Translate this page into:
What Else to Pay Attention in Terms of Bone Health Other than Osteoarthritis among Candidates Undergoing Total Knee Replacement: Observations in a Subset of Indian Population
Address for correspondence Sonam Dubey, MBBS, MD, F- 203, F-Type Building, Government Medical College Shahdol Campus, Shahdol, Madhya Pradesh 484001, India (e-mail: sonamdubeyrewa@gmail.com).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background
Earlier it was thought that osteoarthritis and osteoporosis were mutually exclusive but many studies now prove that these diseases coexist. This study was undertaken to assess the bone health in terms of mineral density and other markers among patients undergoing total knee replacement due to osteoarthritis.
Methods
A total of 100 patients with advanced osteoarthritis undergoing total knee replacement and satisfying inclusion and exclusion criteria were selected. Detailed social, medical, personal, and family history was recorded. All participants underwent for dual-energy X-ray absorptiometry scan (spine and both hips), X-rays (both knees and pelvis), Western Ontario and McMaster Universities osteoarthritis index (WOMAC) scoring, and serum levels of vitamin D, calcium, phosphorus, alkaline phosphatase, and Parathyroid hormone (PTH). Data collected and analyzed.
Results
In total, 87% of total participants were females. Mean values for age, height, weight, serum vitamin D3, serum PTH, serum calcium, serum phosphorus, serum alkaline phosphatase, WOMAC score, and bone mineral density (BMD) score (T-score) were 65.35 years, 160.15 cm, 69.37 kg, 26.91 ng/mL, 48.02 pg/mL, 9.01 mg/mL, 3.40 ng/mL, 57.91 IU/L, 56.32, and −1.16, respectively.
Conclusion
Osteopenia and osteoporosis seem prevalent in the Indian population with advanced knee osteoarthritis. Our findings do not support the hypothesis of inverse relation between osteoarthritis and lower BMD. The study reflected poorer bone health and lesser average age for Indian patients undergoing total knee replacement.
Keywords
arthroplasty
dual-energy X-ray absorptiometry
osteoarthritis
osteoporosis
parathyroid hormone
Introduction
Osteoarthritis (OA) is the most common form of arthritis, and the commonest cause of disability among adults.1,2 Knee OA tends to impose great burden to populations, as the resulting pain and stiffness often lead to significant disability requiring total knee replacement.3 OA of the knee is more common in women as well as in elderlies, so age and sex are both risk factors for development of OA.2–4 Age and female sex are also high risk factors for development of osteoporosis.5–7
In most previous studies, it was indicated that these two diseases were inversely related.8,9 The prevalence of osteoporosis in patients undergoing hip and knee arthroplasty was found to be low. Hip and knee arthroplasty patients had higher bone mineral density (BMD) than an age-matched general population.10 But other studies do not support their mutually exclusive nature.11
Orthopaedicians while taking care of advanced OA might show little interest in osteoporosis care. The high costs of medication and lack of awareness among physicians and patients about coexistent diseases could be the most important barriers.12,13 The role of antiresorptive drugs (bisphosphonates) in pain management and periprosthetic bone loss prevention indirectly supports osteoporosis as a contributor in postoperative pain (and implant loosening) in arthroplasty.14
A retrospective review of 723 patients undergoing surgery at an orthopedic hospital revealed that 40% of patients were vitamin D-deficient.15 Similarly, in a large prospective study, those with the lowest vitamin D3 levels at baseline had the most rapid progression to knee OA.16
Interplay of 25-hydroxyvitamin D3 (vitamin D), parathyroid hormone (PTH), calcium, phosphorus, alkaline phosphatase, etc. is responsible for bone health and these are recorded simultaneously here along with BMD that is rare in existing related Indian studies.
Our primary objective was to determine prevalence of poor bone health in patients with severe OA undergoing total knee replacement in a subset of Indian population. A secondary objective was to compare the trend with that described for populations abroad.
Methods
Study design
Hospital-based, cross-sectional, observational, and nonrandomized study.
A total of 100 patients during a 5-month span with advanced OA undergoing total knee replacement at Max Super Specialty Hospital, Saket, New Delhi, India were included in this study: all of them satisfied the inclusion and exclusion criteria.
Using the prevalence of poor bone health (osteoporosis and osteopenia) as 58.6%, which was reported by Domingues et al, we calculated the sample size as 92 with the following formula:
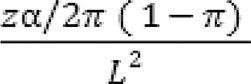
where π is equal to 0.586, and we took L = 0.10 as the margin of error. The confidence level is 95%, which gives zα/2 = 1.96.
Inclusion Criteria
All patients with advanced knee OA undergoing total knee replacement.
Age 50 to 80 years.
Exclusion Criteria
History of treatment for osteoporosis.
Primary hyperparathyroidism.
History suggestive of malabsorption of vitamin D.
Patients taking any medication(s) that could adversely affect bone metabolism.
History of any renal disease contributing impaired hydroxylation of 25(OH) vitamin D to 1,25-dihydroxyvitamin D.
Secondary osteoporosis due to prolonged glucocorticoid intake or significant hepatic or thyroid dysfunction.
After clearance from institutional ethical and scientific committees, we proceeded with the study.
All patients were subjected to dual-energy X-ray absorptiometry (DXA) scan (of both hips and spine). All the values were noted in the form of T-score and World Health Organization guidelines were followed for categorizing as osteoporosis (< −2.5), osteopenia (−1 to −2.5), and normal (> −1). X-rays (both knees–standing anteroposterior and lateral views–and pelvis with both hips–anteroposterior view) were recorded. X-rays interpreted as Lawrence and Kellgren type III were considered as advanced OA. Opinions were taken from two independent radiologists regarding condition of bone at the two different sites (spine and hips). Additionally, serum levels of vitamin D, phosphorus, alkaline phosphatase, and PTH were performed along with other routine preoperative workups. Activity levels of the patient were recorded using the Western Ontario and McMaster Universities osteoarthritis index (WOMAC) scoring system. A detailed social and medical history including features of osteoporosis (h/o fragility fractures), dietary habits, intake of medications and supplements, personal history, and family history (fractures, loss of height, bone pains, etc.) were also recorded.
The DXA machine used was common to all (Hologic DXA system, United States).
Serum vitamin D levels were measured by the chemiluminescence method, serum calcium by the Arsenazo III method, alkaline phosphatase by the 2-amino-2-methylpropanol buffer method, serum phosphorus by phosphomolybdate method, and serum PTH was measured via the intact PTH method.
Reference values considered are shown in ►Table 1.
| S.N. | Parameter | Reference range | ||
|---|---|---|---|---|
| Conventional unit | SI unit | CF | ||
| 1. | Serum vitamin D3 | 30.0–100 ng/mL | 75–250 nmol/L | 2.5 |
| 2. | Serum calcium | 8.8–10.2 mg/dL | 2.19–2.54 mmol/L | 0.2495 |
| 3. | Serum alkaline phosphatase | 32.0–91 IU/L | 0.53–1.52 µkat/L | 0.01667 |
| 4. | Serum phosphorus | 2.3–4.0 mg/dL | 0.74–1.29 mmol/L | 0.3229 |
| 5. | Serum PTH | 12–88 pg/mL | 12–88 ng/L | 1 |
Abbreviations: CF, conversion factor, from conventional unit to SI unit; PTH, parathyroid hormone.
Statistical Analysis
Data were analyzed by correlating the following findings:
Serum levels of vitamin D3.
BMD (T-score) value.
Serum alkaline phosphatase and PTH.
Serum calcium and phosphorus levels.
These correlations compared by Fisher's Z transformation test with values reported in previous literature.
In addition, average T-scores in our patients were compared with previous T-scores by Student's t-test.
The Kruskal – Wallis test and analysis of variance (ANOVA) were also used, wherever applicable.
Results
A total of 100 patients were included in the final result analysis. The following observations and results were found.
87 (87%) were female, and 13 male.
Mean value and observed range for various parameters (►Table 2).
| Parameters (with unit of measure) | Mean value | Range |
|---|---|---|
| Age (y) | 65.35 ± 8.28 | 50–80 |
| Height (cm) | 160.15 ± 7.14 | 147–178 |
| Weight (kg) | 69.37 ± 7.59 | 52–85 |
| Serum vitamin D3 (ng/mL) | 26.91 ± 16.62 | 5–78 |
| Serum PTH (pg/mL) | 48.02 ± 8.68 | 20.3–76.1 |
| Serum calcium (mg/dL) | 9.01 ± 0.46 | 7.9–10.5 |
| Serum phosphate (mg/dL) | 3.40 ± 0 0.45 | 1.9–4.7 |
| Serum alkaline phosphatase (IU/L) | 57.91 ± 9.25 | 42–98 |
| WOMAC score | 56.32 ± 7.81 | 34–76 |
| BMD score (T-scores) for the right hip | −1.68 ± 1.11 | −4.0 to 1.4 |
| BMD score (T-scores) for the left hip | −1.457 ± 1.1 | −4.9–1.8 |
| Overall BMD score (T-score) | −1.16 ± 1.7 | 4.7–1.8 |
Abbreviations: BMD, bone mineral density; PTH, parathyroid hormone; WOMAC, Western Ontario and McMaster Universities osteoarthritis index.
Right Hip
A total of 26 patients had normal bone, 59 had osteopenia, and 15 patients had osteoporosis in the right hip.
Of the 26 patients with normal BMD, 21 were female and 5 were male. This cohort's average age was 61.85 ± 8.64 (range, 51–80 years); average height 160 ± 6.82 (range, 147–174 cm), and mean weight was 71.81 ± 6.78 (range, 59–85 kg). Serum vitamin D3 levels averaged 39.02 ± 19.11 (range, 10–78 ng/mL). The mean serum PTH level was 47.34 ± 6.31 (range, 33.9–58.0 pg/mL), mean serum calcium 9.08 ± 0.53 (range, 7.9–10.5 mg/dL), mean serum phosphorous 3.37 ± 0.53 (range, 1.9–4.7 mg/dL), and the mean value for serum alkaline phosphatase was 58.65 ± 9.43 (range, 42–80 IU/L).
Of the 59 patients diagnosed as osteopenic, 52 were female and 7 male. The average age of this cohort was 65.97 ± 7.76 (range, 50–80 years), mean height 160.03 ± 7.64 (range, 143–178 cm), and mean weight was 69.70 ± 7.47 (range, 52–85 kg). Mean serum vitamin D3 level was 23.20 ± 12.58 (range, 5.0–64.2 ng/mL), mean serum PTH 47.76 ± 9.85 (range, 20.3–76.1 pg/mL), mean serum calcium 9.05 ± 0.43 (range, 8.2–10.3 mg/dL), mean serum phosphorous 3.41 ± 0.44 (range, 2.1–4.7 mg/dL), and average serum alkaline phosphatase level was 58.00 ± 9.39 (range, 45–98 IU/L).
In total, 15 patients presented with osteoporosis, of which 14 patients were female and 1 was male. This cohort's average age was 69.00 ± 7.95 (range, 57–78 years), mean height was 160.16 ± 5.98 (range, 52–74 cm), and mean weight was 63.73 ± 6.96 (range, 52–74 kg). As a group, the average serum vitamin D3 level was 20.48 ± 16.41(range, 5–49.7 ng/mL), mean serum PTH level 50.21 ± 7.31 (range, 34.0–57.1 pg/mL), mean serum calcium level 9.02 ± 0.45 (range, 8.0–10.3 mg/dL), mean serum phosphorous 3.36 ± 0.48 (range, 2.3–4.2 mg/dL), and average serum alkaline phosphatase level was 56.27 ± 9.06 (range, 45–87 IU/L).
For the right hip, we found that age was significantly associated with reduction in T-scores (on DXA scan) (ANOVA test: p-value = 0.018 (<0.05)). We can therefore state that as the age progresses, prevalence of osteoporosis increases.
Similarly, on comparing all three groups (i.e., normal, osteopenia, and osteoporotic groups), the average weight was found to be decreasing (p-value highly significant, p-value = 0.003 (<0.05)). Therefore, we can say that patients with lower weight had more osteopenia and osteoporosis.
The WOMAC scoring in these groups showed the following findings: osteopenic and osteoporotic had higher scores, which reflects the severity of disease in the form of disability. This also was found to be highly significant (with p-values = 0.001 (<0.05)).
Left Hip
A total of 34 patients had normal T-values, 48 had osteopenia, and 18 osteoporosis.
Out of the 34 patients with normal bone, 25 were female and 9 were male. The mean age was 63.03 ± 8.17 (range, 50–80 years), mean height 161.50 ± 7.75 (range, 147–178 cm), and mean weight was 71.82 ± 7.73 (range, 52–85 kg). The mean value for serum vitamin D3 was 34.78 ± 18.98 (range, 10–78 ng/mL), mean PTH 48.35 ± 9.19 (range, 23–76.1 pg/mL), average serum calcium 9.07 ± 0.53 (range, 7.9–10.5 mg/dL), average phosphorus 3.39 ± 0.56 (range, 1.9–4.7 mg/dL), and mean alkaline phosphatase was 57.38 ± 8.23 (range, 42–87 IU/L).
Among the 48 patients with osteopenia, 45 were female and 3 were male. The mean age was 66.48 ± 8.15 (range, 50–80 years), mean height 158.74 ± 7.03 (range, 143–176 cm), and mean weight was 69.34 ± 7.27 (range, 52–82 kg). The mean serum vitamin D3 level was 23.42 ± 13.34 (range, 5–64.2 ng/mL), mean serum PTH 47.54 ± 8.29 (range, 20.4–58.0 pg/mL), mean serum calcium 9.02 ± 0.45 (range, 8.0–10.3 mg/dL), mean serum phosphorus 3.44 ± 0.40 (range, 2.7–4.7 mg/dL), and mean serum alkaline phosphatase was 59.10 ± 10.50 (range, 45–98 IU/L).
A total of 18 patients were diagnosed as osteoporosis, of which 17 were female and 1 was male. The average age for this group was 66.72 ± 7.19, average height 161.39 ± 5.76 (range, 150–170 cm), and average weight was 65.00 ± 6.53 (range, 54–74 kg). The mean value of serum vitamin D3 was 21.34 ± 15.03 (range, 5–49.7 ng/mL), mean serum PTH 48.67 ± 9.13 (range, 20.3–57.1 pg/mL), mean serum calcium 8.89 ± 0.36 (range, 8.2–9.3 mg/dL), mean serum phosphorus 3.27 ± 0.43 (range, 2.4–4.2 mg/dL), and average serum alkaline phosphatase level was 55.73 ± 7.19 (range, 45–98 IU/L).
With increasing age, there should be poor bone health, but our results showed p-value = 0.132 (>0.05), that is, for the left hip, when we took age as a factor, differences among the groups were not significant. The average weight decreased with deterioration of bone health, p-values = 0.009 (<0.05), a highly significant value. Similarly, the WOMAC scores increased with the deterioration of bone health (p-value = 0.000, highly significant).
Spine
A total of 44 patients had a normal BMD, 31 patients showed osteopenia while 25 showed osteoporosis in the spine DXA scans.
Of the 44 patients showing normal DXA values, 35 were female and 9 male. The mean age was 65.2 ± 8.64 (range, 50–80 years), mean height 160.69 ± 7.16 (range, 143–176 cm), and mean weight was 70.44 ± 8.13 (range, 52–85 kg). Mean value for serum vitamin D3 was 26.70 ± 16.33 (range, 5–68 ng/mL), mean serum PTH 48.13 ± 8.38 (range, 23–76.1 pg/mL), mean serum calcium 9.04 ± 0.50 (range, 7.9–10.5 mg/dL), mean serum phosphorus 3.41 ± 0.52 (range, 1.9–4.7 mg/dL), and mean serum alkaline phosphatase level was 58.65 ± 10.13 (range, 45–98 IU/L).
Of the 31 patients with osteopenia, 28 were female and 3 male. These included patients with an average age of 64 ± 8.21 (range, 50–80 years), mean height of 159.16 ± 7.90 (range, 143–178 cm), and mean weight of 69.37 ± 7.22 (range, 52–85 kg). The mean value for serum vitamin D3 was 31.00 ± 16.08 (range, 8.2–10.0 ng/mL), for serum phosphorous 3.36 ± 0.42 (range, 2.6–4.7 mg/dL), for serum PTH 48.67 ± 8.05 (range, 26–78 pg/mL), for serum calcium 8.98 ± 0.46 (range 8.2–10.0 mg/dL), and for serum alkaline phosphatase was 58.16 ± 8.44 (range, 2.6–4.7 IU/L).
In total, 24 (96%) of the 25 patients with osteoporosis were female while 1 (4%) was male. The mean age was 67.20 ± 8.39 (range, 50–80 years), height 160.44 ± 6.25 (range, 147–170 cm), and weight was 67.44 ± 6.99 (range, 54–81 kg). Average values are 22.20 ± 15.03 (range, 5–64.2 ng/mL) for serum vitamin D3, 47.03 ± 10.12 (range, 20.3–57.1 pg/mL) for serum PTH, 8.98 ± 0.41 (range, 8.0–9.6 mg/dL) for calcium, 3.42 ± 0.44 (range, 2.3–4.2 mg/dL) for serum phosphorus, and 56.40 ± 8.74 (range, 42–82 IU/L) for serum alkaline phosphatase. The WOMAC scores averaged 59.68 ± 7.81 (range, 44–76) for this group.
X-Ray Interpretation
Unbiased, independent opinions of two radiologists were taken. Interpretations are presented in ►Table 3.
| DXA scan category | X-ray interpretation by Radiologist I | X-ray interpretation by Radiologist II |
|---|---|---|
| For right hip | ||
| Normal, n = 26 | 25 normal 1 osteoporotic | 25 normal 1 osteoporotic |
| Osteopenia, n = 59 | 23 normal 28 osteopenic 8 osteoporotic | 23 normal 28 osteopenic 8 osteoporotic |
| Osteoporosis, n = 15 | 2 normal 13 osteoporotic | 2 normal 13 osteoporotic |
| For left hip | ||
| Normal, n = 34 | 30 normal 3 osteopenic 1 osteoporotic | 28 normal 5 osteopenic 1 osteoporotic |
| Osteopenia n = 48 | 17 normal 23 osteopenic 8 osteoporotic | 20 normal 21 osteopenic 7 osteoporotic |
| Osteoporosis, n = 18 | 3 normal 2 osteopenic 13 osteoporotic | 2 normal 5 osteopenic 11 osteoporotic |
| For spine | ||
| Normal, n = 44 | 37 normal 7 osteopenic | 39 normal 5 osteopenic |
| Osteopenia, n = 31 | 12 normal 19 osteopenic | 14 normal 17 osteopenic |
| Osteoporosis, n = 25 | 7 osteopenic 18 osteoporotic | 5 normal 20 osteoporotic |
Abbreviation: DXA, dual-energy X-ray absorptiometry.
On comparison, agreement of two radiologists about the condition of bone quality through X-rays is fair (measured by kappa test).
Discussion
This is probably the first study done in India to find out prevalence of poor bone health in an Indian population, and its correlation with the presence of OA. Indian female population is especially at high risk to develop osteoporosis compared with the Western population. Poorer nutrition than the Western population and less physical activity make more prone for development as well as for severity of osteoporosis.
Several community-based studies had presented evidence of an inverse relationship between osteoporosis and OA. There are very few studies done to find out the relationship between advanced OA and osteoporosis. Bergink et al mentioned that patients having advanced OA knee have increased risk of incident vertebral and nonvertebral fractures.17 Pal et al also noted that OA is more prevalent in the female population as compared with their male counterpart.2 Age and early menopause in female are individual risk factors for developing osteoporosis.18 O'Connor also stated that women have more prevalence and severity of OA.19 Looker et al noted similar results in an American population.20 Older age is a significant risk factor for OA.21 These results are in concordance with our study.
Poor nutrition causes dietary deficiency of proteins and hence causes weak bone.22 Calcium intake in elderly is lesser and reduced absorption further lowers effective intake. Vitamin D deficiency is very common in elderlies23 and in the osteoporotic female,24 and is also associated with progression of OA.25 Therefore, vitamin D levels appear to be a contributing factor for both these diseases.
In the present study, 48 (48%) patients had vitamin D3 deficiency and 12 (12%) patients had insufficiency of vitamin D3, while 40 (40%) patients had an adequate level. Ghosh et al26 found normal vitamin D3 value in 45.92% of his patients (comparable to our study), vitamin D3 insufficiency in 29.59% (lower in our study), while vitamin D3 deficiency in 24.49% (higher in our study). Among the control group, 66.66% had normal serum vitamin D3, 13.89% had insufficiency, and 19.44% had deficiency indicating that patients with advanced OA have a higher prevalence of vitamin D deficiency than the normal population.
Breijawi et al27 reported in their study that 84.7% of the patients with OA had serum vitamin D3 levels lower than 30 ng/mL. Jansen and Haddad found 24% prevalence of vitamin D deficiency in elderly patients scheduled for total knee replacement.28 Domingues et al found a very high (84.4%) prevalence of inadequate vitamin D in patients undergoing total hip arthroplasty.29
Ghosh et al26 showed 18.37% of subjects in the study group and 19.44% of subjects in the control group had normal BMD: 32.65% cases and 58.3% controls were osteoporotic; 49.98% cases and 22.22% controls had osteopenia; in total 81.63% of cases and 80.55% of controls had BMDs less than 1 standard deviation below the mean for young healthy adults of the same sex, thus showing a significant correlation of BMD with age.
Chang et al have reported that 57.1% patients had osteopenia, 30.7% patients had osteoporosis, and 47.7% patients had osteopenia in the proximal femur, while 28.9% patients had osteoporosis of the lumbar spine.30 In the study done by Lingard et al, 24% patients had osteopenia and 9% patients had osteoporosis in lumbar spine; 36% patients had osteopenia and 8% had osteoporosis of the index proximal femur; and 31% patients had osteopenia and 6% patients had osteoporosis of the contralateral proximal femur.31
Labuda et al conducted a study to find out the prevalence of osteoporosis in joint arthroplasty patients, and found the prevalence of 26% of osteoporosis in prearthroplasty patients, and not unsurprisingly, higher rates in women.32
Domingues et al similarly found 20.7% prevalence of osteoporosis and 37.9% of osteopenia in patients undergoing total hip arthroplasty.29
We found very high values of WOMAC scores in right, left hip, and spine with osteopenia and osteoporosis in these groups. This indicates that presence of disability has a significant correlation with development of osteoporosis. Lingard et al31 also found high WOMAC scores in patients with OA, which confirmed the presence of severe disease, but they found no significant difference in its prevalence between osteoporotic and nonosteoporotic groups,31 unlike our study. Chang et al30 concluded that poor functional status (determined by WOMAC and SF-36 scores) was related to poorer BMD status.
Conclusion
In our study, we found that patients undergoing total knee replacement for advanced OA had poor bone health, as seen by the high prevalence of vitamin D3 insufficiency (60%), osteopenia, and osteoporosis in the hips (73% for the right, 66% for the left) and spine (56%). Osteopenia and osteoporosis seem prevalent in the Indian population with advanced knee OA.
Limitations
The age range (50–80 years) included in study is younger than that in the Western literature. The sample size of 100 is also less. Most patients belong to urban areas, therefore not the true representation of the target population and the control group was not assigned for the study.
Acknowledgment
We are grateful to Dr. Jitendra Maheshwari and Dr. Rajiv Thukral for their constant support and guidance.
Conflict of Interest
None declared.
Funding
None.
References
- The impact of osteoarthritis in the United States: a population-health perspective: a population-based review of the fourth most common cause of hospitalization in U.S. adults. Orthop Nurs. 2012;31(02):85-91.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of knee osteoarthritis in India and related factors. Indian J Orthop. 2016;50(05):518-522.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105:185-199.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in hip and knee joint replacement: socioeconomic inequalities and projections of need. Ann Rheum Dis. 2004;63(07):825-830.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology and treatment of osteoporosis in women: an Indian perspective. Int J Womens Health. 2015;7:841-850.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for increased bone loss in an elderly population: the Rotterdam Study. Am J Epidemiol. 1998;147(09):871-879.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359(9319):1761-1767.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship between osteoarthritis and osteoporosis in the general population: the Chingford Study. Ann Rheum Dis. 1994;53(03):158-162.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between osteoarthrosis and osteoporosis. An experimental and clinical study. Chir Organi Mov. 1995;80(02):237-243.
- [Google Scholar]
- Baseline bone mineral density and boneturnover in pre-operative hip and knee arthroplasty patients. Bone Joint Res. 2014;3(01):14-19.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoporosis and osteoarthritis–is there really an inverse relation? [in German] Z Orthop Ihre Grenzgeb. 2005;143(02):161-169.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to osteoporosis identification and treatment among primary care physicians and orthopedic surgeons. Mayo Clin Proc. 2002;77(04):334-338.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoporosis management and the utilization of FRAX®: a survey amongst health care professionals of the Asia-Pacific. Arch Osteoporos. 2012;7:193-200.
- [CrossRef] [PubMed] [Google Scholar]
- Painful prosthesis: approaching the patient with persistent pain following total hip and knee arthroplasty. Clin Cases Miner Bone Metab. 2013;10(02):97-110.
- [Google Scholar]
- Hypovitaminosis D in patients scheduled to undergo orthopaedic surgery: a single-center analysis. J Bone Joint Surg Am. 2010;92(13):2300-2304.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D deficiency is associated with progression of knee osteoarthritis. J Nutr. 2014;144(12):2002-2008.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoarthritis of the knee is associated with vertebral and nonvertebral fractures in the elderly: the Rotterdam Study. Arthritis Rheum. 2003;49(05):648-657.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for postmenopausal osteoporosis. Am J Med. 1985;78(01):95-100.
- [CrossRef] [PubMed] [Google Scholar]
- Sex differences in osteoarthritis of the hip and knee. J Am Acad Orthop Surg. 2007;15(01):S22-S25.
- [CrossRef] [Google Scholar]
- Osteoporosis or low bone mass at the femur neck or lumbar spine in older adults: United States, 2005-2008. NCHS Data Brief (93):1-8.
- [Google Scholar]
- Why is osteoarthritis an age-related disease? Best Pract Res Clin Rheumatol. 2010;24(01):15-26.
- [CrossRef] [PubMed] [Google Scholar]
- Dietary protein: an essential nutrient for bone health. J Am Coll Nutr. 2005;24(6)(Suppl):526S-536S.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev. 2001;22(04):477-501.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of vitamin D inadequacy amongst women with osteoporosis: an international epidemiological investigation. J Intern Med. 2006;260(03):245-254. (Erratum in: J Intern Med. 2007 Apr;261(4):408)
- [CrossRef] [PubMed] [Google Scholar]
- Relation of dietary intake and serum levels of vitamin D to progression of osteoarthritis of the knee among participants in the Framingham Study. Ann Intern Med. 1996;125(05):353-359.
- [CrossRef] [PubMed] [Google Scholar]
- A study of the prevalence of osteoporosis and hypovitaminosis D in patients with primary knee osteoarthritis. J Clin Orthop Trauma. 2014;5(04):199-202.
- [CrossRef] [PubMed] [Google Scholar]
- Bone mineral density and vitamin D status in female and male patients with osteoarthritis of the knee or hip. Eur Surg Res. 2009;42(01):1-10.
- [CrossRef] [PubMed] [Google Scholar]
- High prevalence of vitamin D deficiency in elderly patients with advanced osteoarthritis scheduled for total knee replacement associated with poorer preoperative functional state. Ann R Coll Surg Engl. 2013;95(08):569-572.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of osteoporosis in patients awaiting total hip arthroplasty. Acta Ortop Bras. 2015;23(01):34-37.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of osteoporosis in female patients with advanced knee osteoarthritis undergoing total knee arthroplasty. J Korean Med Sci. 2014;29(10):1425-1431.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of osteoporosis in patients with severe hip and knee osteoarthritis awaiting joint arthroplasty. Age Ageing. 2010;39(02):234-239.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of osteoporosis in osteoarthritic patients undergoing total hip or total knee arthroplasty. Arch Phys Med Rehabil. 2008;89(12):2373-2374.
- [CrossRef] [PubMed] [Google Scholar]







