Translate this page into:
Antimicrobial Prescription Pattern in ENT Outpatient Department in a Tertiary Care Teaching Hospital, Telangana, India
*Corresponding author: Uma Pokala, MS (ENT), Department of ENT, Mamata General Hospital, Khammam, Telangana, India. umapokala221@gmail.com
How to cite this article: Aalasyam N, Potnuru S, Sileveru CM, Pokala U, Naveen P. Antimicrobial Prescription Pattern in ENT Outpatient Department in a Tertiary Care Teaching Hospital, Telangana, India. Int J Recent Surg Med Sci. 2024;10:S28-34. doi: 10.1055/s-0043-1761502
Abstract
Objectives
Otorhinolaryngological infections are very common in adults and in children also. These infections are caused by various microorganisms and to treat these infections, antimicrobial agents are used frequently. As irrational use of antimicrobials leads to the development of antibiotic resistance and it is a big threat to the society, the present study was planned to get awareness among the practitioners regarding the antimicrobial prescription pattern.
To study the prescription pattern of antimicrobial agents in outpatient department of otorhinolaryngology in a tertiary care teaching hospital.
Material and Methods
An observational study was planned over a period of 8 months from July 2019 to February 2020 in ENT outpatient department (OPD) at Mamata General Hospital, Khammam in Telangana. In total, 562 prescriptions were collected. Patient's details, probable diagnosis, prescribed medication details such as generic name, dose, and dosage forms were taken. The collected data was analyzed and the conclusions were drawn using descriptive analysis.
Results
Total number of prescriptions were 562. The majority of the prescriptions belonged to the 21 to 40 years of age group. Males were included more than females (males 320 and females 242). Chronic suppurative otitis media (CSOM) (16.2%) was the commonest infection. Most commonly prescribed antimicrobial was amoxicillin and clavulanic acid combination (26.17%), followed by cefpodoxime with clavulanic acid (21.9%) and ciprofloxacin (19.06%). In 371 (66.01%) prescriptions, only one antimicrobial was prescribed, whereas in 36 (6.40%) prescriptions no antibiotic was given. The average number of drugs per prescription was 3.18 and the average number of antimicrobials per prescription was 1.25. Tablet form (52.9%) was the commonest dosage form and most of the drugs were prescribed by generic name (74.06%).
Conclusion
The present study though prescription pattern of antibiotics and adherence to the hospital formulary by the physicians in the hospital is encouraging, still there is a chance in reducing the number of drugs prescribed per patient. The findings of this study will be useful to prescribe antimicrobials rationally so that the patient and health care system on the whole will be benefited.
Keywords
antibiotic resistance
antimicrobial usage
CSOM
polypharmacy
INTRODUCTION
Diseases of ENT are common in general population. ENT diseases affect all age groups ranging from children to adults with significant disability-adjusted life-year (DALY) of patient.[1] Most common ENT infections that can be managed with medications are acute rhinitis, sinusitis, adenoiditis, tonsillitis, pharyngitis, acute and chronic suppurative otitis media (CSOM), otitis externa, laryngitis and epiglottitis. If these conditions are not treated properly some serious consequences can occur like stridor, hoarseness of voice, permanent hearing problems and emotional disturbances which lowers the patient's quality of life.[2]
Upper respiratory tract infections (URTI)s such as tonsillitis, pharyngitis, nasopharyngitis, and otitis media contribute to 20 to 40% of infections among patients who are attending outpatient departments (OPD).[3] For some ENT and respiratory infections such as rhinopharyngitis and acute bronchitis, though the etiology is viral antibiotics were prescribed commonly.
Antimicrobial prescription pattern differs from place to place, depending on the antimicrobial susceptibility, infecting organisms, physician preference, and costs.[4] Irrational antimicrobial usage such as antibiotics in nonbacterial infections, inadequate dosage, and improper route has led to ineffective treatment, prolongation of illness, increased frequency of adverse drug reactions, suboptimal therapy, therapeutic failure, polypharmacy, which ultimately causes increased burden of medical cost as well as the emergence of antibiotic resistance.[5,6] The International Network for the Rational Use of Drugs (INRUD) was established in 1989 and developed various guidelines to promote the rational use of drugs in developing countries.[7]
Regarding the rationale use of antibiotics, sufficient literature is available in India and abroad.[8–10] As increased antibiotic resistance is having impact on economy of developing countries such as India, we thought this type of study will also help physicians to prescribe appropriate antibiotics. This observational study was designed to evaluate the antimicrobial usage in otolaryngology outpatient department. Based on the present study results, we can plan proper interventions and modifications at the level of the physician and the institution to promote rational antibiotic usage.
MATERIAL AND METHODS
An observational study was planned over a period of 8 months from July 2019 to February 2020 in ENT outpatient department (OPD) at Mamata General Hospital, Khammam in Telangana after obtaining approval from the Institutional Ethics Committee (IEC/IRB: 97/19).
Inclusion criteria
Patients attending ENT OPD with infective etiology who has given written consent. Patients of all age groups of both the sexes
Exclusion criteria
Inpatients
Follow-up visit patients
Seriously sick patients
Pregnant and lactating women
Sample size
As per our inclusion and exclusion criteria, a total of 562 prescriptions were collected that were having proper diagnosis and medications.
Parameters for evaluation
According to the World Health Organization (WHO), core drug prescribing indicators such as the average number of drugs per prescription (total number of drugs/total number of prescriptions), average number of antibiotics per prescription (total number of antibiotics/total number of prescriptions), average duration of antibiotic drug treatment (number of antibiotics for a particular duration/total number of antibiotics), and percentage of antibiotics prescribed by generic name (antibiotics prescribed with generic name/total number of antibiotics prescribed × 100) were evaluated.[11] The information regarding patients demographic details such as age, sex, clinical details such as type of ENT infections and antibiotic drug data (group, route of administration, dosage and duration) were analyzed.
Statistical analysis
Data entry was done in Microsoft office excel 2018 and analyzed. Results on categorical measurements are presented as number and percentage and using this, tables were generated.
RESULTS
A total of 562 prescriptions collected from the ENT OPD were classified according to the site of origin, which included 210 ear, 178 throat, and 136 nasal infections. The total number of drugs prescribed was 1,789, of which 703 were antibiotics. Based on the age group classification, 44.83% of the prescriptions belonged to patients of 21 to 40 years, followed by 1 to 20 years (29.53%) [Table 1]. Of total 562 prescriptions, 56.9% were males and remaining 43.1% were females. Most common infections observed were CSOM followed by sinusitis and tonsillitis [Table 2].
Male (n = 320) |
Female (n = 242) |
Total (N = 562) |
Percentage (%) |
|
|---|---|---|---|---|
< 1 year |
1 |
3 |
4 |
0.71 |
1–20 year |
79 |
87 |
166 |
29.53 |
21–40 year |
164 |
88 |
252 |
44.83 |
41–60 year |
58 |
49 |
107 |
19.03 |
61–80 year |
18 |
15 |
33 |
5.87 |
Total |
(56.9%) |
(43.1%) |
(100%) |
100% |
n, number of male and female prescriptions; N, total number of prescriptions
ENT infections (N = 562) |
Frequency of infections |
|
|---|---|---|
Frequency |
% |
|
Ear diseases (n = 210) |
||
CSOM |
91 |
16.2 |
Otitis externa |
34 |
6.04 |
ASOM |
33 |
5.87 |
Fungal infections (otomycosis) |
27 |
4.80 |
Furunculosis |
14 |
2.49 |
Aural polyp |
11 |
1.96 |
Nose diseases (n = 136) |
||
Sinusitis* |
77 |
13.70 |
Acute rhinosinusitis |
46 |
8.18 |
Vestibulitis |
7 |
1.24 |
Epistaxis |
6 |
1.06 |
Throat diseases (n = 178) |
||
Tonsillitis |
73 |
12.98 |
Pharyngitis |
48 |
8.54 |
Adenoiditis |
22 |
3.91 |
Laryngitis |
15 |
2.66 |
Submandibular swelling |
11 |
1.96 |
Parotid abscess |
9 |
1.60 |
Combined (n = 38) |
||
Pharyngitis+ CSOM |
21 |
3.73 |
Tonsillopharyngitis |
17 |
3.02 |
Abbreviations: ASOM, acute suppurative otitis media; CSOM, chronic suppurative otitis media; n, number of male and female prescriptions; N, total number of prescriptions.
*Sinusitis with polyps, sinusitis without polyps and fungal sinusitis.
Analysis of antibiotic prescriptions
In total, 66.01% of the patients received a single antibiotic, 27.58% of the patients received two antibiotics, and remaining 6.40% of patients did not receive any antibiotic. The average number of antibiotics prescribed per encounter was 1.25 [Figure 1]. Next, 52.9% of dosage forms were tablets, followed by 31.8% of capsules and 9.10% of syrups [Figure 2]. Also, 93.9% of antibiotics were prescribed by oral route, followed by 6.11% of topical application, whereas injectables were not prescribed.
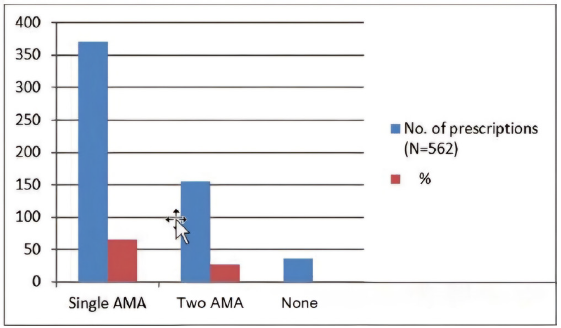
- Numberof antimicrobial agents used per prescription.
- Blue indicates total number of prescriptions. i.e. 562 Red indicates % of patients based on regime of antibiotics i.e. single, two and none
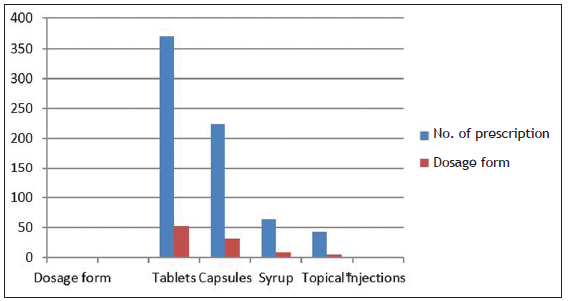
- Distribution of various dosage formulations of antibiotics prescribed.
- Blue indicates total number of prescriptions. i.e. 562 Red indicates % of patients based on regime of antibiotics i.e. single, two and none
In our study, penicillins (34.7%), cephalosporins (25%), and fluroquinolones (23.3%) were commonly prescribed antibiotics [Table 3]. Amoxicillin with clavulanic acid was observed to be the most common FDC, followed by cefpodoxime with clavulanic acid [Table 4]. Also, 70.3% antibiotics were prescribed for 3 to 5 days and 27.6% were prescribed for 6 to 10 days and 2.13% were for more than 10 days [Figure 3]. Most antibiotics prescribed were generic (65.57%) [Table 5].
Class of drugs |
Frequency (N = 703) |
% Consumption |
|---|---|---|
Penicillins |
244 |
34.7 |
Cephalosporins |
176 |
25 |
Fluoroquinolones |
164 |
23.3 |
Macrolides |
28 |
3.98 |
Antifungal drugs |
27 |
3.84 |
Miscellaneous* |
64 |
9.1 |
*Metronidazole, cotrimoxazole, bacitracin, linezolid, doxycycline, and mupirocin.
Class of antimicrobials |
Antimicrobial agents prescribed |
Frequency of prescribed antibiotics (N = 703) |
% of antibiotic consumption |
|---|---|---|---|
Penicillins (244) |
Amoxicillin |
4 |
0.56 |
Amoxicillin + clavulanic acid |
184 |
26.17 |
|
Ampicillin + cloxacillin |
56 |
7.96 |
|
Cephalosporins (176) |
Cefpodoxime + clavulanic acid |
154 |
21.9 |
Cefuroxime |
12 |
1.70 |
|
Cefixime |
10 |
1.42 |
|
Fluoroquinolones (164) |
Ciprofloxacin |
134 |
19.06 |
Ofloxacin |
22 |
3.13 |
|
Levofloxacin |
8 |
1.13 |
|
Macrolides (28) |
Azithromycin |
18 |
2.56 |
Clarithromycin |
10 |
1.92 |
|
Antifungal drugs (27) |
Clotrimazole |
18 |
2.56 |
Nystatin |
9 |
1.28 |
|
Metronidazole |
14 |
1.99 |
|
Others (64) |
Cotrimoxazole |
14 |
1.99 |
Bacitracin |
13 |
1.84 |
|
Linezolid |
12 |
1.70 |
|
Doxycycline |
08 |
1.13 |
|
Mupirocin |
03 |
0.42 |
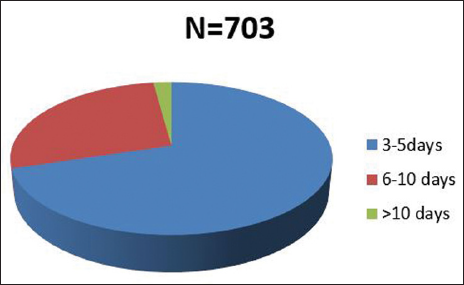
- Duration of antibiotics prescribed.
Parameter |
Number of drugs (N = 1789) |
Percentage (%) |
Number of antibiotics (n = 703) |
Percentage |
|---|---|---|---|---|
Drugs prescribed by brand name |
464 |
25.9 |
242 |
34.42 |
Drugs prescribed by generic name |
1,325 |
74.06 |
461 |
65.57 |
N, number of drugs; n, number of antibiotics
Analysis of Adjuvant Drug Prescriptions
Of 562 prescriptions, 256 (45.5%) had three drugs per prescription, followed by two drugs (21%) with an average of 3.18 [Figure 4]. In the adjuvant group, nasal decongestants were commonly prescribed (52%), followed by antihistamines (18%) and non-steroidal anti-inflammatory drugs (13%) [Figure 5].
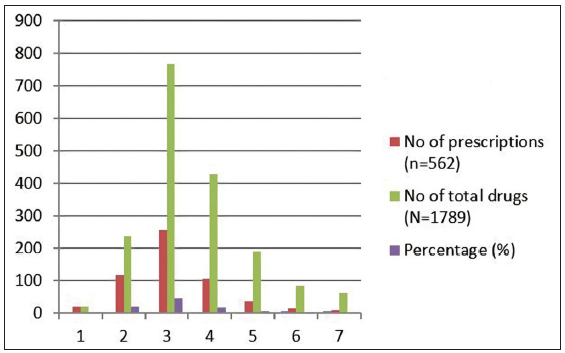
- Number of drugs prescribed per prescription.
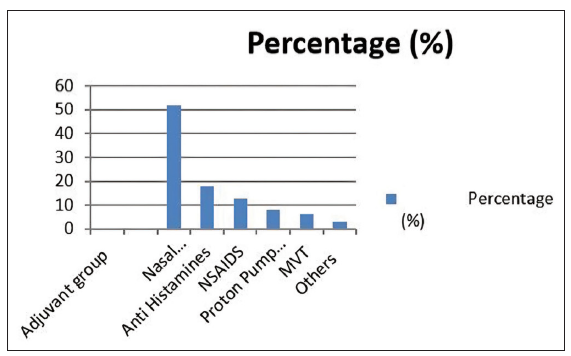
- Distribution of prescriptions based on the adjuvants prescribed.
DISCUSSION
In practice, while covering the most likely pathogens in the treatment of ENT infections is empirical, culture-sensitive antibiotics are prescribed for some times on need basis. The present observational study describes prescription pattern of antibiotics in the OPD of ENT department. These type of studies guide the rational use of drugs and also useful in making treatment cost-effective and beneficial to patients and reduce the medical burden in developing countries such as India.[12]
More number of antibiotic prescriptions were observed in the 21 to 40 years age group patients and the least were observed in the geriatric age group, similar to Ain et al (66.3% between 6 and 35 years age group and 2.17% in 66 to 85 years group).[13] In our study, 56.9% of prescriptions were male and 43.1% were female patients similar to studies by Ain et al (62.68% males) and Suman et al (62% males).[13,14] Higher ambulatory working adult male population and higher exposure to environmental pollutants and pathogens might be the cause of increased prevalence in males. In contrast to our study, more number of female patients (53.12%) were enrolled in a study by Harish et al.[15]
In this study, prescriptions with single antimicrobial agent were 66.01% and with two AMA were 27.58% which was similar to the study by Padwal et al (92.98% of prescriptions with one AMA and 2.10% with two AMA).[16] The average number of antibiotics per prescription was 1.25, which was lower than in the studies done by Suman et al (2015) (1.69),[14] Ain et al (2010) (1.58),[13] Pallavi et al (2016) (2.42),[4] and higher than Padwal et al (2015) (0.98).[16] Penicillins (34.7%), cephalosporins (25%), and fluoroquinolones (23.3%) were commonly prescribed antibiotics and in the FDC, amoxicillin with clavulanic acid was the commonest followed by cefpodoxime with clavulanic acid. Studies conducted by Suman et al (85%), Khan et al (75.68%), Bhat et al (77%), and Anandhasayanam et al (61%) have reported that β-lactam antibiotics were given the highest priority.[14,17–19] The change in the prescription pattern from a narrow spectrum to extended-spectrum penicillins could overcome the problem of antibiotic resistance. Lisha et al[20] observed an almost similar pattern of antibiotic prescription but in contrast to our study, 41% of injectables were prescribed. In our study, CSOM was the most common infection, followed by sinusitis and tonsillitis. Das et al (2005) also reported that CSOM was the commonest infection (60%) in their study.[5] The commonest route of administration was oral, followed by topical. No injectable antibiotics were prescribed. Similar findings such as zero injections were given out of 855 prescriptions in a study done by Padwal et al.[16] This absolute lack of use of injections indicate physicians' awareness regarding side effects related to the over use of injections.
The WHO recommendation for average number of drugs per prescription is 2 to2.5. However, in this study, it was 3.18 which is also reported by Khan et al (2.70),[17] indicating a trend of polypharmacy.[21] As the over prescribing of drugs has higher chances of drug–drug interactions, increased risk of adverse drug reactions, increase in unnecessary cost of treatment and most importantly antibiotic resistance average number of drugs per prescription should be reduced.[22,23] Analysis of prescription of adjuvants showed predominant prescription of nasal decongestants (52%) followed by antihistamines (18%), which are similar to those of Srinivasa et al's study with 60% of nasal decongestants.[24]
About 74.06% of drugs prescribed were generic, which is in contrast with other studies reporting a higher use of brand names.[13,25,26] In the present study, 96% of drugs prescribed were from the hospital formulary list, meaning that physicians are adhering to the list. Also, 95% of the drugs prescribed were from the National List of Essential Medicines, India. The WHO recommendation is 100% prescription of drugs from the essential drug list (EDL).[27] This study clearly showed the prescription pattern of antibiotics, increased prescriptions of generic drugs, and importance of rationale use of antibiotics, which would be useful for all practitioners to reduce the antibiotic resistance and unnecessary medical burden of people of India.
LIMITATIONS
The study was performed for a period of 8 months only. Seasonal variations in ENT infections and their prescribing patterns were not counted. Though the sample size was high, this study was conducted in one hospital only. In this study, antimicrobial therapy was based on empirical and clinical diagnosis as laboratory investigations were not done.
CONCLUSION
The pattern of prescribing a drug and its utilization plays a major role in advising a physician and hospital administration to prescribe antibiotics rationally and analyze its cost beneficiality. The present study though prescription pattern of antibiotics and adherence to the hospital formulary by the physicians in the hospital is encouraging, still there is a chance in reducing the number of drugs prescribed per patient. Extensive studies on the restricted use of antibiotics and updation of development to formulate guidelines for the treatment of common diseases through continuing medical education (CME) is needed. So that the patient and health care system on the whole will be benefitted.
Acknowledgments
Authors would like to extend their thanks to respected Dean and Principal and HOD for allowing us to conduct this study in the institution. Authors are also extremely grateful to the faculty of ENT department for their cooperation in the entire study period.
Author declaration
Ethics Committee approval was obtained for this present study.
Informed consent obtained from the patients included in the study.
Funding
None.
Conflicts of interest
None declared.
References
- Traditional Management of Ear, Nose and Throat (ENT) Diseases in Central Kenya. J Ethnobiol Ethnomed. 2006;2:54.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Upper Respiratory Tract Infections. Indian J Pediatr. 2001;68:1135-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prescribe Pattern of Drugs and Antimicrobials Preference in the Department of ENT at Tertiary Care SGM Hospital, Rewa, MP, India. J Pharm Biomed Sci. 2016;6:89-93.
- [Google Scholar]
- Antimicrobial Utilization Pattern in Outpatient Services of ENT Department of Tertiary Care Hospital of Eastern Nepal. Kathmandu Univ Med J. 2005;3:370-5.
- [PubMed] [Google Scholar]
- Analysis of Prescription Pattern of Antibiotic Drugs on Patients Suffering from ENT Infection Within Dhaka Metropolis, Bangladesh. Int J Basic Clin Pharmacol. 2017;6:257-64.
- [Google Scholar]
- Drug Utilization Studies: A Tool for Determining the Effectiveness of Drug Use. Br J Clin Pharmacol. 1983;16:301-4.
- [CrossRef] [PubMed] [Google Scholar]
- European Antimicrobial Resistance Surveillance System Group; European Surveillance of Antimicrobial Consumption Project Group Antimicrobial Drug Use and Resistance in Europe. Emerg Infect Dis. 2008;14:1722-30.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Profile of Antibiotic Consumption, Sensitivity and Resistance in an Urban Area of Andhra Pradesh, India. Singapore Med J. 2012;53:268-72.
- [PubMed] [Google Scholar]
- 2015. Accessed on June 08, 2019, at: http://www.wpro.who.int/entity/drug_resistance/resources/global_action_plan_eng.pdf
- [Google Scholar]
- 1993. How to investigate drug use in health facilities : selected drug use indicators. World Health Organization. Available at: https://apps.who.int/iris/handle/10665/60519
- [Google Scholar]
- WHO International Working Group for Drug Statistics Methodology, WHO Collaborating Centre for Drug Statistics Methodology & WHO Collaborating Centre for Drug Utilization Research and Clinical Pharmacological Services. (2003). Introduction to Drug Utilization Research. World Health Organization. Available at: https://apps.who.int/iris/handle/10665/42627
- Drug Utilization Pattern of Antibacterials Used in Ear, Nose and Throat Outpatient and Inpatient Departments of a University Hospital at New Delhi, India. J Pharm Bioallied Sci. 2010;2:8-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Assessment of Drug Usage Pattern of Antibiotics Used in ENT OPD of Tertiary Care Teaching Hospital. Int J Health Sci Res. 2015;5:290-7.
- [Google Scholar]
- Drug Utilization Study on Antibiotics Use in the Upper Respiratory Tract Infection. Int J Recent Trends in Sci Technol. 2014;10:299-302.
- [Google Scholar]
- Drug Use Pattern in the Ear, Nose and Throat Outpatient Department of a Rural Tertiary Care Teaching Hospital. NJPPP. 2015;5:212-6.
- [Google Scholar]
- Patterns of Prescription of Antimicrobial Agents in the Department of Otorhinolaryngology in a Tertiary Care Teaching Hospital. Afr J Pharm Pharmacol. 2011;5:1732-8.
- [Google Scholar]
- A Study of Prescription Pattern in the Drug Therapy of Ear, Nose and Throat Infections at a Tertiary Care Hospital in Mangalore. Int J Basic Clin Pharmacol. 2015;4:686-90.
- [Google Scholar]
- Drug Prescription Pattern Observation at a ENT OPD Department in a Tertiary Care Teaching Hospital at Malappuram District of Kerala. IJPSR. 2016;7:4157-63.
- [Google Scholar]
- Patterns of Antimicrobial Therapy in Acute Tonsillitis: A Cross-Sectional Hospital-Based Study from UAE. An Acad Bras Cienc. 2014;86:451-7.
- [CrossRef] [PubMed] [Google Scholar]
- WHO/INRUD Drug Prescribing Indicators at Primary Health Care Centres in Eastern Province, Saudi Arabia. East Mediterr Health J. 2012;18:1091-6.
- [CrossRef] [PubMed] [Google Scholar]
- Investigation on Antibiotics in a Hospital for a One-Year Period. Int J Clin Pharmacol Ther. 1995;33:32-3.
- [PubMed] [Google Scholar]
- A Survey of Inpatient Antibiotic Use in a Teaching Hospital. S Afr Med J. 1991;80:7-10.
- [PubMed] [Google Scholar]
- Prescribing Pattern of Antibiotics in ENT Outpatient Department in a Tertiary Care Teaching Hospital. Int J Basic Clin Pharmacol. 2020;9:1892-6.
- [Google Scholar]
- Pattern of Drug Utilization in the Treatment of Chronic Suppurative Otitis Media in a Tertiary Health Institution in Kaduna, Nigeria. J Health Sci. 2014;4:7-10.
- [Google Scholar]
- Pattern of Drug Utilization in Acute Tonsillitis in a Teaching Hospital in Nepal. Indian J Otolaryngol Head Neck Surg. 2003;55:176-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- 2015. Available at: https://www.nhp.gov.in/NHPfiles/NLEM%2C%202015.pdf







