unsatisfactory |
| < 70 points | Failure |
Statistical Analysis
Results were assessed using mean, standard deviation, Student's t-test, and Pearson's correlation coefficient. A p-value of less than 0.05 was considered significant. The results were entered in MS Excel spreadsheets, and statistical analysis was performed using Statistical Package for Social Sciences (SPSS) version 16.0.
Results
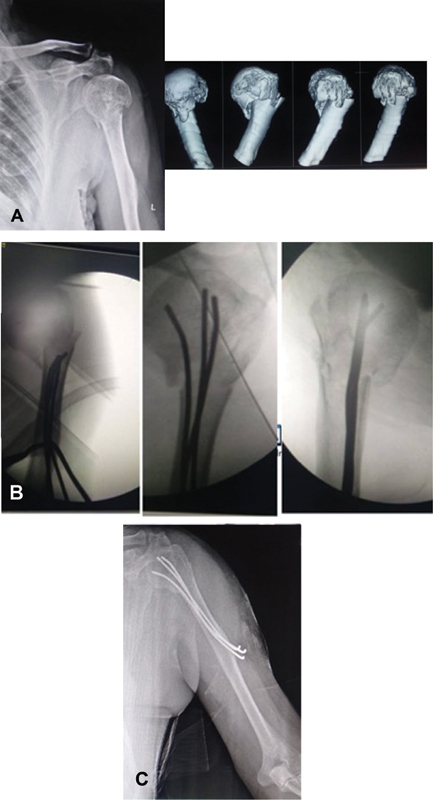
Our study comprised a total of 25 elderly patients, in which 9 patients were male and 16 patients were female. The mean age was 69.76 years and a standard deviation was 7.19 years (range: 60 – 81 years). The most common mode of injury was domestic fall (17 patients) followed by a road traffic accident (8 patients). The right upper limb was involved in 15 patients, while the left upper limb was involved in 10 patients. Thirteen patients were two-part fractures and 12 were three-part fractures. Mean surgical delay was 4.4 days with a standard deviation of 2.31 (range: 2 – 8 days). Mean surgical time was 44.56 minutes with a standard deviation of 5.84. The mean Neer's scoring at the end of follow-up was 80.04 with a standard deviation of 8.79. The mean union time was 13.48 weeks with a standard deviation of 1.19 weeks. All the patients were available for follow-up. Cases illustrated for Neer's type 2 and type 3 are shown in ►Figs. 2 and 3.

- Case 2–(A) Preoperative imaging of patient with two-part proximal humerus fracture in a 77-year-old male. (B) Intra- and postoperative radiographs of the same patient. (C) Follow-up radiographs of the same patient.
- Case 1. (A) Preoperative imaging of patient with Neer's three-part proximal humerus fracture in a 68-year-old female. (B) Intra- and postoperative radiographs of the same patient. (C) Follow-up X-ray with union at 13 weeks.
The mean hospital stay was 3.8 days. The mean CCI was 4.56.
Pearson's correlation coefficient for CCI with union time was weakly negative (r= −0.04).
In Neer's two-part fracture concerning Neer's score, five patients had excellent outcome, four had a satisfactory outcome, three had unsatisfactory outcome, and one had a poor outcome. The mean Neer's score in two-part fracture was 83.92. The mean union time in two-part fracture was 13.23 weeks.
In Neer's three-part fracture concerning Neer's score, one patient had excellent outcome, four patients had a satisfactory outcome, four patients had unsatisfactory outcome, and three patients had a poor outcome. The mean Neer's score in three-part fracture was 74.91. The mean union time in three-part fracture was 13.75 weeks.
There was a statistically significant difference between fracture type and Neer's scoring (p = 0.018). There was no statistically significant difference between fracture type and union time (p = 0.28).
Pearson's correlation coefficient for Neer's scoring with advancing age was weakly negative (r = − 0.19).
Pearson's correlation coefficient for union time with advancing age was weakly positive (r = 0.304).
Malunion with varus angulation was observed in three patients.
With regard to the complication, one patient had implant prominence with the removal of implants done after the radiological union was achieved.
One patient had superficial infection observed at the drilled site of K-wire insertion for fixing tuberosity, treated by oral antibiotics.
There were no cases of implant perforation into the shoulder joint, breakage, and radial nerve injury.
No complication of nonunion and avascular necrosis was seen in follow-up period.
Discussion
Management of proximal humerus fractures in the elderly population often is a matter of debate and great dilemma.9 Proponents of operative approach often favor a minimally invasive approach in a fit elderly population as these people still contribute to the society and fracture in such cases hampers the quality of life. Various treatment options are available for proximal humerus fractures.9 In the yesteryears, these fractures were often treated conservatively. Due to the advent of internal fixation devices, the management of fractures has changed from conservative to operative procedures. But the outcome in proximal humerus fractures when operated still has not been able to show a promising result due to overwhelming complications.
Also, considerable data are lacking in proximal humerus fractures in the elderly population as operative and nonoperative treatment both have shown similar outcome results.10
Surgical management is associated with complications and with the cost puts a health burden over the patients. Surgical management prognosis is dependent on various factors like age, osteopenia, surgical skills, fracture geometry, soft tissue injuries, and rehabilitation protocol.11
Internal fixation with locking plate in osteoporotic bones though has certain advantages, it has been associated with screw penetration, screw cut-out, loss of medial support causing varus failure and extensive soft tissue dissection, loss of vascularity, and infection.12
Augmentation with cement, support with a fibular graft to fill the medial void and support calcar, titanium mesh cage, and endosteal plate are some of the recent advances in the proximal humerus fracture fixation.13–15
Intramedullary nailing multiple locking options though is minimally invasive approach, the risks far outweigh the benefits. The major disadvantage with intramedullary nailing is rotator cuff violation that affects the clinical outcome. Also, intervention with nailing is possible only in certain fracture subtypes of proximal humerus.16
Closed reduction with percutaneous pinning has benefits of minimal soft tissue injury that maintains the vascularity and accelerates fracture healing. However, the major pitfalls associated with percutaneous pinning are pin loosening, pin migration, pin tract infections due to drilling of pins, loss of fixations, and axillary nerve injury.17
Reverse shoulder arthroplasty has been increasingly used in proximal humerus fracture. However, the prerequisites of the cost of the implant and proper patient selection often make the use of replacement procedures in elderly vulnerable.18,19
Minimally invasive approach with J-nailing technique involves minimal soft tissue dissection away from the zone of injury, maintains vascularity, and is cost-effective. Multidirectional blunt tip K-wires get a better fixation and hold in osteoporotic bones. Strategic planned placement of wires supports the calcar area and reduces varus collapse. Moreover, the subdeltoid insertional area does not hamper any joint motion due to tethering of muscles. As regards with other modality, there is no extensive soft tissue injury; no rotator cuff violation hammering rather than drilling and arching of K-wire and multiple point fixation reduces backing of the J nail. The burying of pins under the skin further prevents pin site infection, though in some patients implant prominence can be an issue. Rehabilitation protocol can be started soon after the patient tolerates pain. Implant removal is also easy as K-wires are buried and bent just under the skin.
Complications such as malunion are known to occur but preventable by proper and acceptable reduction. Poor outcomes in our study were due to the poor status of rotator cuff and tuberosity malunion and stiffness, but they were minimally hampering activities of daily living in the elderly.
Avascular necrosis and nonunion although occur by other treatment modalities, the chances of such complications, however, are negligible by J-nailing technique.
All the surgeries were done by single surgeon (1st author).
Our study is unique as literature has very few such studies in elderly osteoporotic age group.
The limitations of our study were small sample size, no comparative group, and exclusion of four-part fractures.
Conclusion
Minimally invasive fixation of proximal humerus fractures with multiple intramedullary blunt K-wires (J-nailing technique) has shown promising results in elderly osteoporotic population. We conclude that this technique is quite economical, offers less hospital stay, reduces the risk of infection, and provides an effective and safe treatment option along with better functional outcome in the elderly population.
Conflict of Interest
None declared.
References
- Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology. 1996;7(06):612-618.
- [CrossRef] [PubMed] [Google Scholar]
- Nondisplaced proximal humeral fractures: high incidence among outpatient-treated osteoporotic fractures and severe impact on upper extremity function and patient subjective health perception. J Shoulder Elbow Surg. 2011;20(05):795-801.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for fractures of the proximal humerus: results from the EPIDOS prospective study. J Bone Miner Res. 2002;17(05):817-825.
- [CrossRef] [PubMed] [Google Scholar]
- The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001;72(04):365-371.
- [CrossRef] [PubMed] [Google Scholar]
- Reverse shoulder arthroplasty for the treatment of proximal humeral fractures. Hand Clin. 2007;23(04):425-430. v–vi
- [CrossRef] [PubMed] [Google Scholar]
- Five-year follow-up results of the PROFHER trial comparing operative and non-operative treatment of adults with a displaced fracture of the proximal humerus. Bone Joint J. 2017;99-B(03):383-392.
- [CrossRef] [PubMed] [Google Scholar]
- Minimally invasive fixation for unstable two-part proximal humeral fractures: surgical techniques and clinical results using j-nails. J Orthop Trauma. 2002;16(06):403-408.
- [CrossRef] [PubMed] [Google Scholar]
- Comparability of patient-reported outcome measures and clinical assessment tools for shoulder function in patients with proximal humeral fracture. Z Orthop Unfall. 2021;159(06):638-648.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of proximal humerus fractures in the elderly: a systemic review of 409 patients. Acta Orthop. 2015;86(03):280-285.
- [CrossRef] [PubMed] [Google Scholar]
- Operative vs non-operative management of displaced proximal humeral fractures in the elderly: a systematic review and meta-analysis of randomized controlled trials. World J Orthop. 2015;6(10):838-846.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with the decision for operative versus non-operative treatment of displaced proximal humerus fractures in the elderly. Injury. 2013;44(04):448-455.
- [CrossRef] [PubMed] [Google Scholar]
- Complex fractures of the proximal humerus in the elderly–outcome and complications after locking plate fixation. Musculoskelet Surg. 2012;96(01):S3-S11.
- [CrossRef] [PubMed] [Google Scholar]
- Cement augmentation of the proximal humerus internal locking system in elderly patients: a multicenter randomized controlled trial. Arch Orthop Trauma Surg. 2019;139(07):927-942.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of the effects of proximal humeral internal locking system (PHILOS) alone and PHILOS combined with fibular allograft in the treatment of Neer three- or four-part proximal humerus fractures in the elderly. Orthop Surg. 2019;11(06):1003-1012.
- [CrossRef] [PubMed] [Google Scholar]
- Indirect reduction and strut support of proximal humerus fractures using a titanium mesh in elderly patients: a novel technique. J Orthop Trauma. 2020;34(04):e142-e147.
- [CrossRef] [PubMed] [Google Scholar]
- Third- generation intramedullary nailing for displaced proximal humeral fractures in the elderly: quality of life, clinical results, and complications. Arch Orthop Trauma Surg. 2022;142(02):227-238.
- [Google Scholar]
- Percutaneous pinning for proximal humerus fracture. Rev Med Chir Soc Med Nat Iasi. 2007;111(01):184-189.
- [Google Scholar]
- Hemiarthroplasty versus reverse total shoulder arthroplasty for acute proximal humerus fractures in elderly patients. Orthopedics. 2012;35(05):e703-e708.
- [CrossRef] [Google Scholar]
- Expanding roles for reverse shoulder arthroplasty. Curr Rev Musculoskelet Med. 2016;9(01):40-48.
- [CrossRef] [PubMed] [Google Scholar]







