Translate this page into:
A Comparison of Femoropopliteal Block versus Spinal Anesthesia for Malleolar Surgeries
*Corresponding author: Reshma Sugathan, MBBS, MD, Department of Anaesthesiology and Critical Care, Sree Gokulam Medical College and Research Foundation, Trivandrum, Kerala 695607, India. reshmasug@gmail.com
How to cite this article: Sugathan R, Mathews RM, Venugopalan PG. A Comparison of Femoropopliteal Block Versus Spinal Anesthesia for Malleolar Surgeries. Int J Recent Surg Med Sci. 2024;10:S39-43. doi: 10.1055/s-0043-1761505
Abstract
Objectives
Surgery for malleolar fractures is associated with severe pain. Ultrasonography-guided nerve blocks have quality, precision, and drug dose reduction but are not preferred over spinal anesthesia. We have conducted a study to compare the effectiveness of femoropopliteal block with spinal anesthesia.
The aim of this study was to compare onset, duration, and hemodynamic variability and total analgesic requirement of femoropopliteal block with spinal anesthesia.
Material and Methods
Preoperatively patients were divided into two groups (30 in each): Group 1—patients receiving spinal anesthesia with 0.5% hyperbaric bupivacaine; Group 2—patients receiving 15 mL in popliteal block and 5 mL in femoral block of 20 mL 0.5% bupivacaine with 8 mg dexamethasone. Onset, duration, hemodynamic changes, and postoperative analgesia requirements were monitored.
Results
Mean onset of sensory blockade in group 1 and 2 was 3.83 ± 0.92 and 12.68 ± 3.03 minutes (p-value <0.001.) and motor blockade in group 1 and 2 was 5.36 ± 1.7 and 12.68 ± 3.03 minutes (p-value <0.01), respectively. Mean duration of analgesia in group 1 and 2 was 3 ± 1.31 and 20.2 ± 4.7 hours, respectively. None of the patients in group 2 and 3% in group 1 had hypotension and bradycardia (p-value > 0.05). The mean dose of morphine required in group 1 and 2 was 20.3 ± 2.1 and 3.56 ± 0.02 mg in 24 hours (p-value < 0.001), respectively.
Conclusion
Femoropopliteal block was slower in onset but produced longer postoperative analgesia with markedly reduced opioid consumption.
Keywords
Femoropopliteal Block
Spinal anesthesia
Malleolar surgeries
INTRODUCTION
It has been observed that malleolar fractures are extremely common in the emergency department, with an incidence of 46.7% of tibial/fibular fractures and 7.6% of all fractures.[1] The commonest etiology is slip or fall followed by trauma.[1]
Orthopaedic surgeries are associated with severe pain and effective pain management is essential to prevent the development of chronic pain conditions. Moreover, poorly controlled pain can hinder patients' rehabilitative exercises and delay complete recovery.
Lower limb surgeries are mostly performed under regional anesthesia. The various techniques used are spinal, epidural, and peripheral nerve blocks of which spinal anesthesia is the technique that is widely used. The advantages of spinal anesthesia are faster onset, reliability, quality of block, and a postoperative analgesia for a limited period. With the advent of ultrasonography (USG) in regional anesthesia, nerve blocks have gained popularity owing to the fact that they do not produce hemodynamic compromise and provide comparable operating conditions as spinal anesthesia with the added advantage of extended postoperative analgesia.
A study by Myerson et al. demonstrated superior outcome with regional nerve blocks and concluded that approximately 70% of lower limb surgeries could be done under nerve blocks.[2] The majority of nerve supply to leg is from the branches of sciatic nerve—tibial and common personal nerve—with the exception of sensory supply to medial aspect of calf and ankle from femoral nerve via saphenous branch.
In this study, we have compared the efficacy of USG-guided femoropopliteal block versus spinal anesthesia for malleolar surgeries with regard to onset and quality of block, intraoperative hemodynamic variables, and postoperative analgesia in first 24 hours.
MATERIAL AND METHODS
This observational study was conducted in Sree Gokulam Medical College and Research Foundation from June 2021 to June 2022. The study was conducted after obtaining institutional ethical committee clearance and written informed patient consent in 60 patients (30 in each group). The patients belonged to ages between 25 and 65 years of either sex, American Society of Anaesthesiologists grade I and II, and weighing between 55 and 95 kg.
Patients with spine deformities, known allergy to local anesthetics, pre-existing neurological diseases, coagulopathy, and local site infection were excluded from the study.
Preoperatively patients were divided into two groups.
Group 1—patients receiving spinal anesthesia (n = 30).
Group 2—patients receiving femoropopliteal block (n = 30).
Once patients were shifted to operating room, monitors to record heart rate, noninvasive blood pressure (NIBP), electrocardiogram, and pulse oximetry were connected and baseline parameters recorded.
An intravenous (IV) access was secured using 18 G in cannula and patients started on Ringer's lactate and premedicated with 0.03 mg/kg midazolam.
Group 1 patients were administered spinal anesthesia in lateral decubitus position via midline approach with 0.5% hyperbaric bupivacaine 2.2 mL using 25 G Quincke Babcock needle.
Group 2 patients were administered 20 mL of 0.5% bupivacaine with 8 mg dexamethasone—15 mL in popliteal block and 5 mL in femoral block under USG guidance using 18 G 100 mm Stimuplex needle with patients in prone position and posterior approach was adopted.[3] Under USG guidance, separate injections of tibial nerve and common personal were given. The patient was then shifted to supine and femoral nerve block was administered.
Sensory block was assessed using response to cold. Inability to recognize cold sensation on the surgical limb was considered to be the onset of sensory block. Motor block was assessed by asking patient to dorsiflex foot and inability was considered as onset of motor block. Sensory and motor blocks were evaluated every 2 minutes till achieved.
Intraoperative hemodynamic variables were monitored every 2 minutes: heart rate, NIBP, and oxygen saturation and respiratory rate.
A fall in systolic blood pressure of more than 25% from baseline was hypotension that was treated with 6 mg boluses of mephentermine and fall in heart rate less than 60 was considered bradycardia that was treated with atropine 0.6 mg.
The duration of analgesia was monitored into the postoperative period using Numerical Rating Scale (NRS). Duration of analgesia extended up to a score of 3.
When patients had a pain score more than 3, they were administered injection morphine 0.1 mg/kg IV. The total doses of IV morphine requirement in 24 hours in each group was also assessed.
RESULTS
Data analysis was done using MS Excel and IBM SPSS statistics 22.0 software.
Mean, median, standard deviation, and percentage were used to describe the study variables. Student's t-test and chi-squared test were used for statistical validation. A p-value less than 0.05 was considered to be statistically significant.
The two groups were statistically comparable in terms of demographic data (age, gender, weight; [Table 1]).
Group 1 |
Group 2 |
p-value |
|
|---|---|---|---|
Age (mean ± SD) |
39.60 ± 1.36 |
42.6 ± 1.37 |
0.421 |
Male |
16 (52%) |
18 (60%) |
0.682 |
Female |
14 (48%) |
12 (40%) |
|
Weight (mean ± SD) |
69.54 ± 2.31 kg |
77.87 ± 1.96 kg |
0.358 |
Abbreviation: SD, standard deviation.
Mean onset of sensory blockade in group 1 and 2 was 3.83 ± 0.92 and 12.68 ± 3.03 minutes, respectively. This was statistically significant with a p-value less than 0.001.
Mean onset of motor blockade in group 1 and 2 was 5.36 ± 1.7 and 12.68 ± 3.03 minutes, respectively, with p-value less than 0.01. This was statistically significant [Figure 1].
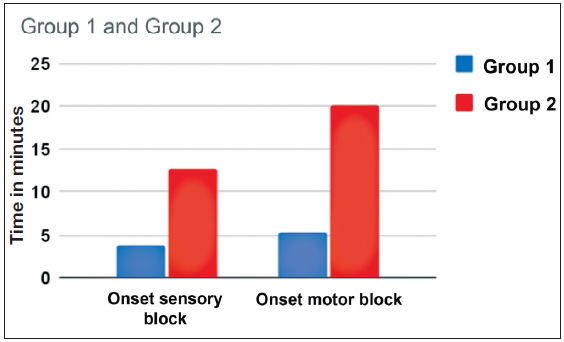
- Comparison of onset of sensory and motor block between groups 1 and 2.
Mean duration of analgesia in group 1 and 2 was 3 ± 1.31 and 20.2 ± 4.7 hours, respectively. This was found to be statistically significant with a p-value less than 0.001 [Table 2; Figure 2].
Group 1 |
Group 2 |
p-value |
|
|---|---|---|---|
Onset sensory block (mean ± SD) min |
3.83 ± 0.92 min |
12.68 ± 3.03 min |
<0.001 |
Onset motor block (mean ± SD) min |
5.36 ± 1.7 min |
16.2 ± 4.7 min |
<0.001 |
Duration of analgesia (mean ± SD) h |
3 ± 1.31h |
14.4 ± 1.91h |
<0.001 |
Total morphine dose 24hours (mean ± SD) mg |
20.3 ± 2.1 mg |
3.56 ± 0.02 mg |
<0.001 |
Abbreviation: SD, standard deviation.
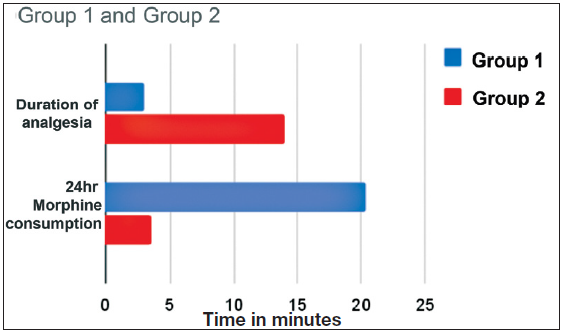
- Comparison of duration of analgesia and its requirement between groups 1 and 2.
Regarding hemodynamic variables, none of the patients in group 2 had hypotension and bradycardia with incidence 0%. Three percent of patients developed hypotension in group 1, but there was no statistically significant difference between the two groups (p-value >0.05). None of the patients in both groups developed bradycardia or fall in oxygen saturation (<90%; [Table 3]).
SBP fall by 25% |
Group 1 |
Group 2 |
p-value |
|---|---|---|---|
Yes |
6 (20%) |
0 (0%) |
0.15 |
No |
24 (80%) |
30 (100%) |
Abbreviation: SBP, systolic blood pressure.
The mean total dose of morphine required in group 1 and 2 was 20.3 ± 2.1 and 3.56 ± 0.02 mg in 24 hours that was statistically significant (p-value < 0.001; [Figure 2]).
DISCUSSION
Malleolar fractures are very commonly encountered in our routine practice and the commonly administered anesthesia is spinal anesthesia. Once the spinal anesthesia has worn off, we usually depend on nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids that are not without adverse effects. NSAIDs can increase perioperative bleeding and precipitate renal failure especially in a hypovolemic trauma patient. Opioids can cause constipation, urinary retention, respiratory depression along with possibility of dependence and addiction and hyperalgesia.[4] Thus, we arrive at a point where we need to devise newer techniques and drugs for the control of pain. Peripheral nerve blocks have always been used either as sole anesthetic technique or along with general anesthesia. The drawback of blocks has been sensory sparing and potential for local anesthetics toxicity. The advent of USG in regional nerve blocks has markedly increased success rate and made local anesthetic dose reduction possible by 60 to 65%, thereby reducing risk of systemic toxicity.[5] USG reduces block performance time, reduces needle pass numbers, and shortens time of onset of block.[6]
Out of the 30 patients in group 2 who received femoropopliteal block, three patients had sensory sparing and had to be converted to general anesthesia. One patient in group 1 had a failed spinal anesthesia that required conversion to general anesthesia. Our study showed a mean onset of sensory block of 12.68 ± 3.03 minutes in group 2, when group 1 had an onset time of 3.83 ± 0.92 minutes. This difference was statistically significant (p < 0.001). We obtained a statistically significant faster onset of motor block in group 1 (5.36 ± 1.7 vs. 16.2 ± 4.7 minutes). This may be due to delay in local anesthetic to be absorbed into a thick sciatic nerve. A study by Taboada et al. showed fastest onset of block of around 16 ± 4 minutes for posterior approach of sciatic nerve.[7] This is comparable to the findings in our study.
The mean duration of analgesia was significantly higher in group 2 (14.4 ± 1.91 hours) when compared with group 1 (3 ± 1.31 hours). This was consistent with a study by Karaarslan et al. They reported longer analgesic duration, delayed rescue analgesic requirement, and better pain satisfaction scores in the popliteal group.[8]
Jeon et al. in 2013 conducted a study comparing spinal anesthesia with popliteal sciatic nerve block in hallux valgus surgeries. They concluded that the time of onset of block to be longer in popliteal nerve block group but provided excellent postoperative analgesia and better patient satisfaction.[9] The addition of 8 mg dexamethasone could have contributed to the extended duration of analgesia. In a study by Cummings et al., analgesia up to 22 hours was obtained with addition of 8 mg dexamethasone to ropivacaine or bupivacaine in supraclavicular block.[10] The patients were administered morphine (0.1 mg/kg) once their NRS pain score was more than 3. Group 1 patients required significantly higher 24-hour morphine doses (20.3 ± 2.1 mg) when compared with group 2 patients who only required a mean dose of 3.56 ± 0.02 mg. This is comparable to the conclusion drawn by Jeon et al.[9]
Protic et al. studied the efficiency of USG-guided femoropopliteal block for ankle surgeries; they also evaluated the duration of analgesia and compared it with analgesia of spinal anesthesia.[11] They found both forms of anesthesia to be equally effective in terms of quality. Duration of postoperative analgesia was significantly higher in femoropopliteal group. But onset of sensory and motor block was faster in spinal anesthesia group.[11]
Arjun et al. evaluated effectiveness of USG-guided popliteal sciatic and abductor canal block for below knee surgeries in high-risk patients in which they were able to successfully perform surgery in all patients without any added analgesic requirement. The nerve block also did not reduce hemodynamic variations in any patients.[12,13] We obtained similar results in our study where none of the patients developed any hemodynamic fluctuations, while 3% patients in group 1 developed a fall in systolic blood pressure more than 20%. This difference was found to be not significant statistically that could be due to the small sample size.
The overall morphine consumption was reduced in group 2 (3.56 ± 0.02 mg) as compared with group 1 (20.3 ± 2.1mg). Hence, nerve blocks also provide the added advantage of reducing opioid use perioperatively.[14]
CONCLUSION
We come to the inference that a femoropopliteal block is a safe and effective sole anesthetic technique for malleolar surgeries especially in patients with underlying cardiac conditions in whom avoidance of the hemodynamic fluctuations of spinal anesthesia is desirable. The stable hemodynamics is also reported to be related to improved survival. Moreover, this technique also provides extended postoperative analgesia, thereby avoiding opioids and NSAIDs in the postoperative period. The only drawback we could find is the slower onset of block when compared with spinal anesthesia but which could easily be negated with the above-mentioned advantages.
Hence, we advocate USG-guided nerve block to be an effective anesthetic technique that provides excellent operating conditions, stable hemodynamics and long postoperative analgesia.
Conflicts of interest
None declared.
References
- Fractures of the Tibia and Fibula Clinical epidemiology of orthopedic trauma (2nd ed) Ch. 5, 287–90
- [Google Scholar]
- Regional Anesthesia for Foot and Ankle Surgery. Foot Ankle. 1992;13:282-8.
- [CrossRef] [PubMed] [Google Scholar]
- The Benefits of Opioid Free Anaesthesia and the Precautions Needed While Employing It. Transl Perioper Pain Med. 2020;7:152-7.
- [PubMed] [PubMed Central] [Google Scholar]
- Local Anesthetic Systemic Toxicity: Current Perspectives. Local Reg Anesth. 2018;11:35-44.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Ultrasound-Guided Peripheral Nerve Blocks: What are the Benefits? Acta Anaesthesiol Scand. 2008;52:727-37.
- [CrossRef] [PubMed] [Google Scholar]
- The Effects of Three Different Approaches on the Onset Time of Sciatic Nerve Blocks with 0.75% Ropivacaine. Anesth Analg. 2004;98:242-7.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison Between Ultrasonography-Guided Popliteal Sciatic Nerve Block and Spinal Anaesthesia for Hallux Vagus Repair. Foot Ankle Int. 2016;37:85-9.
- [CrossRef] [PubMed] [Google Scholar]
- Popliteal Sciatic Nerve Block Versus Spinal Anesthesia in Hallux Valgus Surgery. Korean J Anesthesiol. 2013;64:321-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effect of Dexamethasone on the Duration of Interscalene Nerve Blocks with Ropivacaine or Bupivacaine. Br J Anaesth. 2011;107:446-53.
- [CrossRef] [PubMed] [Google Scholar]
- Benefit of the Minimal Invasive Ultrasound Guided Single Shot Femoropopliteal Block for Ankle Surgery in Comparison with Spinal Anaesthesia. Wien Klin Wochenschr. 2010;122:584-7.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound-Guided Popliteal Sciatic and Adductor Canal Block for Below-Knee Surgeries in High-Risk Patients. Indian J Anaesth. 2019;63:635-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Peripheral Nerve Blocks for Lower Limb Surgery--a Choice Anaesthetic Technique for Patients with a Recent Myocardial Infarction? Singapore Med J. 2002;43:583-6.
- [PubMed] [Google Scholar]








