Translate this page into:
Assessment of Clinical Profile in Patients Suffering from Non-radiographic Axial Spondyloarthropathy

*Corresponding author: Dr. Alhad Mulkalwar, Department of Medicine, Seth Gordhandas Sunderdas Medical College (GSMC) and King Edward Memorial (KEM) Hospital, Mumbai - 400012, Maharashtra, India. alhad.mulkalwar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Limaye S, More S, Nadkar M, Mulkalwar A, Jaju S, Haider H. Assessment of Clinical Profile in Patients Suffering from Non-radiographic Axial Spondyloarthropathy. Int J Recent Surg Med Sci. 2023;9:77-82. doi: 10.25259/IJRSMS-2022-8-4
Abstract
Objectives
Axial Spondyloarthritis is an inflammatory, immune-mediated condition comprising clinically dif- ferentiated ankylosing spondylitis (AS) and non-radiographic axial spondyloarthritis (nr-axSpA). Clinically, as the name suggests, nr-axSpA lacks definitive plain X-ray evidence of structural damage to the sacroiliac (SI) joint. This study was undertaken to assess the patients with newly diagnosed nr-axSpA clinically and compare the same with those with radiographic AS. The laboratory profile of patients suffering from nr-axSpA and their outcomes over three months were also studied.
Material and Method
This study was conducted in the Department of Medicine over 18 months in a tertiary health care institution, being a prospective observational type done with 43 subjects.
Results
We observed a major improvement as per ankylosing spondylitis disease activity score (ASDAS) criteria present among 53.49% of subjects, followed by clinically significant improvement among 27.91% of subjects. 18.60% of subjects did not show any improvement. 9.3 % of subjects showed radiological progression. Out of 8 cases that did not show improvement, all presented with lower back pain (LBP) and morning stiffness. 62.5% had peripheral arthritis. 87.5% had Schober’s test positive, flexion, abduction and external rotation (FABER) test (62.50%), and SI joint tenderness was found among 7.5% of subjects. A total of 4 (9.3%) patients showed radiological progression. They all have low back aches and morning stiffness, and three have peripheral arthritis at presentation. We found that patients who showed progression had higher mean erythrocyte sedimentation rate (ESR) and C-Reactive protein (CRP) levels (45 and 36.5, respectively) values and very high disease activity as per ASDAS and bath ankylosing spondylitis disease activity index (BASDAI) criteria.
Conclusion
There is a great scope and need for research to differentiate the magnetic resonance imaging (MRI) changes in the normal population against the patients with spinal diseases to be able to use MRI with precision in patients with non-radiographic axial spondyloarthropathy (nr-axSpA). As assessed, physiotherapy and Non-steroidal anti-inflammatory drugs (NSAIDS) are currently first-line therapy for patients suffering from nr-axSpA.
Keywords
ASDAS criteria
Schober’s test
spondyloarthropathy
Introduction
Axial Spondyloarthritis is an inflammatory, immune-mediated condition comprising clinically differentiated ankylosing spondylitis (AS) and non-radiographic axial spondyloarthritis (nr-axSpA).[1] Clinically, as the name suggests, non-radiographic axial spondyloarthritis lacks definitive plain x-ray evidence of structural damage to the sacroiliac (SI) joint.[2] Due to the subjectivity of radiological interpretation of SI joint involvement, differentiating AS and nr-axSpA could be more accurate. Patients with axial spondyloarthritis usually present with back pain due to the involvement of the SI joint. They can also present with complaints like dactylitis, peripheral arthritis, enthesis, anterior uveitis, psoriasis, Crohn’s disease, or ulcerative colitis.[3] There has been an increased understanding of axial spondyloarthritis over the period. However, still, there remains difficulty in differentiating axSpA from common mechanical backache, also accounting lack of accurate diagnostic criteria leading to an increased burden on patients and health care systems.[4,5] This factor adds further in nr-axSpA wherein the disease burden at personal and societal levels is similar to that in rheumatoid arthritis (RA) and SpA conditions, with a rise in the cost of treatment due to lesser comparative productivity in the assessment and management aspect of the disease.[6] There is much scope for improvement in understanding and management of nr-axSpa to prevent its conversion to AS, lessen the risk of complications like a fusion of the spine or fractures, prevent deterioration of range of motion, and therefore diminishing the financial impact of the same on patients, healthcare institutions and thus the society.[7]
This study was undertaken to assess the patients with newly diagnosed nr-axSpA clinically and compare the same with those with radiographic AS. We also studied the laboratory profile of patients suffering from nr-axSpA and their outcomes over three months.
Material and Methods
This was a prospective type of observational study carried out at the Medicine department of a tertiary healthcare center conducted over 18 months. We proceeded with the study only after obtaining clearance from the institution’s Ethics Committee and permission from the appropriate authority. The sample size was calculated to be 43 patients. Newly diagnosed treatment naïve patients aged between 18 and 45 years, willing to consent, were a part of the study. Pregnant and lactating females and those allergic to drugs of the sulfa group were not included. The step-by-step workup protocol of the patients is depicted in Figure 1.
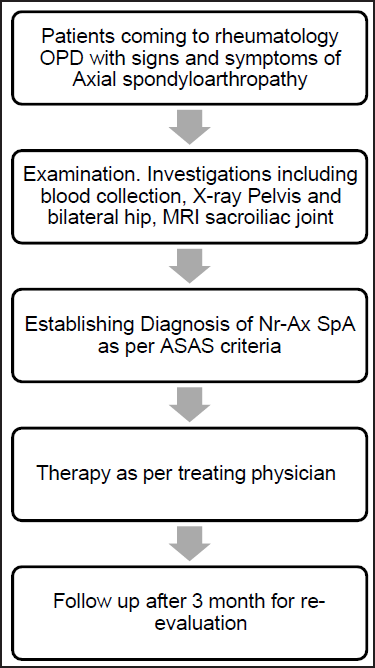
- The step-by-step workup protocol of the study participants.
Written informed consent was taken—detailed history including Low Back Pain (LBP), Early Morning Stiffness, and Peripheral arthritis. Uveitis, Enthesitis, Dactylitis, Constitutional symptoms, etc., obtained. Clinical examination, including general and special tests like Schober’s, FABER, Wall occiput distance, Sacroiliac tenderness, and chest expansion obtained. Exceptional scores ASDAS and BASDAI were calculated. Relevant blood investigations and treatment started as per the physician’s notes. The patient was asked to follow up after three months when a repeat complete physical and laboratory investigation were done. Data were analyzed using the Mcnemar test (for qualitative data assessment) and using the paired t-test (for quantitative data assessment).
Results
Most of the subjects belonged to the age group of 26 to 35 years (46.51%), followed by 18 to 25 years (27.91%) and 36 to 45 years (25.58%). The mean age group of the study subjects was 30.34 ± 7.47 years; the median age is 30 years [Table 1]. The gender wise distribution of study participants is depicted in Table 2.
| Age distribution | Number of subjects | Percentage |
|---|---|---|
| 18 to 25 years | 12 | 27.91 |
| 26 to 35 years | 20 | 46.51 |
| 36 to 45 years | 11 | 25.58 |
| Total | 43 | 100.00 |
| Mean age | 30.34 ± 7.47 years | |
| Median age | 30 years | |
| Gender wise distribution | Number of subjects | Percentage |
|---|---|---|
| Male | 38 | 88.37 |
| Female | 5 | 11.63 |
| Total | 43 | 100.00 |
| M:F ratio | 7.6:1 | |
We observed that low backache was the most typical complaint among all subjects (100%), followed by morning stiffness among 95.35% of subjects, peripheral arthritis among 53.49% of subjects, and fever and uveitis among 25.58% of subjects, fatigue, and enteritis among 11.63% of subjects. On assessing the patients on follow-up after three months, LBP was noted among 30.23% of subjects, while morning stiffness was reported among 9.30% of subjects, Peripheral neuritis among 18.60% of subjects, and Enthesitis and Dactylitis among 2.33% of subjects. It was observed that the majority of the complaints were reduced significantly after three months [Table 3].
| Clinical presentation | On admission | After three months | Significance | ||
|---|---|---|---|---|---|
| Number | % | Number | % | ||
| LBP | 43 | 100.00 | 13 | 30.23 | – |
| Morning stiffness | 41 | 95.35 | 4 | 9.30 | 63.81, <0.0001 |
| Fever | 11 | 25.58 | 1 | 2.33 | 9.68, 0.0018 |
| Fatigue | 5 | 11.63 | 0 | 0.00 | – |
| Weight loss | 0 | 0.00 | 0 | 0.00 | – |
| Peripheral arthritis | 23 | 53.49 | 8 | 18.60 | 11.34, 0.00075 |
| Uveitis | 11 | 25.58 | 0 | 0.00 | 0 |
| Enthesitis | 5 | 11.63 | 1 | 2.33 | 2.86, 0.09 |
| Dactylitis | 2 | 4.65 | 1 | 2.33 | 0.34, 0.556 |
| Pallor | 0 | 0.00 | 0 | 0.00 | 0 |
| Cyanosis | 0 | 0.00 | 0 | 0.00 | 0 |
| Icterus | 0 | 0.00 | 0 | 0.00 | 0 |
| Clubbing | 0 | 0.00 | 0 | 0.00 | 0 |
| Lymphadenopathy | 0 | 0.00 | 0 | 0.00 | 0 |
We also assessed the examination findings among the study subjects. We observed that chest expansion was more than 5 cm among 44.19% of subjects on admission, whereas it improved to 97.67% after three months. Schober’s test was positive among 88.37% of subjects. In contrast, the FABER test was positive among 69.77% of subjects, sacroiliac joint tenderness was observed among 83.72% of subjects, and the wall occiput test was positive among 18.601% of study subjects. The findings improved significantly after three months of follow-up [Table 4].
| Examination findings | On admission | After three months | Significance | ||
|---|---|---|---|---|---|
| Number | % | Number | % | ||
| Chest expansion (> cm) | 19 | 44.19 | 42 | 97.67 | 29.83, <0.0001 |
| Schober’s Test | 38 | 88.37 | 12 | 27.91 | 32.29, <0.0001 |
| Faber Test | 30 | 69.77 | 5 | 11.63 | 30.11, <0.0001 |
| Sacroiliac Joint Tenderness | 36 | 83.72 | 25 | 58.14 | 6.82, 0.008 |
| Wall Occiput Test | 8 | 18.60 | 6 | 13.95 | 0.34, 0.559 |
We also assessed X-ray pelvis (New York grading). We observed grade 0 findings among all subjects on presentation, whereas among 93.02% of subjects on follow-up [Table 5].
| X-ray of pelvis with Bilateral hip (New York Grading) | On admission | After three months | ||
|---|---|---|---|---|
| Number | % | Number | % | |
| Grade 0 | 43 | 100.00 | 40 | 93.02 |
| Grade 1 | 0 | 0.00 | 3 | 6.98 |
We observed a mean pulse rate of 82.84, a mean body temperature of 37.98, and a mean respiratory rate (RR) of 18.12 on admission. After follow-up, the mean pulse was 95.91, the mean body temperature was 37.93, and the mean Respiratory Rate was 15.79. We also studied the hematological parameters among the study subjects. Mean levels on admission and after follow-up after three months are mentioned in Table 6.
| Hematological investigations | On admission | After three months |
|---|---|---|
| Hemoglobin | 12.78 | 13.20 |
| TLC | 8250.00 | 8220.70 |
| Platelet | 2.61 | 2.74 |
| BUN | 10.99 | 10.85 |
| Serum creatinine | 1.08 | 1.10 |
| TP | 7.98 | 8.08 |
| Albumin | 3.69 | 3.74 |
| Total Bilirubin | 0.86 | 0.81 |
| Direct Bilirubin | 0.45 | 0.84 |
| SGOT | 35.05 | 29.72 |
| SGPT | 25.23 | 25.74 |
| ALP | 158.58 | 169.37 |
| RBS | 92.84 | 90.95 |
| Uric acid | 4.81 | 4.66 |
| CRP | 34.51 | 14.04 |
| ESR | 33.42 | 16.61 |
TLC: Total leukocyte count, BUN: Blood urea nitrogen, SGOT: Serum glutamic-oxaloacetic transaminase, SGPT: Serum glutamic pyruvic transaminase, ALP: Alkaline phosphatase, RBS: Random blood sugar, CRP: C-Reactive protein, ESR: Erythrocyte sedimentation rate, TP: Total protein,
The mean ASDAS score was 4.22 ± 2.20 among the study subjects. On admission, the majority of the subjects had ASDAS scores of more than 3.5 (81.40%), followed by a score between 2.1 to 3.5 (18.60%). In the follow-up examination, most subjects had ASDAS scores between 1.3 to 2.1 (48.84%), followed by 2.1 to 3.5 (37.21%), as seen in Table 7.
| ASDAS score | On admission | After three months | ||
|---|---|---|---|---|
| Number | % | Number | % | |
| Less than 1.3 | 0 | 0.00 | 2 | 4.65 |
| 1.3 to 2.1 | 0 | 0.00 | 21 | 48.84 |
| 2.1 to 3.5 | 8 | 18.60 | 16 | 37.21 |
| More than 3.5 | 35 | 81.40 | 4 | 9.30 |
| Total | 43 | 100.00 | 43 | 100.00 |
The mean BASDAI score was 4.57 ± 2.31 among the study subjects. On admission, most subjects had a BASDAI score of more than 4 (62.79%), followed by a score of less than 4 (37.21%). In the follow-up examination, most subjects had a BASDAI score of less than 4 (97.67%). The findings were statistically significant. (The chi-square statistic is 36.4921. The p-value is < 0.00001. Significant at p < .05.) [Table 8].
| BASDAI score | On admission | After three months | ||
|---|---|---|---|---|
| Number | % | Number | % | |
| Less than 4 | 16 | 37.21 | 43 | 97.67 |
| More than 4 | 27 | 62.79 | 1 | 2.33 |
| Total | 43 | 100.00 | 43 | 100.00 |
Significance: The chi-square statistic is 36.4921. The p-value is < 0.00001. Significant at p < .05.
We also assessed the severity according to the ASDAS score. We observed that most subjects had very high disease severity (81.40%), followed by high disease severity among 18.60% of study subjects.
It was observed that most subjects with greater ASDAS scores had greater BASDAI scores. The difference was statistically significant, as seen in Table 9 (The chi-square statistic is 8.412. The p-value is .003728. Significant at p < .05.)
| On admission | BASDAI score | |||
|---|---|---|---|---|
| ASDAS score | Less than 4 | More than 4 | ||
| Number | % | Number | % | |
| Less than 1.3 | 0 | 0.00 | 0 | 0.00 |
| 1.3 to 2.1 | 0 | 0.00 | 0 | 0.00 |
| 2.1 to 3.5 | 7 | 87.50 | 1 | 12.50 |
| More than 3.5 | 11 | 31.43 | 24 | 68.57 |
| Total | 18 | 41.86 | 25 | 58.14 |
Significance: The chi-square statistic is 8.412. The p-value is .003728. Significant at p < .05.
We observed significant improvement among 53.49% of subjects and clinically meaningful improvement among 27.91%. At the same time, 18.60% of subjects showed no improvement. Out of 8 cases that did not show improvement, all presented with LBP and morning stiffness. 62.5% had peripheral arthritis. 87.5% had Schober’s test positive, FABER Test (62.50%), sacroiliac joint tenderness was found among 87.5% of subjects, and wall occiput test positive among 12.5%. MRI findings of the patients are depicted in Table 10.
| MRI findings absent | MRI findings present | |
|---|---|---|
| At presentation | 14 | 29 |
| At three months | 10 | 33 |
4 Patients who had normal MRIs at first progressed to show evidence of spondyloarthropathy on follow-up (MRI progression). All four patients had lower backache and morning stiffness, and 3 (75%) had peripheral arthritis on presentation. They were also found to have raised mean CRP and ESR values, with mean values of 45 and 36.5, respectively, and ASDAS and BASDAI mean scores of 3.76 and 5.3, respectively, suggesting very high disease activity.
Discussion
Non-radiographic axial spondyloarthritis (nr-axSpA) is a form of axial inflammatory arthritis without significant erosive involvement of the sacroiliac joint. It can develop into (AS, also termed radiographic axSpA) in a specific group of people and thus can be associated with deteriorating quality of life in them. With recent advancements in MRI, there has been an improvement in the diagnosis of the condition. However, there’s still less clarity in the criteria for classifying the same amongst the international community. Further studies are underway to define the classification and determine appropriate modalities given the diagnosis of nr-axSpA.
Gavali M et al., in the study on a comparison between clinical and lab profiles of nr-axSpA and AS, concluded that patients with AS were older at presentation and had more extended disease duration history than those with nr-axSpA.[8]
Benchérifa S et al., in the study on a comparison of disease activity parameters, disease activity, and functional scores between r-axSpA and nr-axSpA, didn’t find any significant difference in demographic and clinical characteristics among the two except psoriasis, which was more common amongst r-axSpA patients.[9]
Cantarini et al., in a study on the effectiveness of Adalimumab (ADA) in nr-axSpA suggested a favorable risk-benefit profile for ADA in patients of nr-axSpA inadequately responding to NSAIDS.[10]
Denis Poddubnyy et al., in their study, observed that nr-axSpA is a significant differential diagnosis in patients with diagnosed backaches, especially in ones with recent onset backaches. Moreover, they found that high NSAID intake (NSAIDs index > 50) in AS was associated with slower radiographic progression. No such association was found in patients with nr-axSpA.[11]
Ravinder Goswami et al., in the study on the presence of spondyloarthropathy in hypoparathyroid patients, observed that spondyloarthropathy is associated with a longer duration of hypoparathyroidism and that in patients of sporadic idiopathic hypoparathyroidism, spondyloarthropathy is an important clinical entity which needs to be distinguished from AS due to difference in the management of both the conditions.[12]
David McCormick et al., in the study on tumor necrosis factor (anti-TNF) response rates in r-axSpA and nr-axSpA, showed equal response rates to anti-TNF therapy in both groups after three-month therapy.[13]
Conclusion
Further research is required to determine optimal MRI usage in nr-axSpA to differentiate SI joint changes in normal populations versus ones in spinal diseases. First-line treatment for nr- axSpA remains NSAIDs and physiotherapy. Other treatment modalities include anti-TNF drugs, Janus kinase (JAK) inhibitors, and drugs directed at IL-17 and IL-23. Much active research is being done in the classification, imaging, and treatment of nr-axSpA; hence the future to improve patients’ lives with nr-axSpA looks promising.
Acknowledgment
None.
Ethical Approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patients consent
Patient consent is not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- The concept of spondyloarthritis: where are we now? Best Pract Res Clin Rheumatol. 2014;28:663-72.
- [CrossRef] [PubMed] [Google Scholar]
- The development of assessment of spondyloarthritis international society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis. 2009;68:777-83.
- [CrossRef] [PubMed] [Google Scholar]
- Non-radiographic axial spondyloarthritis patients without initial evidence of inflammation may develop objective inflammation over time. Rheumatology (Oxford).. 2017;56:1162-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- 2021 Feb 11. Available from: https://pubmed.ncbi.nlm.nih.gov/22915622/ [Last accessed on 2022 Feb 12]
- Prevalence of peripheral and extra-articular disease in ankylosing spondylitis versus non-radiographic axial spondyloarthritis: A meta-analysis. Arthritis Res Ther. 2016;18:196.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The assessment of the spondyloarthritis international society concept and criteria for the classification of axial spondyloarthritis and peripheral spondyloarthritis: A critical appraisal for the pediatric rheumatologist. Pediatr Rheumatol Online J. 2012;10:14.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The prevalence of HLA–B27 in the US: Data from the US National Health and Nutrition Examination Survey, 2009. Arthritis Rheum. 2012;64:1407-11.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of clinical and laboratory profile of non-radiographic axial spondyloarthritis and ankylosing spondylitis. Indian J Rheumatol 2015:377.
- [Google Scholar]
- Radiographic axial versus non-radiographic axial spondyloarthritis: Comparison of the disease activity parameters and the disease activity and functional scores: RBSMR study. Int J Clin Rheumatol. 2019;14:282.
- [Google Scholar]
- Effectiveness of adalimumab in non-radiographic axial spondyloarthritis: Evaluation of clinical and magnetic resonance imaging outcomes in a monocentric cohort. Medicine. 2015;94:e1170.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mechanism of new bone formation in axial spondyloarthritis. Curr Rheumatol Rep. 2017;19:55.
- [CrossRef] [PubMed] [Google Scholar]
- Presence of spondyloarthropathy and its clinical profile in patients with hypoparathyroidism. Clin Endocrinol. 2008;68:258-63.
- [CrossRef] [PubMed] [Google Scholar]
- Anti-TNF response rates in radiographic and non-radiographic axial spondyloarthropathy. Ann Rheum Dis. 2015;74:e21.
- [CrossRef] [PubMed] [Google Scholar]







