Translate this page into:
The Utility of Bone Marrow Aspirate Injection in Comminuted Femur Fractures: Does it Improve Functional and Radiological Outcomes?
*Corresponding author: Dr. Pranav Kapoor, Department of Orthopaedics, Sharda University, Noida, Uttar Pradesh, India. drpranavkapoor007@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kapoor P, Mathiyalagen P. The Utility of Bone Marrow Aspirate Injection in Comminuted Femur Fractures: Does it Improve Functional and Radiological Outcomes? Int J Recent Surg Med Sci. 2024;10:114-20. doi: 10.25259/IJRSMS_43_2024
Abstract
Objectives
The study aimed to analyze the functional and radiological outcomes of prophylacticbone marrow aspirate injections (BMAI) in closed comminuted diaphyseal femur fractures treated with closed reduction internal fixation (CRIF) and compare it to those treated only with definitive fixation.
Material and Methods
Forty patients with closed comminuted diaphyseal femur fracture were enrolled and divided equally into two groups. The case group (n=20) prophylactically received bone marrow aspiration injection (BMAI) post 2 weeks of CRIF, and the control group (n=20) received CRIF treatment alone, without BMAI. The lower extremity functional scale (LEFS) and radiological criteria were employed to evaluate the output in both groups.
Results
Graphical representation of categorical variables showed a significant difference (p<0.05) at 26 weeks of follow-up. Delayed union was seen in 10% of patients from the case group and 45% of patients from the control group. Complications were minimal in the case group when compared to the control group (0% vs. 5%). The estimated LEFS score for the case group (68.592+0.524) was significantly higher than that of the control group (66.433+0.524) up till the 20th week. However, by the 26th week, there was no significant difference between the two groups, indicating that while BMAI accelerates recovery, the long-term functional outcomes might converge over time. The percentage of maximal function was higher for the BMAI group than for controls.
Conclusion
The reduced incidence of delayed union in the BMAI group demonstrated that BMAI significantly lowers the risk of delayed healing. The absence of non-unions in the BMAI group further supports the effectiveness of the BMAI in healing, both radiologically and functionally.
Keywords
Bone marrow aspiration injection (BMAI)
Closed femur fractures
Delayed union
Closed reduction internal fixation (CRIF)
Lower extremity functional score (LEFS)
INTRODUCTION
A shaft femur fracture is the most common fracture. Most orthopedic surgeons treat it with the ‘gold standard’ intramedullary nailing.[1] Closed femur comminuted fractures may lead to delayed union or non-union (14% incidence).[2] This complication is a significant issue faced by many orthopedic surgeons, and the treatment modalities commonly suggested to these patients range from dynamic nailing and exchange nailing to screw and plate fixation and external fixation. These procedures may be accompanied with bone grafting and growth factors to enhance the healing of the fracture non-union.[3]
Bone marrow (BM) contains the pluripotent stem cells and the progenitor cells required for new bone formation.[4] The stages of bone healing require these cells to interact with each other for healing to occur. These molecular entities thus induce osteogenesis on injection into animal cells, showing non-union.[4] This concept is used in BM injection at fracture sites. BM injected at the time of definitive fixation or shortly after may prevent the burden of delayed union or non-union. Percutaneous BMAI does not require surgical exploration of the delayed union site, thus minimizing infection. The settled union site is not disturbed, maintaining the vascularity of the fracture site. Treating delayed union pre-emptively corrects the future non-union process, as reported by many researchers.[4,5] So, injecting BM mesenchymal cell aspirates at the fracture site supplemented by the primary fixation process, though seems perplexing, should be tried. This is the objective of this current study.
Though several studies dictate the advantages of BMAI on long bone fractures, the prophylactic role of iliac crest BMAI on comminuted fracture of femur shaft, treated with primary fixation, presents a gap in the literature. Hence, we undertook this study to evaluate the functional and radiological outcome of prophylactic BMAI in closed comminuted diaphyseal femur fractures treated with intramedullary nailing.
MATERIAL AND METHODS
Study design
This prospective observational study was conducted on consenting patients visiting the hospital outpatient/inpatient/emergency department. Between August 2022 and December 2023, 40 patients enrolled, all of which were adults with closed comminuted long bone fractures undergoing surgical fixation. The inclusion and exclusion criteria are given in Supplementary Table 1. All patients qualified as per the inclusion criteria were divided into 2 groups. The case group (n=20) was given BMAI 2 weeks post suture removal after primary fixation of the closed comminuted long bone fracture. In contrast, the control group (n=20) was only given CRIF treatment without BMAI.
Written informed consent was obtained from all the patients, and they were briefed on the treatment plan, operational cost, hospital stay after surgery, and complications of anesthesia. Both groups were followed up every 6 weeks till 26 weeks after surgery and were clinically and radiologically assessed for fracture healing, joint movements, and implant failure. Three radiological criteria were assigned. The fracture was scored as excellent if it united in 20 weeks, good if the fracture united in 26 weeks, and poor if non-union was seen at 26 weeks. Functional evaluation was performed using LEFS where the patient was provided a questionnaire and inquired about the status of movement and bony union.
The operative technique of BM aspiration from the iliac crest
All the patients in the case group were placed in a supine position, and the fracture site and graft site were draped in a sterile fashion. At the site of aspiration, 2% xylocaine was locally administered. After making a stab incision, a Jamshidi needle was used to aspirate 10 ml of BM from the iliac crest. A lumbar puncture needle of gauge 16 was used to inject it into the fracture site. A compression dressing and an antibiotic course were given postoperatively [Figures 1 and 2].

- Administering local anesthesia to bone marrow aspiration injection (BMAI) site.
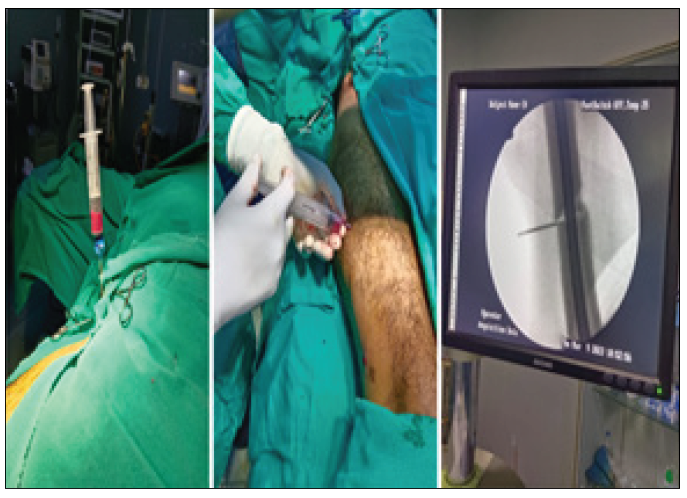
- Aspirating BM with a Jamshidi needle and injecting it into the fracture site.
RESULTS
Age and gender distribution
The age and gender distribution was not significantly different between the study groups [Table 1 and 2].
| Group | N | Mean±Std. deviation | Median (IQR) | P value |
|---|---|---|---|---|
| Case | 20 | 32.35±15.479 | 28.00(16) |
0.626 |
| Control | 20 | 32.90±12.908 | 33.00(18) | |
| Total | 40 | 32.63±14.071 | 30.00(18) |
Mann-Whitney U test was applied. IQR: Inter-Quartile range
| Sex | Group | Total N (%) | P value | |
|---|---|---|---|---|
| Case N (%) | Control N (%) | |||
| Female | 6 (30% | 8 (40%) | 14 (35%) | 0.507 |
| Male | 14 (70%) | 12 (60%) | 26 (65%) | (DOF=1) |
Chi-square test was applied. DOF: Degree of freedom.
Functional scoring assessment
Estimation of LEFS scoring
Data from LEFS scoring showed that the estimated score for the case group (68.592+0.524) was higher than the control group (66.433+0.524) (p=0.006) [Table 3]. A significant difference was observed between the two groups immediately after the operation and continued to be present in the 2nd, 8th, 14th, and 20th week. However, in the 26th week of follow-up, there was no statistical difference [Figure 3].
| Follow up | Group | N | Mean±Std. deviation | Median (IQR) | P value |
|---|---|---|---|---|---|
| Immediate postop | Case | 20 | 63.45±2.395 | 64.00(4.00) | <0.001 |
| Control | 20 | 59.10±2.654 | 60.00(4.00) | ||
| 2nd week | Case | 20 | 65.85±1.927 | 66.00(2.00) | <0.001 |
| Control | 20 | 62.40±1.903 | 62.00(3.00) | ||
| 8th week | Case | 20 | 68.05±2.704 | 68.00(3.00) | 0.001 |
| Control | 20 | 65.55±3.284 | 65.00(2.00) | ||
| 14th week | Case | 20 | 70.00±1.892 | 70.00(3.00) | 0.036 |
| Control | 20 | 68.45±2.350 | 69.00(3.00) | ||
| 20th week | Case | 20 | 74.45±2.743 | 74.00(5.00) | 0.031 |
| Control | 20 | 72.60±1.984 | 72.00(3.00) | ||
| 26th week | Case | 20 | 69.75±14.352 | 71.00(5.00) | 0.107 |
| Control | 20 | 70.50±3.472 | 71.00(4.00) |
Mann-Whitney U test was applied, IQR: Interquartile range.
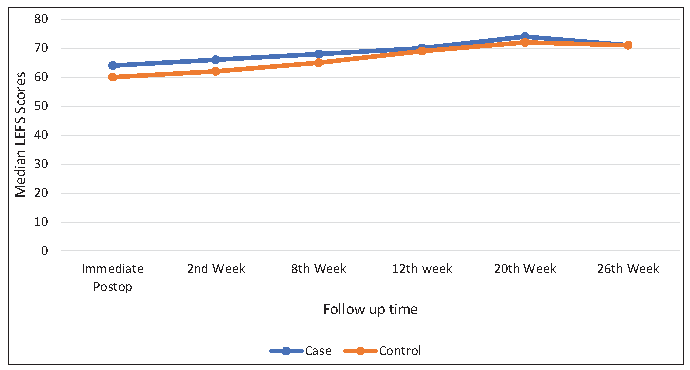
- Distribution of LEFS score among the study groups.
Distribution of percentage of maximal function (f%)
The f% distribution among the study groups was analyzed, revealing that the median (ƒ%) with inter-quartile range (IQR) among the case group was significantly higher (68.95±1.791, IQR=2) compared to that of the control group (66.10±1.518, IQR=3) (p value<0.001) [Table 4].
| Group | N | Mean± Std. deviation | Median (IQR) | P value |
|---|---|---|---|---|
| Case | 20 | 68.95±1.791 | 69.00(2) | |
| Control | 20 | 66.10±1.518 | 66.00(3) | <0.001 |
| Total | 40 | 67.53±2.184 | 68.00(3) |
Mann-Whitney U test was applied. IQR: Inter-Quartile range
Distribution of delayed union and non-union
The data from the distribution of delayed union among study groups showed that the incidence of delayed union was significantly lower in the BMAI group (10%) than in the control group (45%) (p=0.013). However, the non-union rates were 0% in the case group vs. 5% in the control group, showing no significant difference (p=1.000) [Figure 4 and Table 5].
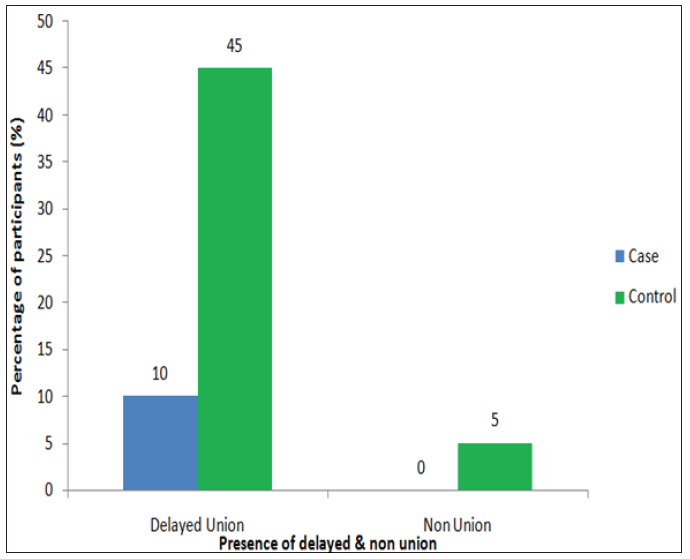
- Distribution of delayed union and non-union among study groups.
| Distribution | Group | Total N (%) | P value | |
|---|---|---|---|---|
| Case N (%) | Control N (%) | |||
| Delayed union | 2(10%) | 9(45%) | 11(27.5%) | 0.013*(DOF=1) |
| Non-union | 0(0%) | 1(5%) | 1(2.5%) | 1.000#(DOF=1) |
*Chi-square test and #Fisher exact test was applied.
Distribution of bony callus formation
As depicted in the bar graph [Figure 5], neither the case nor the control groups showed any stage of callus formation immediately post-operation or up to the 2nd-week follow-up. During the 8th week follow-up, 90% of cases and 50% of controls achieved callus formation in one out of four cortices. During the 14th week follow-up, 85% of cases and 35% of controls achieved callus formation in two cortices. During the 20th week follow-up, 75% of cases and 15% of controls achieved callus formation in three cortices. During the 26th week follow-up, 40% of cases and 10% of controls achieved callus formation in four cortices. The graph shows the significant progress in callus formation in the case group compared to the control group. There was a moderately significant positive correlation between LEFS scores and callus formation in the 20th week. However, this correlation was not significant in the 26th week. Figures 6 and 7 show the radiological union in the fractured lower shaft femur of two individual cases.
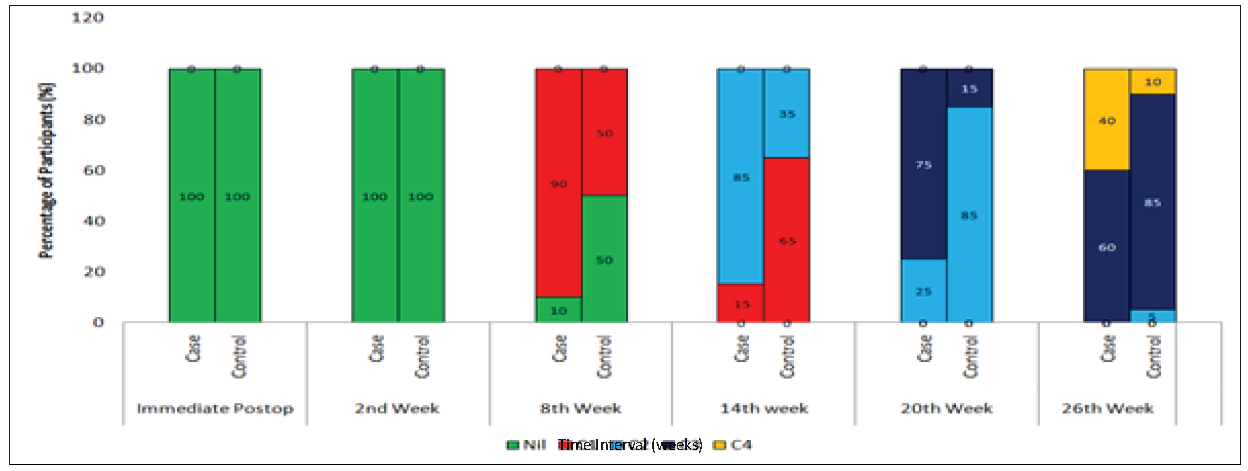
- Distribution of bony callus formation among the study participants.
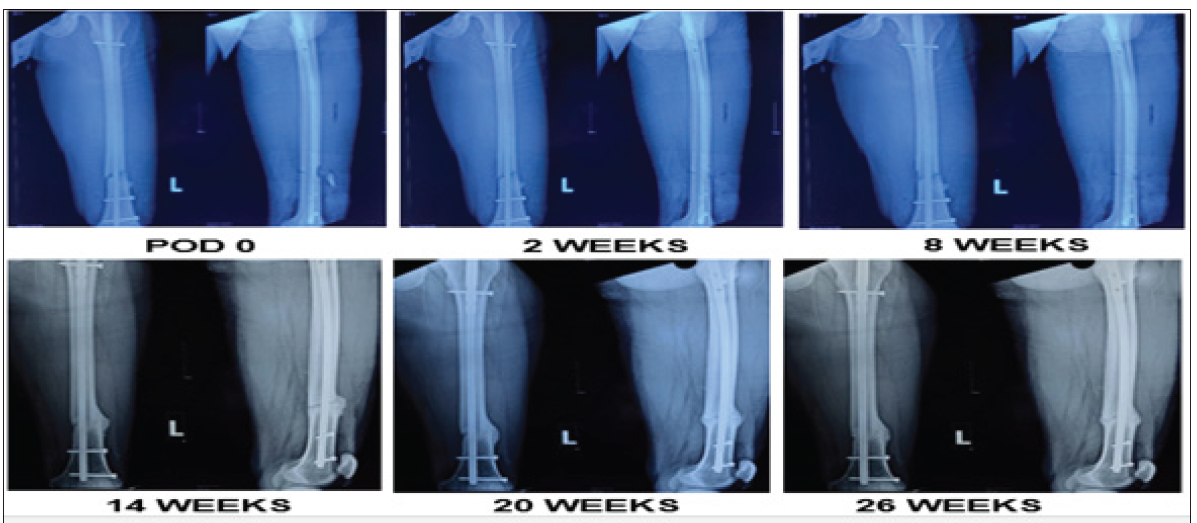
- Case 1. Radiological union in fractured lower shaft of the femur.
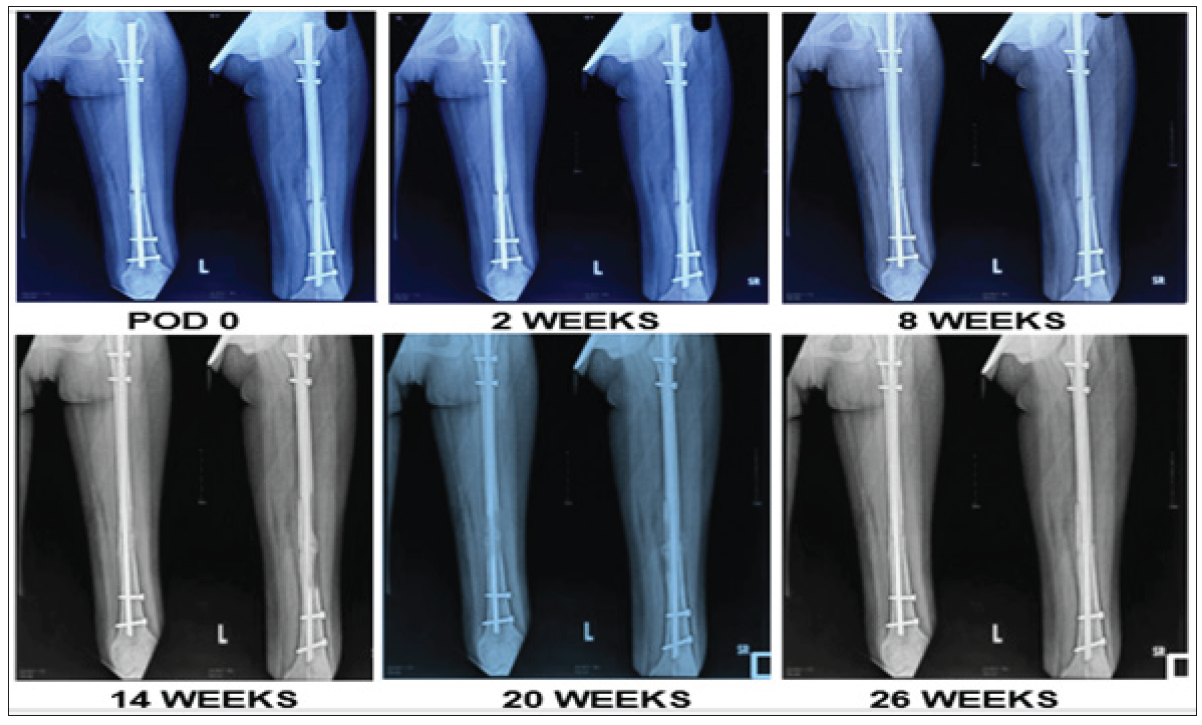
- Case 2. Radiological union in comminuted fracture shaft femur.
DISCUSSION
Non-union and delayed union of femur bone fractures are perplexing for orthopedic surgeons. Autologous bone grafting is commonly employed but is associated with adverse side effects. Less invasive options like BMAI, utilizing autologous stem cell therapy to enhance bone healing, present promising clinical outcomes with fewer complications.[6]
The current study demonstrated that prophylactic BMAI in combination with CRIF treatment significantly convalesce the radiological and functional outcomes in patients with closed comminuted diaphyseal femur fractures compared to standalone treatment with CRIF. The main findings revealed that the incidence of delayed union in the group of patients who received BMAI treatment was significantly lower than those who did not receive BMAI treatment. In addition, there were no cases of non-union in the BMAI-treated patients. Moreover, functional scoring, i.e. LEFS, was significantly higher in the BMAI-treated patients up to the 20th week procedure, indicating accelerated recovery. However, by the end of the 26th week, BMAI-treated and non-BMAI-treated patients showed similar functional outcomes, implying that while BMAI facilitates early recovery, the long-term functional benefits converge over time.
Previous studies suggest that autologous stem cells from the BM of a patient can enhance bone healing, especially in those showing delayed union or non-union of fractures.[7-10] Ma et al and Hasan et al., reported that iliac crest bone marrow injections avoid the risks associated with traditional bone grafting, such as immune reactions and donor site morbidity.[8,9] Numerous clinical studies advocate the advantage of using percutaneous autologous BMAI in showing good bony union at the fracture site.[11-13] Non-union at different fracture sites have been corrected by the use of calcium sulphate, autogenous bone powder or use of bone marrow mononuclear cells have shown good bone union.[14-16] Our findings align with these previous studies emphasizing the benefits of BMAI in enhancing bone healing and functional recovery. In our study, a lesser percentage of delayed union and absence of non-union in the BMAI-treated patients, along with a higher incidence of bony non-union in non-BMAI-treated patients, highlighted the significance of BMAI in promoting timely and complete bone healing. Further, in our study, we found that 75 % of patients showed excellent results, suggesting fracture union in 20 weeks. This is consistent with the findings of Parvez et al., who also graded fracture healing outcomes into excellent, good, and poor for fracture union or non-union and showed a higher percentage of “excellent” results in BMAI-treated patients.[11]
In our study, we found a good percentage of maximal function (ƒ%) in the BMAI group vis a vis the control group in improving the overall function. The data on callus formation stages provide compelling evidence of enhanced bone healing in the BMAI group. The progression from stage 1 to stage 4 callus formation was significantly faster and more prevalent in the BMAI group, indicating a more robust and expedited bone healing process. These findings were consistent with those of Sahu et al.[17]
Post the femur fracture rehabilitation phase, the patient’s physical functioning is of utmost importance. Besides this, monitoring the patient’s progress to optimize their treatment is also crucial. In our study, we used the LEFS questionnaire [Annexure No. 1] that served a critical role in forming a correlation with callus formation similar to the studies of Ratter et al.[18] and Lisan RA.[19] This correlation suggested that while functional improvement and bone healing are related, other factors also influence recovery. The moderate positive correlation of LEFS and callus formation in the 20th week, as found in our study, underscores the impact of early bone healing on functional recovery.
Hernigou et al.[10] and Braly et al. observed the benefits of hematopoietic stem cells as pluripotent cells (those that can differentiate into other cells) . These pluripotent cells from the BM decrease with smoking and the use of steroids and alcohol, indicating that the BMAI procedure has a high success rate in selected patients. In addition, as these pluripotent cells are located in the concentrated buffy coat, BMAI efficacy is favored by the density and concentration of stem cells available for injection, suggesting the use of concentrated BMAI to achieve the best results.[4] Using a similar methodological approach, our findings also align with these investigators who have shown a correlation between bone healing and the concentration of progenitor cells in BMAI. Significant progress in callus formation stages observed in the BMAI group than the control group further corroborates the effectiveness of BMAI in enhancing bone healing due to the usage of concentrated BMAI.
While efficacy is crucial for any therapeutic procedure, safety profile plays a critical role in decision-making for choosing an orthopedic procedure. Santhanam et al reported that the interval between external fixation and secondary nailing was found to be a significant determinant of radiological outcome at three months (p-value at 3 months=0.045) and better functional outcome at six months (p-value at 6 months=0.030) with patients undergoing secondary nailing within 10 days of external fixation having a good final outcome.[20]Belete et al reported that the magnitude of functional limitation in lower limb fracture individuals was considerably high in our study setup. Level of education, presence of hospitalized complications, severity of pain, duration of onset, and knee flexion limitation were the independent risk factors for functional limitation.[21] Similarly, in our study, we utilized iliac crest BMAI injections and observed no adverse reactions or complications at the aspiration site.
The study’s strong points constitute its prospective design and the use of the standardized LEFS score to gauge functional recovery. Furthermore, the study showed a precise scientific approach to BMAI delivery that might be applied in clinical settings. The strong outcomes, in terms of callus formation, delayed union, and non-union, provide strong evidence in favor of BMAI’s efficacious use as adjuvant therapy.
However, the study also had several limitations. Though the study design was prospective, the sample size was too small to conclude the lack of difference between the two groups. To evaluate the efficacy of the prophylactic BMAI procedure in diverse patient populations and confirm our findings, large randomized controlled clinical trials are needed. In addition, this procedure cannot be used in cases where there is an existing infection, open fracture, or femur shaft fractures treated with modalities other than interlocking (IL) intramedullary (IM) nailing or neglected fractures, narrowing the applicability of the results. Lastly, the results of the present study might have been affected by the surgical technique used in our department, which can challenge the generalizability of results. This implies a need for future studies across different clinical settings.
Taken together, the findings of this study highlight the significant benefits of BMAI in enhancing both functional recovery and bone healing in patients with closed comminuted diaphyseal femur fractures. However, further investigation is crucial to corroborate these outcomes for optimizing BMAI usage in orthopedic practice.
CONCLUSION
This study concludes that the BMAI group shows a more rapid improvement in lower extremity function post-surgery. While BMAI accelerates early recovery, the long-term functional outcomes might converge over time. For a better understanding of the effectiveness of BMAI in closed comminuted diaphyseal femur fractures treated with CRIF, randomized controlled trials with larger sample sizes should be conducted.
Author contributions
PK and ADS: Conceived, designed the study, conducted research, provided research materials, collated and organized the data;
PM: Analyzed and interpreted the data;
PK: All clinical aid and logistic support ;
ADS: Wrote the article with initial and final draft;
VKG: Corrected the last version of the article and supervised it to its final version. His true mentorship made the manuscript see its final version. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
Acknowledgments
The authors would like to thank the orthopedic and OR staff for their collaborative effort.
Ethical approval
The research/study was approved by the Institutional Review Board at Sharda University, number SU/SMS & R/76-A/2022-23, dated 7th July 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Intramedullary Nailing for Femoral Shaft Fractures in Adults. Cochrane Database Syst Rev. 2018;2018:CD010524.
- [CrossRef] [Google Scholar]
- Union Rates and Functional Outcome of Double Plating of the Femur: Systematic Review of the Literature. Arch Orthop Trauma Surg. 2022;142:1009-30.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- What is the Best Treatment of the Femoral Shaft Nonunion After Intramedullary Nailing? A systematic review. Life (Basel). 2023;13:1508.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Percutaneous Autologous Bone Marrow Injection in the Treatment of Distal Meta-Diaphyseal Tibial Nonunions and Delayed Unions. J Orthop Trauma. 2013;27:527-33.
- [CrossRef] [PubMed] [Google Scholar]
- The Effect of Autologous Concentrated Bone-Marrow Grafting on the Healing of Femoral Shaft Non-Unions After Locked Intramedullary Nailing. Injury. 2014;45:S7-S13.
- [Google Scholar]
- Fractures of the Lower Extremity. In: Canale ST, Beaty JH, eds. Campbell’s Operative Orthopedics (12th edition). Elsevier Mosby; 2013. p. :2681-88.
- [Google Scholar]
- The Treatment of Acute Diaphyseal Long-Bones Fractures with Orthobiologics and Pharmacological Interventions for Bone Healing Enhancement: A Systematic Review of Clinical Evidence. Bioengineering (Basel). 2020;7:22.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- [Clinical Observation on Percutaneous Autologous Bone Marrow Grafting for Treatment of Fracture Nonunion] Zhongguo Gu Shang. 2009;22:862-4.
- [PubMed] [Google Scholar]
- Bone Marrow Aspirate Injection Technique in the Treatment of Scaphoid Fracture Utilizing Percutaneous Screw Fixation. Acad J Health Sci. 2024;39:155-62.
- [Google Scholar]
- Percutaneous Autologous Bone-Marrow Grafting for Nonunions. Surgical Technique. J Bone Joint Surg Am. 2006;88:322-7.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous Autologous Bone Marrow Injection in the Treatment of Delayed Union of Long Bone Fractures After Definitive Fixation. Indian J Orthopaedics Surg. 2022;8:10-16.
- [CrossRef] [Google Scholar]
- Percutaneous Internal Fixation of Proximal Fifth Metatarsal Jones Fractures (Zones II and III) With Charlotte Carolina Screw and Bone Marrow Aspirate Concentrate: An Outcome Study in Athletes. Am J Sports Med. 2011;39:1295-301.
- [CrossRef] [PubMed] [Google Scholar]
- Injection of Demineralized Bone Matrix with Bone Marrow Concentrate Improves Healing in Unicameral Bone Cyst. Clin Orthop Relat Res. 2010;468:3047-55.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Successful Treatment of Refractory Tibial Nonunion Using Calcium Sulphate and Bone Marrow Stromal Cell Implantation. J Bone Joint Surg Br. 2007;89:1382-6.
- [CrossRef] [PubMed] [Google Scholar]
- A Study of 23 Unicameral Bone Cysts of the Calcaneus: Open Chip Allogeneic Bone Graft Versus Percutaneous Injection of Bone Powder with Autogenous Bone Marrow. Foot Ankle Int. 2008;29:164-70.
- [CrossRef] [PubMed] [Google Scholar]
- Cell-Based Therapy by Autologous Bone Marrow-Derived Mononuclear Cells for Bone Augmentation of Plate-Stabilized Proximal Humeral Fractures: A Multicentric, Randomized, Open Phase IIa Study. Stem Cells Transl Med. 2024;13:3-13.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Percutaneous Autogenous Bone Marrow Injection for Delayed Union or Non-Union of Long Bone Fractures After Internal Fixation. Rev Bras Ortop. 2017;53:668-73.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Content Validity and Measurement Properties of the Lower Extremity Functional Scale in Patients with Fractures of the Lower Extremities: A Systematic Review. J Patient Rep Outcomes. 2022;6:11.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Comparison of Pre-And Post-Implantation of Indonesian-Made Plates in Fracture Patients: Functional, Radiological, Biomechanical and Chemical Analyses. Narra J. 2024;4:e752.s.
- [Google Scholar]
- Factors Determining the Functional and Radiological Outcome After Secondary Nailing in Open Fractures of Lower Extremity- a Prospective Cohort Study. J Clinical Diag Res. 2022;16:RC01-RC04.
- [CrossRef] [Google Scholar]
- Assessment of Functional Limitation and Associated Factors in Adults with Following Lower Limb Fractures, Gondar, Ethiopia in 2020: Prospective Cross-Sectional Study. Orthop Res Rev. 2021;13:35-45.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







