Translate this page into:
An Observational Analysis of Mesh Fixation with Minimum Sutures and Its Postoperative Outcomes
*Corresponding author: Abhay Saini, MBBS, MS(General Surgery), Department of General Surgery, LN Medical College, Bhopal, Madhya Pradesh, India. sainiabhay69@gmail.com
How to cite this article: Saini A, Mishra N, Kushwah P, Toseef M, Huda T. An Observational Analysis of Mesh Fixation with Minimum Sutures and Its Postoperative Outcomes. Int J Recent Surg Med Sci. 2024;10:S62-6. doi: 10.1055/s-0043-1761617
Abstract
Objectives
The history of hernia repair is the history of the surgery itself. The surgical management of inguinal hernia has continuously evolved for 200 years.
This article determines the incidence of recurrence, chronic pain, and complications following open, tension-free Lichtenstein hernioplasty using a minimal stitch approach.
Material and Methods
This was a single-center, hospital-based, prospective observational study. A total of 197 participants with uncomplicated hernias were enrolled. All participants were operated following open, tension-free, minimal stitch Lichtenstein hernioplasty. The duration of follow-up was 6 months.
Results
Thirty-one (15.7%) participants were lost to follow-up, and 154 (78.2%) participants completed the follow-up. Making total of 166 cases (of which 142 were unilateral and 12 were bilateral, counted as 24 individually). Overall, right-sided direct inguinal hernia (30%) was the most common type, followed by right-sided indirect hernia (26%). Most participants (85%) were given three sutures to fix the mesh during open tension-free hernioplasty. The incidence of postoperative complications, including wound infection, hematoma, and seroma, was zero among participants in each group. The incidence of chronic pain and recurrence at 3 and 6 months after the surgery was zero among all participants.
Conclusion
Most patients in this study required three stitches to fix the mesh during hernioplasty. There were zero incidences of chronic pain, recurrence of the hernia, or any postoperative complication among participants. Thus, hernioplasty can be safely and effectively performed with minimal sutures among male patients with either unilateral or bilateral uncomplicated hernia.
Keywords
Inguinal hernia repair
Mesh fixation
Minimum sutures
INTRODUCTION
Hernia in Greek stands for a “bud or offshoot” and is defined as “abnormal protrusion of whole or a part of a viscus through the wall that contains it.”[1] The history of the modern approach to hernia repair is approximately 150 years old. In December 1889, Dr. Edoardo Bassini repaired the posterior wall of the inguinal canal as a part of the surgery and claimed less recurrence.[2] His novel technique remained the gold standard for inguinal hernia repair for the next 80 years. It had some disadvantages like long recovery time, prolonged pain due to suture line tension, and discomfort in day-to-day activities.[3-6] This led to the next step in the evolution of hernia repair, that is, the era of tension-free hernia repair.
In 1984, Lichtenstein proposed his novel approach for tension-free hernioplasty.[7,8] At present, the two most widespread methods for hernia repair are open Lichtenstein repair and laparoscopic hernia repair.[9] In the standard technique, 8 to 10 stitches with interrupted nonabsorbable sutures (mostly Prolene) are typically required to fix the mesh. One recent addition to the list of techniques was proposed by Patchayappan et al in the year 2015 for the repair of uncomplicated hernia.[10] Therefore, this study was conducted to analyze the postoperative outcomes of minimal sutures applied for fixing the mesh during open tension-free hernioplasty.
MATERIAL AND METHODS
The study was conducted at the Department of General Surgery at Laxmi Narayan Medical College and Research Centre and affiliated J.K. Hospital, Bhopal, Madhya Pradesh, India. The total duration of the study: 18 months, from December 2019 to May 2021.
Criteria for inclusion
-
Patients undergoing elective inguinal hernia repair.
-
Patients aged between 18 and 80 years (both inclusive).
Criteria for exclusion
-
Patients diagnosed with a recurrence of hernia.
-
Patients with strangulated or obstructed hernia
Data collection
The data relating to demographic details, clinical history and examination, laboratory and radiological investigations, surgical procedure, intraoperative complications, and events in the postoperative period were collected.
Procedure
Participants enrolled in the study were operated on following the “minimum stitch hernioplasty” procedure under spinal anesthesia. Criteria for deciding the number of stitches are described in [Table 1].
Criteria for determining the number of stitches/sutures |
|
|---|---|
Indirect hernia and age < 30 y |
2 |
Indirect hernia and age ≥ 30 y |
3 |
Direct hernia and defect size < 2 cm |
3 |
Direct hernia and defect size ≥ 2 cm |
4 |
Prolene mesh fashioned as in Lichtenstein’s repair, fixed only by Prolene suture at the following landmarks [Figure 1]:
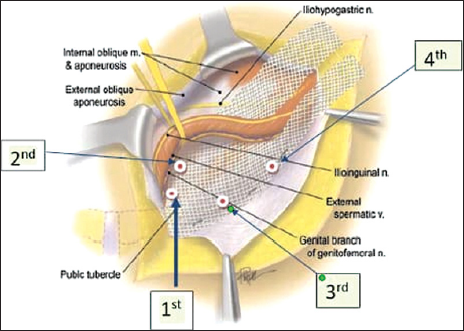
- Points of fixation of mesh.
1st stitch – Pubic tubercle.
2nd stich – Conjoint tendon (2 cm superolateral to 1st suture).
3rd stich – Inguinal ligament (2 cm inferolateral to 1st suture) (if required).
4th stich – 2 cm lateral to third suture (if required).
Intraoperative period
Time taken for the hernioplasty (incision to suturing) was noted.
Postdischarge follow-up
All participants were called for follow-up visits on postoperative day 1, 3, and 10. Further, participants were followed up at 1, 3, and 6 months following the discharge from the hospital.
Duration of follow-up
All participants were followed up 6 months after the surgery.
RESULTS
During the data collection period, we approached 228 patients: 22 were excluded, and 9 patients refused to participate. A total of 197 participants were enrolled in the present study: 31 participants were lost to follow-up or came later than 6 months after hernioplasty, and the remaining 154 participants completed the study. Making total of 166 cases (of which 142 were unilateral and 12 were bilateral, counted as 24 individually).[11]
In the present study, most participants (85%) were given three sutures to fix the mesh during open tension-free hernioplasty [Table 2]. The mean age of the participants who required two, three, and four stitches during hernioplasty was 29.2, 55.4, and 77.9 years, respectively. Overall, the proportion of participants with bilateral, right, and left side inguinal hernia were approximately 15, 57, and 29%, respectively. About 58% of participants had a direct hernia, and the rest, 42% of participants, had an indirect hernia. Overall, right-sided direct inguinal hernia (30%) was the most common type among the enrolled participants, followed by right-sided indirect hernia (26%). The bilateral indirect inguinal hernia was the least common type among study participants.
Number of stitches |
n |
% |
|---|---|---|
2 |
12 |
7.23 |
3 |
142 |
85.54 |
4 |
12 |
7.23 |
Total |
166 |
100.00 |
Table 3 shows the distribution of the total time taken to complete the surgery and the type of hernia. In the present study, the mean and the median duration of hernioplasty among the participants were 56 and 52 minutes, respectively. The mean duration of hernioplasty among the participants who required two, three, and four stitches were comparable without any statistically significant difference between the groups. Among the participants diagnosed with a direct and indirect hernia, the mean time taken to complete the hernioplasty was 66 and 80 minutes, respectively. Among the participants diagnosed with a direct and indirect hernia, the median time to complete the hernioplasty was 60 and 70 minutes, respectively. Among the study participants the shortest duration of postoperative stay was 3 days, and the most extended duration of stay was 5 days. Additionally, most of the participants (85%) stayed in the hospital for 4 days or less. The mean duration of hospital stays among the participants who were given two, three, and four stitches during hernioplasty was 3.5, 3.9, and 4.4 days.
Time (min) |
Type |
||
|---|---|---|---|
Direct (n, %) |
Indirect (n, %) |
Total (n, %) |
|
< 30 |
1 |
0 |
1 |
1.18 |
0.00 |
0.60 |
|
31–45 |
26 |
1 |
27 |
30.59 |
1.23 |
16.27 |
|
46–60 |
17 |
4 |
21 |
20.00 |
4.94 |
12.65 |
|
15 |
45 |
60 |
|
17.65 |
55.56 |
36.14 |
|
76–90 |
8 |
2 |
10 |
9.41 |
2.47 |
6.02 |
|
> 90 |
18 |
29 |
47 |
21.18 |
35.80 |
28.31 |
|
Total |
85 |
81 |
166 |
Mean (SD) |
66.4 (24.53) |
80.9 (17.73) |
73.5 (22.6) |
Median |
60 |
70 |
71 |
Range |
30–120 |
45–110 |
30–120 |
Abbreviation: SD, standard deviation.
On the third postoperative day, the median pain score was highest among the participants who required four stitches to fix the mesh, and it was the minimum among the participants who required only two stitches [Table 4]. The percentage of participants who felt no pain (visual analog scale [VAS] score = 0) on the third postoperative day among those who required two, three, and four stitches was 33, 21, and 8%, respectively. On the 10th postoperative day, more than 90% of participants did not complain of pain at the surgery site. The percentage of participants who felt no pain (VAS score = 0) on the 10th postoperative day among those who required two, three, and four stitches was 100, 95, and 66%. Only 2 and 16% of participants who required three and four stitches complained of pain equivalent to a VAS score of 2. About 1 month after the hernioplasty, none of the participants felt any pain at the surgery site. VAS score among participants in each of the three study groups was zero.
Pain score (VAS) |
Number of sutures |
Total |
||
|---|---|---|---|---|
Two (n, %) |
Three (n, %) |
Four (n, %) |
(n, %) |
|
0 |
4 |
30 |
1 |
35 |
33.33 |
21.13 |
8.33 |
21.08 |
|
1 |
0 |
8 |
0 |
8 |
0.00 |
5.63 |
0.00 |
4.82 |
|
2 |
4 |
30 |
0 |
34 |
33.33 |
21.13 |
0.00 |
20.48 |
|
3 |
3 |
42 |
4 |
49 |
25.00 |
29.58 |
33.33 |
29.52 |
|
4 |
1 |
26 |
5 |
32 |
8.33 |
18.31 |
41.67 |
19.28 |
|
5 |
0 |
6 |
2 |
8 |
0.00 |
4.23 |
16.67 |
4.82 |
|
Total |
12 |
142 |
12 |
166 |
Median |
2 |
3 |
4 |
|
Abbreviation: VAS, visual analog scale.
Chronic pain
About 3 months after the hernioplasty, none of the participants felt any pain at the surgery site. Moreover, no localized tenderness was detected in any participant on local examination at the surgery site. In the present study, the maximum follow-up duration was 6 months. On the last follow-up visit, that is, 6 months after the surgery, none of the participants complained of any type of pain (intermittent or persisting). Moreover, no tenderness was detected in any participant on local examination at the surgery site.
Postoperative complication
In the present study, postoperative wound infection was not seen in any patient. None of the participants in the two-, three-, or four-stitch group had postoperative wound infection. Moreover, no redness or swelling was detected in any participant on local examination of the surgery site. None of the participants in the two-, three-, or four-stitch group had seroma and hematoma during the postoperative period. Moreover, no abnormality was detected in any participant on local examination of the surgery site.
On the last follow-up visit, that is, 6 months after the surgery, none of the participants had a recurrence of hernia at or around the site of surgery. The incidence of hernia recurrence was zero in each of the three study groups.
DISCUSSION
The history of hernia and its repair is more than two millenniums old. Thus, it is hardly surprising that great surgeons of each generation have made some contributions to the science of hernia repair. Therefore, at present, there are several approaches to repairing a hernia. Further, each of these techniques had numerous variations and adaptations. Each technique is marketed as a revolution in the field of hernia repair. All these techniques have their merits and drawbacks.
Moreover, variation not only exists for the technique of hernia repair but also the materials, viz., suture, adhesives, glue, etc., used during hernia repair. We evaluated the technique first proposed by Patchayappan et al to repair an uncomplicated hernia.[10] In the present study, we compared the postoperative and late outcomes of hernioplasty using this approach. In the standard technique, 8 to 10 stitches with interrupted nonabsorbable sutures (mostly Prolene) are usually required to fix the mesh.[9] In the present study, a minimum of two to a maximum of four stitches with interrupted nonabsorbable sutures were given. Further, most patients in the present study required only three stitches to fix the mesh.
In the present study, the mean and the median duration of hernioplasty among the participants were 56 and 52 minutes, respectively. The mean duration of hernioplasty among the participants who required two, three, and four stitches were comparable without any statistically significant difference between the groups. Patchayappan et al performed hernioplasty using the novel three-stitch technique (three interrupted nonabsorbable sutures) on 100 patients with uncomplicated hernias. They reported that the mean duration of surgery was 95 minutes.[10] Jain and Vindal reported that among 40 participants who underwent convectional tension-free open hernioplasty, the mean duration of surgery was 34 minutes.[12] Bracale et al reported that among 52 participants who underwent convectional tension-free open hernioplasty, the mean duration of surgery was 35 minutes.[13] Negro et al reported that among 171 participants who underwent convectional tension-free open hernioplasty, the mean duration of surgery was 61 minutes.[14] Hoyuela et al reported that out of 182 participants who were operated on following open tension-free hernioplasty with sutures, the mean duration of surgery was 40 minutes.[15] Shen et al reported that out of 55 participants who were operated on following open tension-free hernioplasty with sutures, the mean duration of surgery was 43 minutes.[16]
In the present study, a total of 166 participants—142 with a unilateral hernia and 24 with a bilateral hernia—were followed up for 6 months to detect any chronic pain among the participants. In the present study, none of the participants in any of the suture groups, viz., two, three, and four, complained of pain 6 months after the surgery. Patchayappan et al performed hernioplasty using the novel three-stitch technique (three interrupted nonabsorbable sutures); during the 24 months of follow-up, the author observed that only 2% of participants complained of chronic pain at the operative site.[10] Shen et al reported that approximately 10% of participants reported chronic pain after the standard tension-free open hernioplasty.[16] Lichtenstein, in his original report based on observations on 1,000 patients treated for hernia, reported that only 1.5% of participants reported chronic pain.[7] Redha et al followed 158 participants for a total of 12 months. They reported that 9.8% of participants reported having chronic pain at the operative site.[17] Jain and Vindal followed a total of 401 patients for 12 months. They reported that approximately 12.5% of all patients complained of chronic pain during follow-up.[12]
In the present study, the total follow-up duration was 6 months. None of the participants in any of the suture groups, viz., two, three, and four, had any hernia recurrence 6 months after the surgery. Patchayappan et al followed participants for a total duration of 24 months. They reported a recurrence rate of only 1% from their novel technique.[10] Lichtenstein followed the participants for a total duration of 60 months. He did not observe any recurrence even in a single patient.[7]
Similarly, Bracale et al followed 52 participants for 12 months.[13] Like our findings, they did not observe any recurrence among their participants. Also, Matikainen et al followed 151 participants for 84 months.[18] They observed the recurrence of hernia only among 1.25% of the participants. Redha et al followed 158 participants for 12 months.[17] Like our findings, they did not observe any recurrence among their participants. However, Eker et al followed 103 participants for 35 months. They reported a recurrence rate of 14% among their participants.[19]
CONCLUSION
In the present study a total of 166 cases, 142 with unilateral and 24 with bilateral inguinal hernia, were operated using the open, tension-free hernioplasty based on Lichtenstein’s technique using minimal suture approach. Most patients in this study required three stitches to fix the mesh during hernioplasty. There was zero incidence of chronic pain, recurrence of hernia, or any postoperative complication among participants.
Thus, hernioplasty can be safely and effectively performed with minimal sutures and this technique can be adopted by surgeons for the repair of either unilateral or bilateral uncomplicated hernia.
Funding
None.
Conflicts of interest
None declared.
References
- General Introduction and History of Hernia Surgery. Management of Abdominal Hernias. 5th ed. [Internet]. April 16, 2018;3–30. Accessed February 3, 2022, at: https://link.springer.com/chapter/10.1007/978-3-319-63251-3_1
- [Google Scholar]
- Milestones in the History of Hernia Surgery: Prosthetic Repair. Hernia. 2004;8:8-14.
- [CrossRef] [PubMed] [Google Scholar]
- Shouldice Technique Versus Other Open Techniques for Inguinal Hernia Repair. Cochrane Database Syst Rev. 2012;2012:CD001543.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Randomized Trial of Modified Bassini Versus Shouldice Inguinal Hernia Repair. Br J Surg. 1994;81:1531-4.
- [CrossRef] [PubMed] [Google Scholar]
- Randomized Clinical Trial Comparing 5-year Recurrence Rate After Laparoscopic Versus Shouldice Repair of Primary Inguinal Hernia. Br J Surg. 2005;92:1085-91.
- [CrossRef] [PubMed] [Google Scholar]
- Crucial Steps in the Evolution of the Preperitoneal Approaches to the Groin: An Historical Review. Hernia. 2011;15:1-5.
- [CrossRef] [PubMed] [Google Scholar]
- Herniorrhaphy. A Personal Experience with 6,321 Cases. Am J Surg. 1987;153:553-9.
- [CrossRef] [PubMed] [Google Scholar]
- International Guidelines for Groin Hernia Management. Hernia. 2018;22:1-165.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Three Stitch Hernioplasty: A Novel Technique for Beginners. Avicenna J Med. 2021;5:106-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- How to Calculate Sample Size for Different Study Designs in Medical Research? Indian J Psychol Med. 2013;35:121-6.
- [CrossRef] [PubMed] [Google Scholar]
- Gelatin-Resorcin-Formalin (GRF) Tissue Glue as a Novel Technique for Fixing Prosthetic Mesh in Open Hernia Repair. Hernia. 2009;13:299-304.
- [CrossRef] [PubMed] [Google Scholar]
- Beneficial Effects of Fibrin Glue (Quixil) Versus Lichtenstein Conventional Technique in Inguinal Hernia Repair: A Randomized Clinical Trial. Hernia. 2014;18:185-92.
- [CrossRef] [PubMed] [Google Scholar]
- Open Tension-Free Lichtenstein Repair of Inguinal Hernia: Use of Fibrin Glue Versus Sutures for Mesh Fixation. Hernia. 2011;15:7-14.
- [CrossRef] [PubMed] [Google Scholar]
- Randomized Clinical Trial of Mesh Fixation with Glue or Sutures for Lichtenstein Hernia Repair. Br J Surg. 2017;104:688-94.
- [CrossRef] [PubMed] [Google Scholar]
- NBCA Medical Adhesive Suture for Patch Fixation in Lichtenstein Inguinal Herniorrhaphy: A Randomised Controlled Trial. Surgery. 2012;151:550-55.
- [CrossRef] [PubMed] [Google Scholar]
- The Difference in Outcome of Patients with Open Inguinal Hernia Repair by Using Delayed Absorbable Sutures Instead of Non-Absorbable Sutures for Mesh Fixation. Int Surg J. 2021;8:24-7.
- [Google Scholar]
- Randomized Clinical Trial Comparing Cyanoacrylate Glue Versus Suture Fixation in Lichtenstein Hernia Repair: 7-year Outcome Analysis. World J Surg. 2017;41:108-13.
- [CrossRef] [PubMed] [Google Scholar]
- Randomized Clinical Trial of Total Extraperitoneal Inguinal Hernioplasty vs Lichtenstein Repair: A Long-Term Follow-Up Study. Arch Surg. 2012;147:256-60.
- [CrossRef] [PubMed] [Google Scholar]








