Translate this page into:
Clinical Outcomes of Unilateral Biportal Endoscopy in Lumbar Disc Herniation and Degenerative Lumbar Canal Stenosis

*Corresponding author: Dr. Saurabh Shrikant Kulkarni, Department of Orthopedics, Mahatma Gandhi Mission’s Medical College and Hospital, Chhatrapati Sambhajinagar, Maharashtra, India. saurabh711.kulkarni@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gaike CV, Kardile SD, Gadekar GN, Kulkarni SS. Clinical Outcomes of Unilateral Biportal Endoscopy in Lumbar Disc Herniation and Degenerative Lumbar Canal Stenosis. Int J Recent Surg Med Sci. 2025:11(e004). doi: 10.25259/IJRSMS_1_2025
Abstract
Objectives
This study aimed to assess the clinical outcomes in patients operated with UBE for lumbar disc herniation (LDH) and degenerative lumbar canal stenosis (DLCS) at our center.
Material and Methods
The subjects consisted of 50 patients aged 40-70 years who underwent UBE for LDH and DLCS. They were analyzed retrospectively. Outcomes of the patients were assessed with respect to operation time, hospital stay, complications, visual analog scale (VAS) for back and leg pain, and the Oswestry disability index (ODI).
Results
The average operative time for the procedure was 70-90 minutes. The average hospital stay was two days. The VAS score for back pain, leg pain, and ODI scores had significantly reduced at the six-month follow-up. In patients with DLCS, all could walk comfortably to over two kilometers at the six-month follow-up. Recurrence of symptoms was seen in one patient with LDH. However, no intra-operative or post-operative complication was noted. No surgical site infection was encountered.
Conclusion
UBE for the treatment of degenerative lumbar diseases is a safe, effective, and ergonomically comfortable surgical technique under a clear and wide endoscopic view. Segmental stability could be preserved since it allows over-the-top decompression easily without the removal of the spinous process & spinous ligaments. However, large-scale comparative studies will be needed to assess the differences in clinical outcomes and infection rates with other procedures.
Keywords
Hospital stay
Lumbar canal stenosis
Lumbar disc herniation
Pain
Unilateral biportal endoscopy
INTRODUCTION
Lumbar disc herniation (LDH) is a clinical condition where the intervertebral disc is displaced from the intervertebral disc space into the vertebral canal, producing symptoms [Figure 1]. LDH manifests as radicular pain predominantly associated with numbness or neurological deficit depending upon the location and size of the herniated disc causing the neural compression. Degenerative lumbar canal stenosis (DLCS) is a clinical syndrome resulting from a degenerative cascade in the spine attributed to pathoanatomical changes like- disc degeneration, desiccation of nucleus pulposus with fissuring in annulus fibrosus, thinning of vertebral end plates and eventually loss of disc space [Figure 2]. As the degenerative arthritis of the spine progresses, it results in the instability and hypermobility of the spinal segment, which can lead to hypertrophy of the facet joint and ligamentum flavum, eventually causing stenosis and compression of the neural structures.[1,2] The venous congestion caused by this cascade produces symptoms referred to as intermittent neurological claudication, which was encountered as the chief symptom in patients with DLCS in this study. Wide laminectomy with or without concomitant fusion procedures is considered the standard surgical procedure.[3] This classical approach usually involves extensive soft tissue dissection and a longer retraction time, which would result in prolonged post-operative lower back pain.[4] A minimally invasive approach towards decompression in such patients has been shown to be associated with better control of immediate postoperative pain with significantly improved clinical outcomes.[5] In patients with lumbar disc herniations, current evidence-based recommendations suggest the use of conservative treatment in the absence of a neurological deficit.[6] Although nonsurgical care remains the mainstay of initial treatment, discectomy surgery is applied to effectively alleviate symptoms that persist for prolonged periods.[7,8]
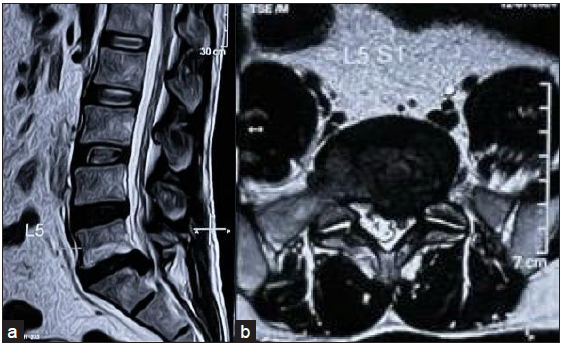
- Lumbar disc herniation (LDH) (a) MRI T2w sagittal cut, (b) MRI T2w axial cut.
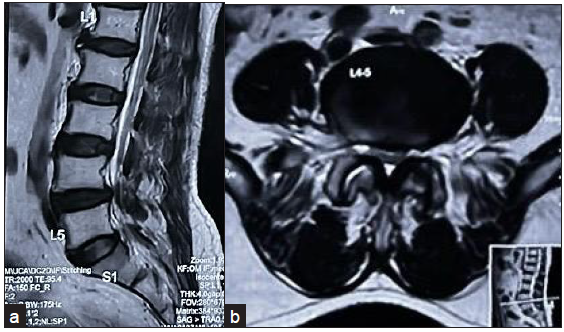
- Degenerative lumbar canal stenosis (DLCS) (a) MRI T2w sagittal cut, (b) MRI axial cut.
The unilateral biportal endoscopic (UBE) decompression technique is a percutaneous endoscopic technique. It is performed through two separate small incisions on the same side of the spinous process and does not involve extensive soft tissue dissection like the conventional wide laminectomy and decompression. UBE is not confined by the working tube or the working channel. With continuous high-pressure normal saline irrigation and high-definition arthroscope, the surgeon can do very precise decompression in a clear and magnified surgical field. UBE has been shown to decompress a greater area in the same amount of time compared to conventional micro-endoscopic and full-endoscopic spine surgery (FESS) decompression techniques.[9,10] UBE spinal surgery has gradually expanded in recent years for the treatment of various disorders, including lumbar degenerative diseases.[11-14] The benefits of UBE surgery are widely thought to include a larger field of vision, flexible operation, minimal invasiveness, complete nerve decompression, and a quicker recovery.[15]
In this study, we aim to analyze the clinical outcomes of patients who underwent UBE for a single-level LDH or DLCS.
MATERIAL AND METHODS
Patient selection
Fifty patients with single-level DLCS (19 patients) & LDH (31 patients) operated on using the UBE technique were retrospectively reviewed in this study. This included patients from the 40-70 years age group. The majority of the patients i.e., 34 (68.0%), were male. All the patients were assessed in a retrospective manner six months postoperatively.
Outcomes were assessed with:
-
1)
Operation time,
-
2)
Hospital stay,
-
3)
Complications,
-
4)
Visual analog scale (VAS) for back and leg pain,
-
5)
Oswestry disability index (ODI).
Inclusion criteria
-
1.
Procedure- Unilateral Biportal endoscopy
-
2.
Single-level involvement
-
3.
Pathology of lumbar disc herniation or degenerative lumbar canal stenosis
-
4.
Age 40-70 years
-
5.
Patients with a completed follow-up period of six months
Exclusion criteria
-
1.
Open procedure
-
2.
Preexisting degenerative scoliosis (Cobb’s angle >20 degrees)
-
3.
Pre-operative instability
-
4.
History of prior lumbar surgery
-
5.
Multilevel involvement
-
6.
Associated neurological deficit like cauda equine syndrome
Surgical technique
The patient is positioned prone position over the radiolucent frame in a flexed position so as to obliterate the lumbar lordosis [Figure 3]. Marking of the pathological level was done using a fluoroscope in anteroposterior (AP) and lateral views like we do in the microscopic technique. A proper anterior-posterior image can only be obtained with the fluoroscope angled parallel to the disc space. For draping, we used specialized waterproof drapes which have an outflow for normal saline fluid. UBE was performed through two separate small surgical ports (endoscope port and working port) on the same side of the spinous process. UBE is usually done from the left side. For a right-handed person, the scopic port is proximal, and the working port is distal. However, with experience, surgeons can switch the ports as per the need.
-
1)
Working/Instrument port – transverse 10 mm to 15 mm port is made at the Inferomedial border of the distal pedicle (for instrumentation & saline outflow)
-
2)
Endoscope port – A small 5 mm transverse port was made in line with the medial border of the pedicle, approximately 3 cm proximal to the working port, which is subject to patient build (for Scope & saline inflow) [Figure 4].

- Prone position.
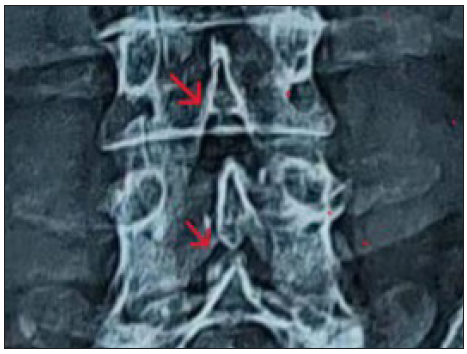
- Spinolaminar junction. Red arrow - Depicting the spinolaminar junction.
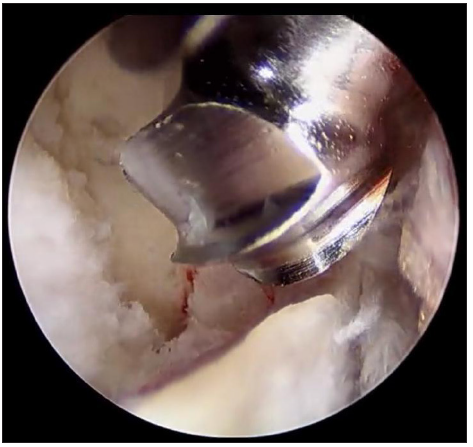
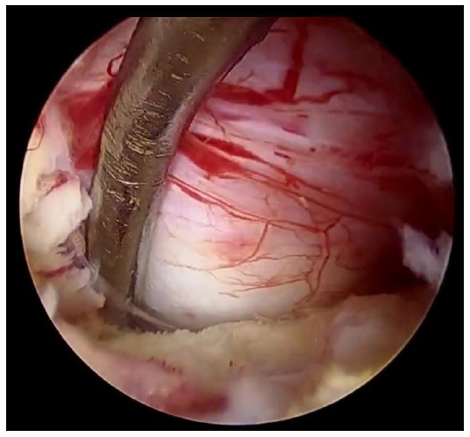
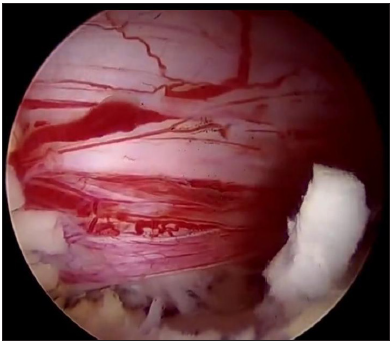
We maintained the saline fluid pressure using the gravity-assisted method rather than using the pressure pumps. To ensure free outflow of irrigation fluid, multifidus muscle was atraumatically separated using the blunt muscle-splitting technique with a serial dilator touching the lamino-spinal junction, separated with a blunt muscle detacher. A low-voltage radiofrequency probe is a safe means to control minor muscle hemorrhage. For more severe cancellous bone bleeds, bone wax can be helpful. The spino-laminar junction [Figure 5], which is the intersection of the superior vertebra’s lower laminar margin and the spinous process, is the first target location for decompression. Ipsilateral decompression was performed first on the pathological lesion site. Laminotomy was done using a high-speed burr followed by Kerrison rongeurs starting at the spino-laminar junction till the midline cleft of ligamentum flavum is seen, which indicates the midline portion of the spinal canal [Figure 6]. The ipsilateral lamina was then burred and removed till the upper border of ipsilateral flavum was visualized. For a case of LDH, the ligamentum flavum was removed starting at the upper margin with Kerrison punches. The traversing nerve root can be visualized directly under high magnification, which was retracted along with the dura using a blunt dura retractor to visualize the disc [Figure 7]. Annulotomy was performed, following which the disc fragments were removed using disc punches [Figure 8]. While operating a case of DLCS, ligamentum flavum was not removed immediately after ipsilateral laminotomy. Ligamentum flavum was detached from the undersurface of the opposite side lamina. It was preserved as a protective layer for dura like a cottonoid while burring the opposite side undersurface of the lamina. Once the bony work was complete, the flavum was removed carefully using Kerrison punches till the central canal and lateral recess was decompressed completely. Complete decompression was made until the lateral borders of the bilateral traversing nerve roots were exposed [Figure 9]. Adequate decompression can be assessed by visualizing nerve root mobility using a blunt dura retractor.
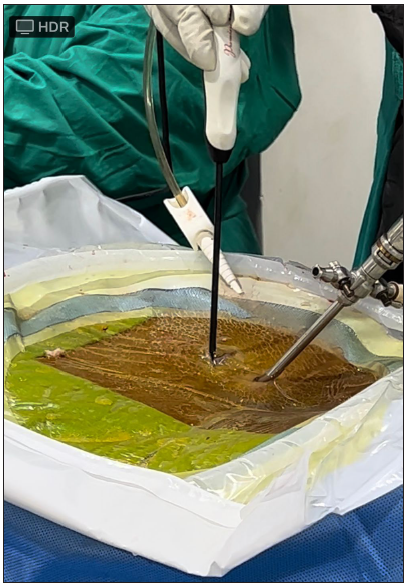
- Port assembly.
- High-speed burr laminotomy.
- Lumbar disc herniation at the shoulder of nerve root.
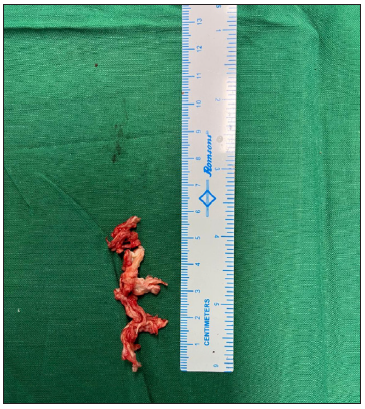
- Excised disc fragments.
- Decompressed nerve root.
Statistics
Data was entered in Microsoft Excel and analyzed using SPSS version 20.0th Mean and SD were calculated for quantitative variables and proportions were calculated for categorical variables. Paired t-test was applied to check the significance difference between pre and post-treatment. P- Value of <0.05 was considered statistically significant.
RESULTS
Demographic characteristics
A total of 50 patients, LDH (31 cases) and DLCS (19 cases), with a mean age of 51.62 years, were studied retrospectively over six months. Males predominated, with a total of 34 men (68%) and 16 females (32%). Out of all the patients with LDH - 12 patients had L4-5 disc prolapse, 12 patients had L5-S1 disc prolapse, and seven patients had L3-4 disc prolapse. Out of the patients with DLCS – nine patients had L4-5 stenosis, six patients had L5-S1 stenosis, and four patients had L3-4 stenosis
Outcomes of the surgery
The mean operative time for the procedure was 70 – 90 minutes. The average hospital stay was two days. The VAS scores and ODI decreased significantly in the two groups after the operation as compared to the preop values (p<0.05). The average VAS for back pain reduced from 5.04±1.37 to 0.47±0.66 at the six-month post-op follow-up. Average VAS leg pain reduced from 6.3±1.1 pre-operatively to 0.67 ±1.34 at the six-month post-op follow-up. The average ODI score at the final follow-up reduced significantly from 49.39±7.92 to 12.5±2.5 [Table 1]. In patients with DLCS, claudication distance was less than 500m preoperatively. All these patients could walk comfortably to over 2 km at the six-month follow-up period.
| Time | VAS (back pain) | VAS (leg pain) | ODI (%) |
|---|---|---|---|
| Pre-operative | 5.04 ± 1.37 | 6.3 ± 1.1 | 49.39 ± 7.92 |
| 6 month follow up | 0.47 ± 0.66 | 0.67 ± 1.34 | 12.52 ± 2.51 |
| P value |
P<0.0001 S |
P<0.0001 S |
P<0.0001 S |
S: Significant, VAS: Visual analogue scale, ODI: Oswestry disability index
Reoperations and complications
No intra-op complications (dural tear) or post-operative fluid-related complications (pulmonary oedema, cerebral oedema) were noted. No deaths were observed during the study. However, recurrence of symptoms was seen in one case of LDH i.e. two percent. Reoperation consisted of open laminectomy and decompression. No surgical site infection was encountered at the final follow up period.
DISCUSSION
To maintain the overall segmental stability and decrease post-operative morbidity, numerous minimally invasive surgical techniques have been devised with the objective of achieving adequate neural decompression with minimal soft tissue damage, shortening hospital stay, and optimizing peri-operative pain and time to recovery. We used the unilateral biportal endoscopic technique, which permits flexible handling and enables us to utilize instruments in sensitive regions while safeguarding neural elements and maintaining midline stabilizing structures. To avoid post-operative instability, especially in DLCS, midline stabilizing structures (spinous process, supraspinous and interspinous ligaments), pars, and facet joints must be preserved. More than 90% of the facet joint on the contralateral side and more than 80% of the facet joint on the approach side can be preserved using the UBE technique.[16]
The UBE integrates the benefits of both traditional open decompression and fully endoscopic techniques. It enables the use of standard open surgery tools through one portal, while also utilizing routine arthroscopic instruments, eliminating the need for specialized endoscopic tools.
By using a biportal endoscopic technique, it is possible to avoid injuring the erector spinae and multifidus as muscles are dilated and not cut, which would otherwise occur in traditional surgery. One of the most important benefits of UBE is faster recovery due to minimal injury to the soft tissue, which leads to early ambulation and shorter hospitalization.[17,18] Many studies comparing the effectiveness of UBE with other minimally invasive spine surgeries are being conducted, demonstrating that UBE can provide adequate decompression with a smaller incision with excellent clinical outcomes.[19-22]
Continuous irrigation with normal saline ensures a clear view during surgery, helps compress the dura, and improves the expansion of the epidural space throughout the procedure and washout of the debris. A bipolar cautery used under continuous saline irrigation can assist in controlling intraoperative bleeding more effectively by reducing the risk of thermal damage and post-operative epidural hematomas.[23]
Surgical microscopes or exoscopes can be used in spine surgeries for better visualization and understanding of neural structures, but the cost can be a limiting factor for the same. Hence most surgeons use surgical loops for enhanced vision and accuracy. However, continuous use of surgical loops can cause significant neck pain in the long run since the surgeon has to flex his neck while doing surgeries. Most orthopedic hospitals have arthroscopic systems. By combining the arthroscopic system and routine spine instruments, surgeons can start doing spine surgeries using the UBE technique. UBE provides great magnification of the surgical field and neural structures. Surgeries can be done without the need for extra specialized costly equipment with an ergonomically better surgical environment which makes it easier to do over-the-top decompression of the opposite side without removal of supraspinous and interspinous ligaments.
Our study’s limitations are the short duration of follow-up, a limited sample size, and no comparison group. UBE has shown clinically significant clinical outcomes in the short term follow up, in terms of a shorter hospital stay, reduction of VAS score, and ODI score. A comparative analysis of UBE with other minimally invasive procedures with a long-term follow-up will provide a better comparison of the outcomes of these surgical techniques.
CONCLUSION
UBE for the treatment of degenerative lumbar diseases is a safe, effective, and ergonomically comfortable surgical technique under a clear and wide endoscopic view. Segmental stability can be preserved since it allows over-the-top decompression easily without the removal of the spinous process & spinous ligaments. However, large-scale comparative studies will be needed to assess the difference in clinical outcomes and infection rates with other procedures.
Ethical approval
The research/study approved by the Institutional Review Board at Mahatma Gandhi Mission’s Medical College and Hospital, number MGM-ECRHS/2024/176, dated 27th June 2024.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Spine Update Lumbar Foraminal Stenosis. Spine (Phila Pa 1976). 2000;25:389-94.
- [CrossRef] [PubMed] [Google Scholar]
- Lumbar Stenosis: A Recent Update by Review of Literature. Asian Spine J. 2015;9:818-28.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Management of Degenerative Lumbar Spinal Stenosis: An Evidence-Based Review. EFORT Open Reviews. 2016;1:267-74.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Serial Changes in Trunk Muscle Performance After Posterior Lumbar Surgery. Spine (Phila Pa 1976). 1999;24:1023-8.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative Analysis of Three Types of minimally Invasive Decompressive Surgery for Lumbar Central Stenosis: Biportal Endoscopy, Uniportal Endoscopy, and Microsurgery. Neurosurg. Focus. 2019;46:E9.
- [CrossRef] [PubMed] [Google Scholar]
- The Role of Conservative Treatment in Lumbar Disc Herniations: WFNS Spine Committee Recommendations. World Neurosurg X. 2024;22:100277.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Herniated Discs: When is Surgery Necessary? EFORT Open Rev. 2021;6:526-30.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- International Society for the Advancement of Spine Surgery Policy 2019-Surgical Treatment of lumbar Disc Herniation with Radiculopathy. Int J Spine Surg. 2020;14:1-17.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical Outcomes of Uniportal and Biportal Lumbar Endoscopic Unilateral Laminotomy for Bilateral Decompression in Patients with Lumbar Spinal Stenosis: A Retrospective Pair-Matched Case-Control Study. World Neurosurg. 2022;161:e134-45.
- [CrossRef] [PubMed] [Google Scholar]
- Fully Endoscopic Lumbar Interbody Fusion Using a Percutaneous Unilateral Biportal Endoscopic Technique: Technical Note and Preliminary Clinical Results. Neurosurg. Focus. 2017;43:E8.
- [CrossRef] [PubMed] [Google Scholar]
- Can Percutaneous Biportal Endoscopic Surgery Achieve Enough Canal Decompression for degenerative Lumbar Stenosis? Prospective Case-Control Study. World Neurosurg. 2018;120:e684-9.
- [CrossRef] [PubMed] [Google Scholar]
- Extraforaminal Approach of Biportal Endoscopic Spinal Surgery: A new Endoscopic Technique for transforaminal Decompression and Discectomy. J Neurosurg Spine. 2018;28:492-8.
- [CrossRef] [PubMed] [Google Scholar]
- Preliminary Clinical and radiological Outcomes of the “No-Punch” decompression Techniques for Unilateral Biportal Endoscopic Spine Surgery. Neurospine. 2024;21:732-41.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Biportal Endoscopic Approach for lumbar Degenerative Disease in the Ambulatory Outpatient vs Inpatient Setting: A Comparative Study. Int J Spine Surg. 2023;17:858-65.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Biportal endoscopic Spine Surgery (BESS): Considering Merits and Pitfalls. J Spine Surg. 2020;6:457-65.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Unilateral Biportal Endoscopic Decompression for Degenerative Lumbar Canal Stenosis. J Spine Surg. 2020;6:438-46.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Advantages of New Endoscopic Unilateral Laminectomy for bilateral Decompression (ULBD) Over Conventional Microscopic ULBD. Clin Orthop Surg. 2020;12:330-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical and Radiological Outcomes Between Biportal Endoscopic Decompression and Microscopic Decompression in Lumbar Spinal Stenosis. J Orthop Sci. 2020;25:371-8.
- [CrossRef] [PubMed] [Google Scholar]
- Biportal Endoscopic Lumbar Decompression for Lumbar Disk Herniation and Spinal Canal Stenosis: A technical note. J Neurol Surg A Cent Eur Neurosurg. 2017;78:390-6.
- [CrossRef] [PubMed] [Google Scholar]
- Is Biportal Technique/Endoscopic Spinal Surgery Satisfactory for Lumbar Spinal Stenosis Patients?: A Prospective Randomized Comparative Study. Medicine (Baltimore). 2019;98:e15451.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Comparison of Lumbar Microdiscectomy and Unilateral Biportal Endoscopic Discectomy Outcomes: A Single-Center Experience. J Neurosurg Spine. 2024;40:351-8.
- [CrossRef] [PubMed] [Google Scholar]
- Unilateral Biportal Endoscopy Versus Tubular Microendoscopy in Management of Single Level Degenerative Lumbar Canal Stenosis: A Prospective Study. Clin Spine Surg. 2021;34:E323-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Water Dynamics in Unilateral Biportal Endoscopic Spine Surgery and its Related Factors: An in Vivo Proportional Regression and Proficiency-Matched Study. World Neurosurg. 2021;149:e836-43.
- [CrossRef] [PubMed] [Google Scholar]







