Translate this page into:
Clinical Evaluation and Management of Varicose Veins of Lower Limb at a Tertiary Care Hospital in India

Corresponding author: Dr. Santosh Nayak K, Department of General Surgery, Karwar Institute of Medical Sciences, Karwar, Karnataka, India. santoshnk888@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shrikanth C, Tenginkai P, Nayak SK. Clinical Evaluation and Management of Varicose Veins of Lower Limb at a Tertiary Care Hospital in India. Int J Recent Surg Med Sci. 2024;10:30-34. doi: 10.25259/ IJRSMS_9_2023
Abstract
Objectives
Varicose veins are defined as dilated, tortuous and elongated veins in the lower limbs. Being one of the most common chronic vascular disorders of the lower limb, the varicose veins affect approximately 10% of the population. If left untreated, the patient may end up with complications like ulceration. The present study is aimed at evaluating the demography, risk factors, clinical features and management of varicose vein patients attending the Department of General Surgery at a tertiary care hospital.
Material and Methods
This is a prospective observational study conducted at a tertiary care hospital involving patients with lower limb varicose veins. Demographic factors like age, gender, etiology, clinical features, site of incompetence, type of surgical procedure and postoperative complications were studied.
Results
Out of 74 patients, majority of them (47.2%) were between 41 and 50 years of age, with a predominance of males (51 cases). Analysis of the history of the patients showed that many were chronic alcoholics (72.9%) and chronic smokers (66.2%). Nearly, 91.8% of them presented with visible dilated veins and pain (60.8%) in the affected limb. The long saphenous vein was greatly involved, and majority of them were managed by saphenofemoral flush ligation + subfascial ligation of perforators (SFFL + SFLP) with minimal postoperative complications.
Conclusion
Varicosity of the veins of the lower limb is common in patients with long-standing jobs, chronic alcoholics and smokers. Involvement of the long saphenous vein is observed in majority of the patients. Duplex ultrasound is the most sensitive diagnostic procedure and surgery is the primary modality of the treatment.
Keywords
Varicose veins
Long saphenous vein
Saphenofemoral flush ligation
INTRODUCTION
During 1550 B.C., a scientist named Ebers Papyrus mentioned varicose veins in his book, and Hippocrates described the relation of varicose veins with long standing work. He also mentioned about treatment options like, small punctures in varicose veins and the use of compressive bandages.[1] Chronic peripheral vascular diseases like varicose veins of the lower limbs are very common with an incidence rate of 20–30%.[2]
The exact mechanism of varicose veins is still under debate. According to recent theories, there are many aggravating factors, such as genetic predisposition, thinned out vascular walls, raised intravenous pressure and incompetent valves. The reduced elasticity of the vein wall and the incomplete closure of valve leaflets, leading to valvular dysfunction, is a major cause for the development of varicose veins. In varicose veins, due to valvular dysfunction the blood flows in the reverse direction, i.e. from proximal to distal and deep to superficial. The mechanism of reversed blood flow causes increased pressure on larger veins, creating stress on endothelial cells and inflammation of the veins. Ultimately, due to chronic pressure and inflammation, the larger veins become elongated and tortuous.[3]
The following are the risk factors that are greatly associated with varicose veins.[4]
1) Older patients have thin venous valve. 2) Women are at higher risk due to their hormonal effect on vein wall. 3) Subjects who work in standing position for prolonged hours. 4) Obesity can put extra pressure on veins. 5) Chronic history of alcohol consumption and smoking. 6) History of varicose veins in the family (parents and grandparents). 7) Hormonal changes during puberty, pregnancy, menopause and postmenopausal, and hormone replacement therapy.
The great saphenous vein and the small saphenous vein are the two major superficial veins involved in the venous drainage of the lower limbs, and the same two veins are at higher risk of developing varicosity.[5] Clinically, varicose veins of the lower limbs can be classified into two types: a) Primary varicose veins that develop spontaneously in the absence of deep venous thrombosis; b) Secondary varicose veins that follow an attack of phlebitis. Anatomically, there are three types of varicose veins-trunk varicose veins, reticular varicose veins, and telangiectasia (also called as its starbursts, thread veins, matted veins and spider veins).[6]
The patients with varicose veins in lower extremities present with mild-to-severe symptoms. Initially, the patients present with swelling of the lower limb (ankle oedema), pain in the affected limb, itching and cosmetic issues (skin discoloration). If untreated, they may end up in severe cases like thrombophlebitis, lipodermatosclerosis, spontaneous bleeding of small veins leading to hemorrhage and ulcers.[7,8]
Venous duplex ultrasonography (VDU) is considered to be a standard investigation for the diagnosis of varicose veins since 1990. Recently, the transvaginal venous duplex ultrasound scan (TVDUS) has become the gold standard laboratory test for varicose veins.
Based on the symptoms and severity, the patient can be managed with conservative treatment and surgical or interventional treatment. During the initial days, the patient can be managed conservatively by advising compression stockings, avoidance of prolonged standing, keeping the affected leg in an elevated position and doing lifestyle modifications like weight loss and exercise. However, according to many publications, the best practise is to carry out interventional treatment for a complete cure of varicose veins. Various interventional therapies are also available, such as thermal ablation, external laser thermal ablation, endovenous thermal ablation, endo-venous sclerotherapy and surgical ligation or stripping.[3,9] The present study is aimed at evaluating the demography, risk factors, clinical features and management of varicose vein patients attending the Department of General Surgery at a tertiary care hospital.
MATERIAL AND METHODS
This is a prospective observational study conducted on patients presenting with varicose veins at the Department of General Surgery. The Institutional Ethical clearance was obtained before initiating the study. The Institutional Ethical Committee clearance was obtained before initiating the study approved with the referral number KIMS/ IEC/15/2023. Patients with a history of leg pain, cramps, and further complicated cases like dermatitis, pigmentation, ulceration and superficial thrombophlebitis, and patients with large varicosities who are concerned about cosmetic purposes were included in the study. Patients who can be treated on an Out Patient Department (OPD) basis, with deep vein thrombosis (DVT), secondary veins, pregnancy and peripheral vascular diseases were excluded from the study. All the admitted patients were explained verbally in a regional language about the benefits and risks of the study and written informed consent form was obtained. Apart from clinical evaluation, the diagnosis of the patient was confirmed by duplex ultrasound color Doppler, Perthes clinical test and Trendelenburg multiple tourniquet test. The data was collected in predesigned case study form. Demographic data such as age, sex, occupation and family history was collected.
The following surgical procedures were carried out:
1) Trendelenburg’s operation; 2) subfascial or extra facial ligation of perforators; 3) stripping of the long saphenous vein; 4) multiple stab avulsion of the long saphenous vein; and 5) saphenopopliteal junction ligation. All the patients who underwent surgical management were followed up postoperatively and prognosis of the patients were assessed. Complications, if encountered, were treated accordingly. The descriptive statistics were used to analyze the results.
RESULTS
In the present study, a total of 74 patients with varicose veins who are fulfilling the inclusion criteria were studied. As shown in Figure 1, majority of patients (47.2%) were between 41 and 50 years of age, followed by 24.3% of patients were between 51 and 60 years of age. Out of 74 patients, 51 patients were male and 23 patients were female.

- Age distribution of the patients.
The right lower limb was found to be greatly affected, contributing 59.45% of cases, followed by the left lower limb in 40.5% of cases. Nine patients had bilateral varicose veins. Analysis of the history of the patients showed that varicose veins were greatly seen in chronic alcoholics (72.9%) and chronic smokers (66.2%) [Table 1].
| History of the patients | Number (n = 74) | Percentage (%) |
|---|---|---|
| Prolonged standing occupation | 47 | 63.5 |
| Sedentary activity | 41 | 55.4 |
| Family history | 12 | 16.2 |
| Chronic alcoholism | 54 | 72.9 |
| Chronic smoking | 49 | 66.2 |
n: history of patients with varicose veins.
Figure 2 shows the clinical presentations of patients with lower limb varicose veins.
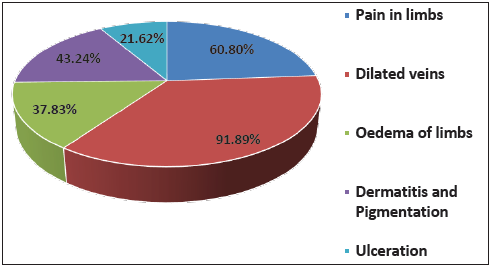
- Percentage of signs symptoms of patients with varicose veins.
Out of 74 patients, the majority (44 cases) showed long saphenous vein involvement. In the present study, the level of incompetence was also assessed after the Doppler study of the limb [Table 2].
| Long saphenous vein | Number (n = 74) | Percentage (%) |
|---|---|---|
| Right side | 21 | 28.3 |
| Left side | 19 | 25.6 |
| Bilateral | 04 | 5.4 |
| Short saphenous vein | ||
| Right side | 14 | 18.9 |
| Left side | 11 | 14.8 |
| Bilateral | 05 | 6.7 |
| Perforator incompetence | ||
| Thigh | 15 | 20.2 |
| Below knee | 29 | 39.1 |
| Above ankle | 25 | 33.7 |
| Unnamed | 05 | 6.7 |
n: number of patients showed long saphenous vein involvement.
All 74 patients were managed with surgical procedures and majority of them (45.9%) were operated on for saphenofemoral flush ligation with stripping of Long Saphenous Vein (LSV) and saphenofemoral flush ligation + subfascial ligation of perforators (SFFL + SFLP). The other types of surgical procedures carried out among the patients are shown in Table 3. Postoperative complications like surgical wound infection were seen in 9 patients, followed by hematoma in 4 patients.
| Procedure done | Number (n = 74) | Percentage (%) |
|---|---|---|
| Saphenofemoral flush ligation (SFFL) | 14 | 18.9 |
| Saphenopopliteal junction ligation (SPJL) | 6 | 8.1 |
| Subfascial ligation of perforators (SFLP) | 4 | 5.4 |
| SFFL + SFLP | 34 | 45.9 |
| SFFL + SPJL | 9 | 12.1 |
| SPJL + SFLP | 7 | 9.4 |
n: number of patients managed with surgical procedures.
DISCUSSION
In the present study, we included 74 patients, out of which 51 were male and 23 were female. In contrast to the previous literature on varicose veins, which have shown that the incidence of varicose veins is more common in females due to their hormones (estrogen and progesterone). However, in a study done by Vijayakumar S et al., findings of gender distribution in varicose veins were in support of the present study (male predominance with 60 cases and females with 40 cases was observed).[10]
In the present study, the majority of patients (47.2%) were between 41 and 50 years of age, followed by 24.3% of patients between 51 and 60 years of age. Similar types of findings were observed in a study carried out by Nitesh et al., where 40% of the patients belonged to the age group of 51–65 years, while 37% of the patients belonged to the age group of 31–50 years.[11] The manifestation of varicose veins in young adults is due to their current lifestyle and aging, which causes more wear and tear on valves.
In the present study, 72.9% of patients were chronic alcoholics, 66.2% of patients were chronic smokers, 63.5% of patients had prolonged standing occupations and 55.4% of patients had a sedentary lifestyle. A positive family history was seen in 16.2% of patients. A study carried out by Shankar KH et al., reveals that 57.14% of the patients were involved in prolonged standing occupations, and 14.28% of the cases had a family history of varicose veins.[12] Prolonged standing or sitting causes the blood to pool in the lower limbs that increases the pressure on the lower limb veins.
The evaluation of signs and symptoms among 74 patients in the current study showed that 68 patients (91.8%) presented with visible dilated veins on the affected limb. In addition, 45 patients (60.8%) had pain in the affected limb, and 32 patients (43.2%) presented dermatitis and pigmentation of the affected limb. Oedema of the affected limb was observed in 28 (37.8%) patients. In a recent study, the patient attending the surgical units of Siddhartha Medical College also presented with similar signs and symptoms. In their study, all (100%) patients presented with prominent veins, pain (86%), oedema (12%), pigmentation (32%) and ulceration (28%).[13]
In the present study, the majority of the patients (44 cases) showed long saphenous vein involvement, followed by short saphenous vein involvement (30 cases). Concerned with vein involvement, our study findings were comparable to many other studies that were conducted recently. The study findings of Rao BN et al., were supportive of the present study, where the long saphenous vein was involved in 52.5% of all cases, the short saphenous in 27.5%, and both in 20% of cases.[14]
As we can see in the results, all 74 patients in the present study underwent surgical procedures. The majority of the patients were operated on by SFFL+SFLP in the present study (45.9%) as well as in a study done by Vikram Ramamurthy et al., (30.7%) [Table 4].[15]
| Present study findings | Study done by Vikram Ramamurthy et al. | ||
|---|---|---|---|
| Saphenofemoral flush ligation (SFFL) | 18.9% | Saphenofemoral flush ligation (SFFL) | 22.7% |
| Saphenopopliteal junction ligation (SPJL) | 8.1% | SFLP | 13.3% |
| Subfascial ligation of perforators (SFLP) | 5.4% | SFFL + Stripping | 17.3% |
| SFFL + SFLP | 45.9% | SFFL + SFLP | 30.7% |
| SFFL + SPJL | 12.1% | Sclerotherapy | 12% |
| SPJL + SFLP | 9.4% | SFFL + SFLP + SPJL + stripping | 4% |
CONCLUSION
From our study, we could reveal that varicose veins are equally common in male patients and young adults in the age group of 41–60 years. Most of the patients were involved in long-standing jobs, chronic alcoholism and smoking. The majority of the patients presented with visible dilated veins and pain on the affected limb, more commonly involving long saphenous vein. We could manage the patients with SFFL + SFLP with minimal postoperative complications.
Acknowledgement
Nil.
Authors contribution
Dr. Shrikant C designed the entire work. Dr. Pradeep Tenginkai and Dr. Santosh Nayak K contribute in making necessary correction and revision of the manuscript. The final draft was checked by all the authors.
Ethical approval
The author(s) declare that they have taken the ethical approval from IEC (KIMS/ IEC/15/2023).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
REFERENCES
- Manipal manual of surgery (2nd ed). New Delhi: CBS; 2005. p. :90-100.
- Efficacy and safety of Buyang Huanwu decoction in the treatment of varicose veins of the lower extremities: A protocol of randomized controlled trial. Medicine. 2021;100:8 (e24663).
- [Google Scholar]
- Prevalence and awareness of varicose veins among teachers in Abha, Saudi Arabia. J Family Med Prim Care. 2020;9:4784-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A brief review on herbs used in the treatment of varicose veins. J Drug Deliv Ther. 2022;12:158-62.
- [Google Scholar]
- A prospective clinical study on varicose veins of lowerlimbs and its management in a tertiary care general surgery department. IOSR J Dent Med Sci (IOSR-JDMS). 2020;19:16-21.
- [Google Scholar]
- Treatment of varicose veins of lowerextremity: A literature review. Int J ClinExp Med. 2019;12:2142-50.
- [Google Scholar]
- Current best practice in the management of varicose veins. Clinical, Clin Cosmet Investig Dermatol. 2022;15:567-83.
- [Google Scholar]
- Clinical study of asymptomatic deep vein thrombosis in patients with varicose veins of lower extremities. JMSCR. 2020;8:117-25.
- [Google Scholar]
- Retrospective study of varicose vein and its management in IGIMS, Patna. Int J Contemp Med Res. 2020;7:G9-G12.
- [Google Scholar]
- A clinical study on surgical management of primary varicose veins. IOSR J Dent Med Sci (IOSR-JDMS). 2018;17:32-6.
- [Google Scholar]
- A clinical study on varicose veins of lower limb, surgical management and functional outcome at a tertiary care hospital of South India. Int Surg J. 2020;7:1051-5.
- [Google Scholar]
- A prospective study on clinical presentation and surgical management of varicose veins at a tertiary care hospital in Bangalore, India. Int J Anat Radiol Surg. 2021;10:SO30-SO33.
- [Google Scholar]







