Translate this page into:
Outcome of Laparostomy as a Treatment Measure for Abdominal Compartment Syndrome: A Retrospective Study
How to cite this article: Kumar ESS, Singh SA, Sagar BV, Chithambaram N, Jeyasekharan S, Jeyasekharan D. Outcome of laparostomy as a treatment measure for abdominal compartment syndrome: A retrospective study. Int J Recent Sur Med Sci doi: 10.1055/s-0043-1761457
Abstract
Introduction
Abdominal compartment syndrome is a life-threatening condition that affects critically ill patients. When pressures inside a fixed cavity of the body increases, ischemia, muscle injury, and organ failure can result.
Aim
To assess the benefits and outcomes of laparostomy for abdominal compartment syndrome.
Methods
This retrospective study included patients who underwent a laparostomy procedure as a treatment measure for abdominal compartment syndrome, secondary to different etiologies such as sepsis and major abdominal visceral trauma.
Results
Although there are a few complications such as incisional hernia in the future following a laparostomy, the mortality rate following the procedure is less than < 10%, thus ensuring a good prognosis for patients who present with acute surgical emergencies. It could also be further noted that an early closure by 7 to 14 days had definite beneficial outcomes as compared with delayed closure of more than 14 days. It prevented most long-term complications such as entero-atmospheric fistula formation or granuloma formation, the outcomes of which were further aided by the use of a transparent custom-made polypropylene mesh.
Conclusion
Laparostomy is the gold standard treatment for abdominal compartment syndrome. The use of a custom-made polypropylene mesh has proven to have the least complications in the follow-up period. Incisional hernias are the most common complications documented, followed by entero-atmospheric fistula.
Keywords
Laparostomy
Gangrene bowel
Abdominal trauma
Abdominal compartment syndrome
Introduction
Laparostomy is a surgical procedure in which the abdominal cavity is opened and left open deliberately because of a difficult primary closure or when primary closure is avoided due to severe intra-abdominal sepsis, trauma, and risk of abdominal compartment syndrome.[1] The World Society of Abdominal Compartment syndrome (WSACS) has defined abdominal compartment syndrome (ACS) as a sustained intra-abdominal pressure (IAP) of > 20 mm Hg with the presence of an attributable organ failure. Although it is commonly confused with the term intra-abdominal hypertension (IAH), WSACS defines intra-abdominal hypertension as a sustained or repeated pathological elevation in IAP of ≥12 mm Hg and does not have any associated organ damage.[2] Though surgeons in south India do not commonly do laparostomy, we in our institute have been performing laparostomy as a treatment modality for the last three decades. Thus, a retrospective study was conducted, and all data information for the study was obtained from previous medical records at the hospital.
Materials and Methods
This retrospective study was conducted among patients who presented to the surgical intensive care unit (ICU), were diagnosed with abdominal compartment syndrome of both infective and traumatic origin, and were treated with laparostomies over 10 years. Further, follow-up on these patients was done on an out-patient basis (OP) basis to determine their complications from the surgery. A total of 75 patients were seen during 10 years, from January 2011 to December 2020. Ethics committee approval and scientific committee approval were obtained.
Inclusion criteria
All surgical patients admitted in the surgical ICU underwent a laparostomy procedure as a treatment measure for ACS, secondary to different etiologies such as sepsis and major abdominal visceral trauma.
Patients age between the age of 18 years and 75 years.
Patients with prior co-morbidities such as diabetes mellitus, hypertension, chronic kidney disease, liver cell failure, malignancies, chronic lung diseases, and ischemic heart diseases.
Exclusion criteria
Pregnant patients.
Patients less than 18 years of age and more than 75 years of age.
Abdominal trauma is associated with other associated injuries such as long bone fracture, chest wall injury, head injury, pelvic fractures, and spine injury.
Laparostomies performed for etiologies other than the abdominal origin.
Loss of follow-up on patients.
Methodology
Data collection, analysis, and interpretation were used for the study. Mean, standard deviation, and percentage of occurrence were calculated to estimate the ratio of prevenances in the population. All data regarding the study population were collected from previous medical records stored in the data drive in PDF formats. Manual collection of data was done and the results were obtained by calculating the mean, median, and standard deviation.
In our hospital, laparotomy is performed at a point of an inter-abdominal pressure of more than 20 mmHg. The method of performing an open abdomen in our hospital involves procedures such as bowel resection, end-to-end anastomosis, and leaving the abdomen open. Following the procedure, a temporary closure technique, using a custom-made polypropylene mesh is sutured into place with interrupted stay sutures using 1–0 prolene. The patient is covered using a custom-made laparostomy belt with adjustable tags, which secure the incision and closure in place. Drains are sutured into the place in the perihepatic pouch or pelvic cavity depending on the procedure done to further prevent the accumulation of intra-abdominal free fluid. Follow-up dressing and closure were done serially as per the patient's need.
Clinical variables
Indications for surgery
Type of surgery done
Associated organ damage
Period of closure-early or delayed
Complications in the post-surgical period
Cause of death
Statistical methods
Data were collected and presented as mean, standard deviation, frequency, and percentage.
Results
Laparostomies were performed with no restrictions on age or gender. From the data collected, each age group seems to have an almost equal distribution of ACS; however, the etiology they developed had pre-dominances in specific age groups. The younger age group needed laparostomies mainly secondary to complications arising out of appendicular surgeries or trauma. The elderly group had more predominance toward mesenteric infarcts due to mesenteric thrombosis or strangulated hernias. Similarly, it was also noted that laparostomies were more predominant in males than females to a ratio of more than 2:1 [Tables 1 and 2].
Age group |
Frequency |
Percentage |
|---|---|---|
<30 |
17 |
22.7% |
31–40 |
6 |
8.0% |
41–50 |
14 |
18.7 |
51–60 |
14 |
18.7 |
61–70 |
13 |
17.3 |
71–80 |
11 |
14.6 |
Total |
75 |
100.0 |
Gender |
Frequency |
Percentage |
|---|---|---|
Male |
53 |
70.7 |
Female |
22 |
29.3 |
Total |
75 |
100 |
There were several different etiologies involved, which caused a rise in the intra-abdominal pressure. Peritonitis, hemoperitoneum, and intestinal obstruction were the three most commonly encountered conditions in our study. In all, 82.7% of the patients were noted to have peritonitis, 17.3% of the patients had hemoperitoneum secondary to abdominal visceral traumas such as RTAs. Out of 82.7% cases with peritonitis, 9.3% of cases were due to appendicular complications such as appendicular gangrene and abscess, and 22.7% of the cases were due to intestinal obstruction, 24.0% of the cases were due to bowel perforation due to complications such as ulcers, and 12.0% due to bowel gangrene seen to secondary due to mesenteric infarcts and thrombosis. Another 14.7% of cases had laparostomy performed secondary to abdominal abscesses such as a pancreatic abscess. On the traumatic side, hemoperitoneum seen secondary to visceral trauma had 17.3% of the total cases due to mesenteric tear and liver injury [Figure 1 and Table 3].
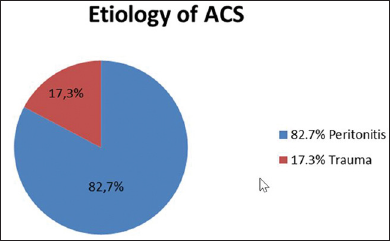
- Etiology of ACS.
Etiology |
Frequency |
Percentage |
|---|---|---|
Appendicular complications |
7 |
9.3 |
Intestinal obstruction |
17 |
22.7 |
Bowel perforation |
18 |
24.0 |
Bowel gangrene |
9 |
12.0 |
Abdominal abscess |
11 |
14.7 |
Total |
62 |
82.7 |
To completely understand the outcome of a laparostomy procedure, it is also important to consider the preoperative complications that the patients presented with. In most cases, it could be noted that by the time the patients present to the surgical ICU, secondary organ damage and its resultant consequences have set in. Out of the 75 cases considered in the study, 53 cases presented with sepsis associated with metabolic acidosis and acute kidney injury, and 8 cases had evidence of acute respiratory distress syndrome. Another presentation mainly noted in the traumatic origin was hypovolemic shock with hypothermia, seen secondary to trauma, which accounted for 11 cases. A small number of cases (3) presented with DIC and coagulopathy. A few cases had more than one of these complications [Table 4].
Secondary complications |
Frequency |
Percentage |
|---|---|---|
Sepsis |
53 |
70.7 |
ARDS |
8 |
10.6 |
Hypovolemic shock |
11 |
14.7 |
DIC |
3 |
4.0 |
Total |
75 |
100 |
Another important factor to consider is the type of surgery the patient underwent, which ended up with a laparostomy for a closure technique. The most commonly noted bowel resection is mainly seen secondary to gangrenous ileum or duodenum due to mesenteric vein thrombosis, resection anastomosis of the perforated colon, jejunum, and other parts of the intestinal loops. The other more common ones worth noting are appendicular-related surgeries, exploratory laparostomy, adhesiolysis, and perforation of the duodenum following Graham's patch closure [Table 5].
Procedures |
Frequency |
Percentage |
|---|---|---|
Bowel resection |
34 |
45.4 |
Appendicular complications |
7 |
9.3 |
Duodenal perforation closure |
18 |
24.0 |
Adhesiolysis |
5 |
6.7 |
Exploratory laparotomy |
4 |
5.3 |
Others |
7 |
9.3 |
Total |
75 |
100 |
Considering the closure period, it could be noted that 88% of the population study had early closure or the same admission closure. This closure period varies from 7 days to 14 days. In contrast, 9 cases comprising 12% of the total study population had delayed closure, the period of which varies from 14 days to as long as 42 days. However, only two people from the delayed closure period developed incisional hernias in the post-operative period [Figure 2].
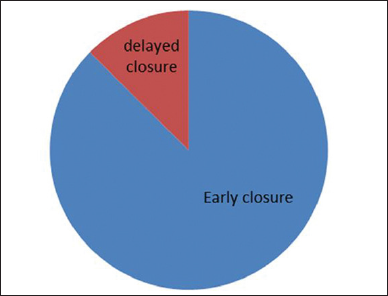
- Closure period.
There are a certain number of complications that arise from performing a laparostomy. In our study, it was seen that 22.7% of the cases developed ventral hernias. This is the most common complication seen in patients and presents 4 of 5 years post-surgery. Thus, choosing the correct temporary closure plays a vital role in this condition. Other complications noted are entero-atmospheric fistula (2.7%) and death. Four cases died due to non-surgical complications.
Four deaths documented in the study had secondary complications before the surgery. Two cases had acidosis with coagulopathy and hypothermia, while the other two had sepsis with metabolic acidosis and secondary organ damage such as acute respiratory distress syndrome. Therefore, the prognosis of these cases could be skewed by their respective complications. A point worth noting is that 94.7% of the population that underwent the procedure survived their life-threatening condition, with 69.3% of the patients having an uneventful postoperative period with no complications such as hernia or fistula formation [Table 6].
Outcome |
Frequency |
Percentage |
|---|---|---|
No complications |
52 |
69.3 |
Ventral incisional hernia |
17 |
22.7 |
Entero-atmospheric fistula formation |
2 |
2.7 |
Mortality |
4 |
5.3 |
Total |
75 |
100 |
Discussion
Laparostomy or open abdomen is a commonly employed surgery for the treatment of ACS. It differs in the fact that the abdomen is left open with a temporary closure technique in situ. These temporary closure techniques involve the usage of Bogota bags, a vacuum-assisted system with polypropylene mesh, or even custom-made polythene sheets.[2] However, the need for an open abdomen should be weighed against the patient's physical health condition and the benefits of other conservative treatments.[3,4]
Treatment measures for abdominal compartment syndrome can be both medical and surgical. However, there is no clear-cut evidence so far to compare the medical methods with surgical methods to prove the benefits of either. Most medical managements can only provide temporary relief. Abdominal perfusion pressure (APP) is the difference between mean arterial pressure and intra-abdominal pressure. Targeting an APP of more than 60 mm Hg has been proposed as a better predictor of outcome in IAH than measuring IAP.
Medical management can be used as neuromuscular blockade, which helps to relax the abdominal wall muscles and hence increase the intra-abdominal volume.[5] However, this is only a temporary measure and is limited by time. In certain situations such as colonic wall edema, the use of diuretics has also proven some efficacy in reducing bowel wall edema and distension. However, the focus should be more on the controlled intake of fluids rather than the removal of fluids with the use of diuretics.[6] The administration of pro-kinetics has also shown certain benefits by aiding in the evacuation of bowel contents. However, it must also be kept in mind that medical management is a temporary measure and only aids in preventing the progression of organ damage while adding time for the preparation of surgical intervention.
There are significant benefits in using the open abdomen technique, such as reducing intra-abdominal pressure and easy access to the abdomen in re-exploratory laparotomy. It also gives us the advantage of inspecting the bowels serially, assessing the color of the bowel and peristalsis, and checking for bile or fecal content leakage [Figure 3].
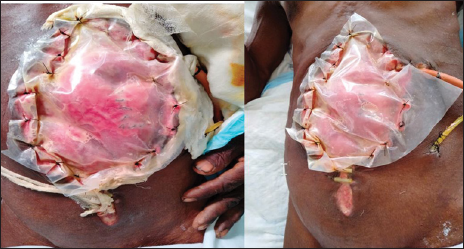
- Shows the temporary closure technique for a laparostomy using custom made polypropylene mesh.
A recent study in the European Journal of Surgery, early fascial closure for patients with extensive abdominal wall defects would result in at least a 50% recurrence rate of abdominal wound dehiscence.[7] It has been noticed that early fascial closure may be associated with a high mortality rate of the open abdomen due to its induced visceral compression and IAH.[8] However, this was seen more true toward cases who had a closure period of 3 days or less. In our study, the early closure period was from day 7 to day 14. In all, 88% of the study population had early closure and only 12% of the remaining population had delayed closure, out of which 3% developed incisional hernia later. Thus, proving that an adequate wait period of at least 7 days, even in the cases of early closure, had significant benefits in terms of mortality and other complications.
Similarly, a recent, well-conducted randomized study comparing an on-demand to a planned relaparotomy strategy in patients with severe peritonitis showed that the on-demand group had a substantial reduction in relaparotomy, health care utilization, and medical costs.[9] Only seven cases required relook surgeries in our hospital. Out of these seven cases, four cases required resection of gangrenous bowel noticed in the relook procedure, while three had fecal fistula leak. There is no particular evidence to show that a relook surgery increased the chances of developing complications such as fistula or ventral hernia.
Fifty-five percent of the patients with primary closure techniques developed an incisional hernia in a study conducted in Bonn, Germany.[10] Similarly, a study on the complications of using Bogota bags showed that 65.45% of the cases needed skin grafting or healing by the formation of granulation tissue, leading to the development of hernias in the future.[11] The overall incidence of incisional hernia after laparotomy was 9.9%. The incidence was significantly higher for midline incisions compared with transverse incisions.[12] The study conducted in our hospital found that 22.7% of the population developed incisional hernias, of which 3% had a delayed closure after 7 days on the post-surgical period, some extending until 30 days. A custom-made polypropylene mesh with interrupted sutures was used as the temporary closure technique in the study, which has shown a reduction in the overall occurrence of incisional hernias as compared with other studies
A study conducted in Amsterdam, Netherlands, showed that 44 cases (77%) reported the occurrence of fistulae as a complication of TAC (temporary abdominal closure).[13] The incidence of developing a new entero-atmospheric fistula when VAC (vacuum-assisted closure) is applied reaches an average of 5.7% (ranging from 0% to 15%).[14] Another 9.09% developed a small bowel fistula.[10] A clear advantage noted in our study is how only 2.7% of the entire population had a fistula. It was also found to be significantly smaller in number than its occurrence in other techniques. This could be attributed to 88% of all cases having an early admission closure in 7 to 14 days of their postoperative period [Figure 4].

- Shows closure of the laparostomy incision with the formation of entero-atmospheric fistula.
In a study conducted in China in 2012, it was said that compared with delayed abdominal closure, early fascial closure significantly reduced mortality (12.3% vs. 24.8%, RR, 0.53, p < 0.0001) and complication incidence (RR, 0.68, p < 0.0001)[15] and mentioned before it was found to reduce at least 50% of the mortality.[7] Our study conducted in this hospital showed that out of 75 patients, only 4 patients had mortality, while 71 patients survived. All patients who survived had an early closure period with a few having complications such as incisional hernia. The mortality of these four patients could also be attributed to the fact they had complications before the surgery, such as sepsis, metabolic acidosis, hypothermia, hypovolemia, and coagulopathy.
Conclusion
Though the treatment of using laparostomy is quite tedious, requiring immense knowledge and skills, it plays a vital role in providing a good prognosis to patients in an acute emergency. Similarly, though several closure techniques have been followed to date, the use of a custom-made polypropylene mesh has proven to have the least complications during the follow-up period. For example, incisional hernia is the most common complication documented, followed by entero-atmospheric fistula. New methods can be developed in the future to avoid these complications, further emphasizing laparostomy as the gold standard treatment for abdominal compartment syndrome.
Conflict of interest
None declared.
References
- Outcomes and associated factors among patients undergone emergency laparotomy: a retrospective study. Int J Surg Open. 2021;36:100413.
- [CrossRef] [Google Scholar]
- Temporary intravenous bag silo closure in severe abdominal trauma. J Trauma. 1996;40:258-60.
- [CrossRef] [PubMed] [Google Scholar]
- Paracentesis for resuscitation-induced abdominal compartment syndrome: an alternative to decompressive laparotomy in the burn patient. J Trauma. 2006;60:1119-21.
- [CrossRef] [PubMed] [Google Scholar]
- Abdominal compartment syndrome: risk factors, diagnosis, and current therapy. Crit Care Res Pract. 2012;2012:908169.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Results from the international conference of experts on intra-abdominal hypertension and abdominal compartment syndrome. I. definitions. Intensive Care Med. 2006;32:1722-32.
- [CrossRef] [PubMed] [Google Scholar]
- Abdominal compartment syndrome: often overlooked conditions in medical intensive care units. World J Gastroenterol. 2020;26:266-78.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Unacceptable results of the Mayo procedure for repair of abdominal incisional hernias. Eur J Surg. 1998;164:361-7.
- [CrossRef] [PubMed] [Google Scholar]
- To close or not to close, that is one of the questions? Perceptions of Trauma Association of Canada surgical members on the management of the open abdomen. J Trauma. 2006;60:287-93.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of on-demand vs planned relaparotomy strategy in patients with severe peritonitis: a randomized trial. JAMA. 2007;298:865-72.
- [CrossRef] [PubMed] [Google Scholar]
- Long term outcome after open abdomen treatment: function and quality of life. Front Surg. 2021;8:590245.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Small bowel fistulas and the open abdomen. Scand J Surg. 2007;96:263-71.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and prevention of ventral incisional hernia. J Visc Surg. 2012;149(5, Suppl):e3-e14.
- [CrossRef] [Google Scholar]
- Temporary closure of the open abdomen: a systematic review on delayed primary fascial closure in patients with an open abdomen. World J Surg. 2009;33:199-207.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Surgical techniques for the management of enteroatmospheric fistulae. Surg Infect (Larchmt). 2009;10:47-52.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of outcomes between early fascial closure and delayed abdominal closure in patients with open abdomen: a systematic review and meta-analysis. Gastroenterol Res Pract. 2014;2014:784056.
- [PubMed] [PubMed Central] [Google Scholar]







