Translate this page into:
Effectiveness of Virtual Reality Environment for Post-Operative Pain Management

Corresponding author: Dr. Himavathy Kodandarao Gara, Department of Physiology, Gayatri Vidya Parishad Institute of Healthcare and Medical Technology, Marikavalsa, Visakhapatnam, India. snowgara2212@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Thippabathuni S, Chandra Dronamraju VA, Gara HK, Vanamali DR. Effectiveness of Virtual Reality Environment for Post-Operative Pain Management. Int J Recent Surg Med Sci. 2024;10:63-71. doi: 10.25259/IJRSMS_29_2023
Abstract
Objectives
The imperative need of post-operative period is effective pain management. Virtual reality (VR) causes psychological distraction from pain stimuli, and thus may cause pain alleviation. The study was undertaken to determine the effectiveness of VR distraction on post-operative pain and experience of VR sessions among the patients.
Material and Methods
A hospital-based interventional study was conducted for a period of two months with the objectives to estimate changes in post-operative pain intensity after VR session as well as to analyze experience related to VR interventions. It comprised patients of either gender undergoing surgery and with 1–3 days of hospitalization, who were randomized into two groups (age and gender matched). The control group was kept on standard post-operative pain management. The interventional group was subjected to VR exposure in addition to standard care therapy. The Numerical Rating Scale (NRS) scores were obtained twice post-operatively in subsequent days. I-group presence questionnaire (IPQ) responses were obtained after the VR session.
Results
Both control and interventional groups had 25 participants each for analysis. In both the groups, majority were given bupivacaine for anesthesia and combination of paracetamol and diclofenac for post-operative analgesia. The NRS scores of both groups obtained post-operatively on standard therapy without VR intervention did not show any significant difference. However, the post-VR-sessions’ NRS scores showed significant reduction as compared to pre-session scores among the participants of the interventional group. The responses obtained via IPQ revealed acceptance for the features of realism, engagement, and presence during VR intervention. Majority confirmed their willingness to undergo VR sessions in future.
Conclusion
VR session helped in significant reduction of pain perception as VR simulation diverted considerable attention away from the pain. Majority expressed positive inclination for utilization of VR in comprehensive patient care.
Keywords
Virtual reality
Post-operative pain
Numerical Rating Scale
I-group presence questionnaire
INTRODUCTION
As per International Association for the Study of Pain (IASP), pain is defined as ‘an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage’.[1] Medical or surgical procedures often induce pain and emotional distress for which suitable pharmacological approaches are employed for pain alleviation.[2] However, these pose the risk of adverse side effects, narrow therapeutic windows and the potential for drug misuse. A shift to newer and safer therapeutic modalities as an adjuvant for pain management is the need of the hour. In view of multidimensional nature of pain, non-pharmacological interventions might have scope for therapeutic potential in the growing epidemic of non-steroidal anti-inflammatory drugs (NSAID) and opioids prescriptions, as they allow manipulation of affective or attentional processes.[3]
The gold standard to assess the efficacy of pain management after surgery is the patient’s self-assessment of pain.[4] The characteristic of pain may influence the clinical and psychological outcomes. Hence, continual evaluation of pre- and post-operative pain shall help to deliver an effective patient care and achieve higher patient satisfaction. Variables such as age, coping skills, anxiety and depression may influence levels of post-operative pain.
Virtual reality (VR) has emerged as an effective non-pharmacological therapeutic modality for pain.[5] VR creates a sensation of a realistic 3D-world utilizing computer-generated images and sound, enabling the users to experience the total immersion in a virtual world. The technologically created virtual milieu with multisensory inputs like vision, audition, and proprioception demand more conscious attention by the cortical areas, which are likely to interfere mutually, resulting in less focus on nociceptive inputs.[6] Thus, VR acts as a positive distraction limiting the processing of nociceptive stimuli, eventually mitigating subjective pain experience.[3,7]
Inadequate pain relief remains a major healthcare dilemma despite the advent of multi-modal approaches and updates in clinical practice guidelines. It is often associated with extended hospitalization, increased morbidity and risk of progression into chronic pain.[8] Targeting physiological and emotional responses to pain shall enhance cognitive reconstruction and pain acceptance.
Objective
The aim of the study was to evaluate the efficacy of VR as an adjunct for post-operative pain management in patients undergoing surgical procedures.
-
Primary objective
To assess the effect of VR intervention on post-operative pain intensity compared to standard therapy alone as measured by Numerical Rating scale (NRS) scores.
-
Secondary objectives
To evaluate the level of presence and immersion experienced by participants during VR sessions using the I-group Presence Questionnaire (IPQ).
To determine the demographic characteristics of participants.
To examine the clinical course of participants, including the type of surgery, days of hospitalization, and details of pharmacotherapy for analgesia.
To estimate the adverse events and unintended events associated with VR-intervention.
MATERIAL AND METHODS
This was a hospital-based parallel-group randomized controlled study conducted for a period of 2 months from 1 August 2022 to 30 September 2022. The study was initiated after acquiring approval from the Institutional Ethical Committee reference no: GVPIHCMT/IEC/20220620/01 dated 20.06.2022. The study was performed according to the Declarations of Helsinki and Good Clinical practice requirements.
Patient recruitment and screening
The study participants were recruited from patients of either gender undergoing surgical procedures from the Department of Surgery and Obstetrics and Gynaecology. A comprehensive recruitment methodology was applied for the identification of eligible candidates for inclusion in the study. The attending physicians and medical staff identified the potential participants who matched the age and surgical criteria. The patients who expressed interest in participation were reviewed for their medical history, surgical procedure details, and general health condition to screen them for their eligibility based on the following inclusion criteria:
Age ≥18 years and ≤80 years
Hospital stay of 1–3 days following surgery.
Ability to understand and follow instructions.
The exclusion criteria were
VR-induced symptoms and effects (VRISE) during or after VR sessions.
Unable to cooperate completely for study procedure or complete the questionnaire.
Responded to less than 80% of the intervention (VR sessions).
Clinically unstable condition which could interfere with participation in the study.
Severe cognitive dysfunction that might impede the understanding of the study requirements.
Severe visual/hearing impairment that could affect the VR experience.
Patients with injuries or who underwent surgery for head, eye, ear, and neck region at time of enrolment for the study.
Refusal to participate.
Participant informed consent
Before enrolment, a written informed consent form was obtained from the participants in a non-coercive environment, assuring them confidentiality of the collected information. The eligible candidates were provided a detailed explanation of the study during the outpatient visit a day prior to surgery. The explanation comprised the purpose, methodology, potential benefits and potential risks of the study. The consent form also highlighted their right to withdraw from the study at any time without consequences.
Sample size calculation
The expected effect size of 0.49 was chosen for the sample size calculation based on the systemic review and meta-analysis of 20 studies by Chan and his colleagues.[9] They suggested Standard Mean Difference reduction in pain score with VR to be −0.49 (95% confidence interval −0.83 to −0.41, p = 0.006). Considering an effect size of 0.49, with α = 0.05 and power =0.80, the minimum sample size for the study was 50 participants with 25 participants in each group, calculated using G*power 3.1.9.7 software.
Randomization process
Randomization was employed to ensure unbiased distribution of participants into control and interventional groups. Allocation sequence was computer-generated to prevent selection bias. Due to the nature of the VR intervention, blinding the participants was not feasible.
The study had two groups:
Control group: Participants in this group received standard post-operative care, which included pharmacotherapy and routine pain management practices.
Interventional group: Participants in this group received VR-based intervention in addition to standard post-operative care.
Primary and secondary outcomes
The primary outcome measure was pain assessment using NRS. Secondary outcomes included evaluation of experience of VR session using IPQ and the willingness of participants to undergo further VR sessions using a dichotomous response.
Data collection
The selected patients as per Consolidated Standards of Reporting Trials (CONSORT) guidelines [Figure 1] were subjected to face-to-face interviews and clinical examination. The socio-demographic data included age, gender, marital status, educational qualification, medical history, drug history, family history and history of substance abuse. The clinical information included diagnosis, type, and name of surgery, type of anesthesia given, pharmacotherapy given and route of administration, and number of days of hospitalization.

- Flowchart of participants for the study as per CONSORT guidelines showing recruitment and progress of the study VRISE: VR-induced symptoms and effects. Control group: receiving standard care post-operatively. Interventional group: receiving VR-based intervention in addition to standard care treatment post-operatively; VR: Virtual reality; CONSORT: Consolidated Standards of Reporting Trials; n: number of participants.
VR intervention
Each session constituted 15 minutes’ exposure to immersive virtual environment. The VR immersion was achieved with the use of VR headset (Procus Pro, compatible with all smartphones) as shown in Figure 2. The headset had inbuilt headphones for immersive wholesome sound experience. It had provision for focal length adjustment and high-quality lenses providing 100–120 degree field of vision.
The first session was given pre-operatively a day prior to surgery for the patient to get introduced to VR sessions and address any queries. On the day of surgery, in the recovery room, the anesthetic doctor assessed the patient for recovery from anesthetic in terms of regain of consciousness, recovery of protective airway reflexes, and resumption of motor activity. After about 60–90 minutes, when the patient regained his/her coordination of activities and intellectual function and was hemodynamically stable, he/she was shifted to the ward. The patient was subjected to a second VR session approximately 4–6 hours post-operatively. The third session was on the next consecutive day.
The patient was instructed to lie comfortably on the bed and fitted with the VR headset as shown in Figure 2. He/she was asked to select a VR programme of nature scenes with guided relaxation, adjusted to his/her preferences and needs. He/she was encouraged to explore the VR environment, interact with the elements and focus on the sensations and emotions. Simultaneously continuous monitoring was done to look for VRISE or unintended effects under supervision of an attending physician/nurse. At the end of the session, the patients were gently brought back to reality and asked to rate their pain level based on NRS. They were also administered IPQ questionnaire at the end of the VR sessions to evaluate their experience and satisfaction with the VR exposure.
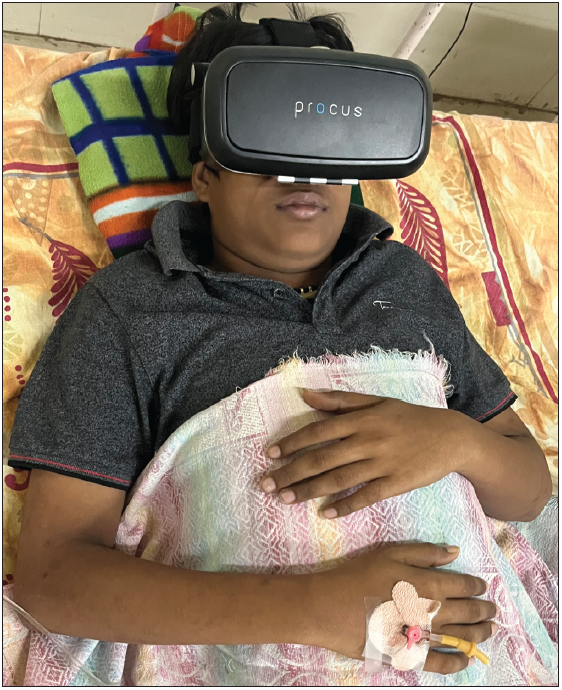
- VR session of study participant with VR headset; VR: Virtual reality.
Adverse events and unintended effects
Patients were monitored for any adverse event related to VR intervention and the findings were recorded. The major concern with utilization of VR systems in clinical settings was VRISE, e.g., presence of nausea, headache, dizziness, instability, fatigue or disorientation. This indicated the safety of VR intervention in the study protocol.
NRS
This pain score was administered verbally by asking the patients to report the intensity before and after VR session on a scale, wherein ‘0’= no pain, ‘5’ = moderate pain, and ‘10’ = extremely painful.[10,11] In the control group, NRS scores were obtained after their pharmacological therapy. In the interventional group, NRS scores were obtained pre- and post-VR session. The NRS scores were obtained twice post-operatively on subsequent days. The changes from the baseline within groups and final values between the groups were assessed.
IPQ
IPQ is a 14-item questionnaire to evaluate the different aspects of the presence and immersion into the VR world. The assessment was driven by three latent variables, namely, spatial presence, involvement and realism. IPQ was administered to patients after the third VR session.[12] After the completion of IPQ, an additional question with dichotomous response regarding willingness to undergo further VR sessions was also asked.
Data analysis
The collected data were organized into the Microsoft excel sheet. The data were subjected to statistical analysis with the help of Statistical Package for Social Sciences (SPSS) version-24. The categorical data were expressed as frequency (n) and percentages (%) and were analyzed by Chi-square test and Fisher’s exact test, depending upon the nature of data distribution. The descriptive data were computed into mean and standard deviation. The differences between the control and the cases were analyzed with the help of a two-tailed unpaired ‘t’ test. The differences in NRS scores of the interventional group obtained pre- and post-VR sessions were analyzed using a dependent ‘t’ test. The p-value of 0.05 was adopted for statistical significance for all analyses.
RESULTS
A total of 63 patients who were supposed to undergo surgery were enrolled for the study after taking into consideration the inclusion and exclusion criteria. However, seven patients were excluded due to the reasons cited in Figure 1. A total of 56 patients were assigned into two groups, namely, the control group (standard therapy) and the interventional group (standard therapy + VR), using block randomization method, with 28 patients in each group. In the control group, three patients were excluded as their hospitalization extended beyond three days. In the interventional group, three patients were excluded as they reported VRISE during the VR session. Hence, the data analysis for both groups was limited to 25 patients each [Figure 1].
The mean age of the participants in the control and intervention groups were 36.24 ± 13.01 and 39.56 ± 14.27 years, respectively, with no statistical difference [Table 1]. There was no statistical variation noted regarding gender. Hence, both the control and interventional groups were age and gender-matched.
| Variable | Controls (n = 25) n (%) | Cases (n = 25) n (%) | p-value |
|---|---|---|---|
| Age (in years) | 36.24 ±13.01 | 39.56 ± 14.27 | 0.3943 |
| Gender: | |||
| Male | 9 (36) | 14 (56) | 0.2563 |
| Female | 16 (64) | 11 (44) | |
| Marital status: | |||
| Single | 4 (16) | 5 (20) | 1 |
| Married | 21 (84) | 20 (80) | |
| Staying with: | |||
| Alone | 1 (4) | 1 (4) | 1 |
| Family | 24 (96) | 24 (96) | |
| Educational qualification: | |||
| Schooling | 11 (44) | 8 (40) | 0.3587 |
| Intermediate | 9 (36) | 11 (44) | |
| Graduate | 5 (20) | 4 (16) | |
| Occupation: | |||
| Unemployed | 6 (24) | 8 (32) | 0.824 |
| Skilled agricultural and fishery workers | 7 (28) | 9 (36) | |
| Clerks | 4 (16) | 2 (8) | |
| Technicians and associate professionals | 3 (12) | 2 (8) | |
| Professionals: Legislators, senior officials and managers | 5 (20) | 4 (16) | |
| Consumption of: | |||
| Alcohol | 5 (20) | 0 | - |
| Smoking | 5 (20) | 0 | |
| Drugs | 0 | 0 | |
n: number of participants.
In the control group and the interventional group, 28% (n = 7) and 72% (n = 18) patients underwent laparoscopic and open surgery, respectively [Table 2]. The average duration of hospitalization in the control and interventional groups was 2.84 ± 0.37 and 2.6 ± 0.645, days, respectively, with no statistical difference. The combination of paracetamol with diclofenac was highest prescribed in both groups for post-operative analgesia with no significant differences. The interventional group had lesser need for rescue analgesic drugs post-operatively as compared to the control group, but it was not statistically significant.
| Variable | Controls (n = 25) n (%) | Cases (n = 25) n (%) | p-value |
|---|---|---|---|
| Department: | |||
| Obstetrics and gynecology | 15 (60) | 8 (32) | |
| Surgery | 10 (40) | 17 (68) | 0.5512 |
| Type of surgery | |||
| Laparoscopy | 7 (28) | 7 (28) | 1 |
| Open | 18 (72) | 18 (72) | |
| Days of Hospitalization | |||
| 2 days | 5 (20) | 8 (32) | 0.333 |
| 3 days | 20 (80) | 17 (68) | |
| Average duration of hospitalization (in days): | 2.84 ± 0.37 | 2.6 ± 0.645 | 0.1131 |
| Pharmacotherapy for analgesia: | |||
| Paracetamol | 7 (28) | 3 (12) | 0.488 |
| Paracetamol + tramadol | 5 (25) | 4 (16) | |
| Paracetamol + tramadol + diclofenac | 1 (4) | 1 (4) | |
| Paracetamol + diclofenac | 10 (40) | 16 (64) | |
| Tramadol + diclofenac | 2 (8) | 1 (4) | |
| Rescue analgesia | |||
| Total received | 17 (68) | 10 (40) | 0.0877 |
| Paracetamol | 7 (28) | 4 (16) | |
| Tramadol | 5 (20) | 2 (8) | |
| Diclofenac | 5 (20) | 3 (12) | |
Bupivacaine was the most preferred drug for anesthesia in both groups followed by ropivacaine [Table 3]. The preferred route of administration was spinal. In both the control as shown in Table 4 group utilization and the interventional group as shown in Table 5, paracetamol was the highest prescribed drug followed by diclofenac for post-operative pain management.
| Anesthetic Drug | Average dose (in mg) | Route | Number of patients [n (%)] |
|---|---|---|---|
| Control group | |||
| Bupivacaine | 11.9 ± 3.06 | Spinal | 20 (80) |
| Ropivacaine | 22.25 ± 1.658 | Spinal | 4 (16) |
| Propofol | 100 | Intravenous | 1 (4) |
| Interventional group | |||
| Bupivacaine | 14.28 ± 3.144 | Spinal | 18 (72) |
| Ropivacaine | 19.025 ± 4.71 | Spinal | 4 (16) |
| Propofol | 86.67 ± 23.09 | Intravenous | 3 (12) |
| Drug | Average dose (in mg) | Average duration (in days) | Number of patients | Frequency of administration in a day |
|---|---|---|---|---|
| Paracetamol | ||||
| Oral | 2133.33 ± 1570.11 | 2 ± 1 | 2 | 2.5 ± 0.70 |
| IV bolus | 3500 ± 921.32 | 1.5 ± 0.70 | 3 | 3 |
| IV infusion | 2687 ± 115 | 2.3 ± 0.70 | 17 | 3 |
| Intramuscular | 450 | 1 | 1 | 1 |
| Tramadol | ||||
| Oral | 600 | 3 | 1 | 2 |
| IV bolus | 300 | 3 | 2 | 1 |
| IV infusion | 300 | 1 | 1 | 3 |
| Intramuscular | 116.67 ± 68.31 | 1.67 ± 0.516 | 4 | 1.25 ± 0.5 |
| Diclofenac | ||||
| Intramuscular | 703.84 ± 262.56 | 2.84 ± 0.375 | 13 | 2 |
n: number of participants.
| Drug | Average dose (in mg) | Average duration (in days) | Number of patients | Frequency of administration in a day |
|---|---|---|---|---|
| Paracetamol | ||||
| Oral | 2435.71 ± 1228.38 | 2.28 ±0.487 | 19 | 2.285 ± 0.48 |
| IV infusion | 3044.44 ±1078.23 | 2.33 ± 0.707 | 20 | 2.78 ± 0.44 |
| Tramadol | ||||
| IV bolus | 166.67 ± 57.73 | 1.33 ± 0.57 | 2 | 2 |
| Intramuscular | 200 | 2 | 4 | 2 |
| Diclofenac | ||||
| Oral | 600 ± 122.47 | 3.33 ± 1.24 | 3 | 2 |
| Intramuscular | 510 ± 194.75 | 1.8 ± 0.56 | 15 | 1.72 ± 0.460 |
n: number of participants.
The NRS scores in the control and interventional groups during standard post-operative analgesic therapy were not statistically significant (p = 0.3277) [Table 6]. After the VR intervention, the NRS scores on day 1 and day 2 were 6.36 ± 0.95 and 4.2 ± 0.577, respectively [Table 7]. The scores in the interventional group after the VR session were statistically significantly lower as compared to before the VR session (p < 0.001), thus reflecting reduction in pain perception after the VR session. Regarding the experience about the VR session via IPQ, the majority responded positively to the VR experiences, feeling the presence of virtual world, with the virtual world seeming real [Table 8]. For the dichotomous question regarding willingness to undergo VR sessions in hospital care, 80% of the patients gave a positive response.
| Post-operative day | Controls (n = 25) | Interventional group (n = 25) | p-value* |
|---|---|---|---|
| Day 1 | 7.6 ± 0.866 | 7.84 ± 0.85 | 0.3277 |
| Day 2 | 6.2 ± 0.75 | 6.04 ± 0.611 | 0.4123 |
NRS: Numerical rating scale, VR: virtual reality, *p-value < 0.05 – statistically significant.
| Post-operative day | Pre-VR intervention NRS score | Post-VR intervention NRS score | p-value |
|---|---|---|---|
| Day 1 | 7.84 ± 0.85 | 6.36 ± 0.95 | 0.000115* |
| Day 2 | 6.04 ± 0.611 | 4.2 ± 0.577 | <0.001* |
NRS: Numerical rating scale, VR: virtual reality, *p-value < 0.05 – statistically significant.
| Q. | Questions | –3 n (%) | –2 n (%) | –1 n (%) | 0 n (%) | 1 n (%) | 2 n (%) | 3 n (%) |
|---|---|---|---|---|---|---|---|---|
| 1 | How aware were you of the real world surrounding you while navigating in the virtual world? (i.e., sounds, room temperature, other people, etc.)? | 0 | 0 | 0 | 1 (4) | 24 (96) | 0 | 0 |
| 2 | How real did the virtual world seem to you? | 0 | 0 | 4 (16) | 1 (4) | 20 (80) | 0 | 0 |
| 3 | I had a sense of acting in the virtual space, rather than operating something from outside. | 0 | 0 | 3 (12) | 15 (60) | 7 (28) | 0 | 0 |
| 4 | How much did your experience in the virtual environment seem consistent with your real-world experience? | 0 | 0 | 0 | 5 (20) | 20 (80) | 0 | 0 |
| 5 | How real did the virtual world seem to you? | 0 | 0 | 6 (24) | 6 (24) | 13 (52) | 0 | 0 |
| 6 | I did not feel present in the virtual space. | 0 | 0 | 8 (32) | 11 (44) | 6 (24) | 0 | 0 |
| 7 | I was not aware of my real environment. | 0 | 0 | 0 | 1 (4) | 18 (72) | 6 (24) | 0 |
| 8 | In the computer-generated world, I had a sense of ‘being there’. | 0 | 0 | 0 | 0 | 21 (84) | 4 (16) | 0 |
| 9 | Somehow, I felt that the virtual world surrounded me. | 0 | 0 | 0 | 0 | 22 (88) | 3 (12) | 0 |
| 10 | I felt present in the virtual space. | 0 | 0 | 5 (20) | 13 (52) | 7 (28) | 0 | 0 |
| 11 | I still paid attention to the real environment. | 0 | 0 | 1 (4) | 5 (20) | 19 (76) | 0 | 0 |
| 12 | The virtual world seemed more realistic than the real world. | 0 | 0 | 6 (24) | 9 (36) | 10 (40) | 0 | 0 |
| 13 | I felt like I was just perceiving pictures. | 0 | 0 | 4 (16) | 15 (60) | 6 (24) | 0 | 0 |
| 14 | I was completely captivated by the virtual world. | 0 | 0 | 0 | 6 (24) | 13 (52) | 6 (24) | 0 |
IPQ - I-group Presence Questionnaire; n: number of participants.
DISCUSSION
Each patient has his/her unique perception of pain which permits the utilization of a combination of interventions for pain alleviation. Effective management of post-operative pain is considered as the essential and humanitarian requirement of every surgical event.[13] Post-operative pain management is critical due to its pervasive nature and multi-dimensional components. This has led to the escalation of analgesics prescriptions with the risk of side-effects and addiction. Uncontrolled pain or inadequate pain relief often results in patient’s dissatisfaction.[8]
In the present study, bupivacaine was the preferred anesthetic drug for surgery given in both groups. After the administration of bupivacaine, pain is the first sensation to be lost. It has prolonged anesthetic action with better sensory than motor block.[14] The present study also revealed that the combination of paracetamol with diclofenac (NSAID) was the preferred pharmacotherapy for post-operative analgesia among both groups. Ong CKS and his colleagues in their qualitative systematic review of 21 studies highlighted that the combination of NSAIDs with paracetamol showed better improvement in pain relief as compared to the drugs when used alone.[15] In the post-operative period, the patient is kept nil by mouth that limits its oral usage. Availability of the IV form of paracetamol and its better safety profile has led to increased use of paracetamol in post-operative analgesia.[16]
In the present study, NRS was used to assess the pain perception in the post-operative phase. The NRS scores, when both groups were on standard pharmacological analgesic therapy, did not show any statistically significant difference. However, after exposure to the VR session in the interventional group, the post-session NRS scores were statistically significantly lower as compared to the pre-session scores. Thus, it could be concluded that the VR intervention caused substantial reduction in pain perception. The findings were consistent with the studies by Payne O et al.,[17] Karaveli CS et al.,[18] Jie D et al.[19] and McSherry T et al.[20] All the studies have shown a promising potential of VR interventions to redefine non-pharmacological intervention for acute pain services. Higher patient load with limited medical personnel and resources highlights the need for co-existing, user-friendly adjuncts to the standard pharmacological therapy. VR can offer great benefit, especially in the case of children, elderly and obese patients where pain dynamics are unpredictable, and risk of side-effects is higher.[21–24]
In the present study, three patients showed VRISE during VR sessions, namely, nausea and headache, hence VR sessions were terminated in those patients. Hence, it is essential to watch for VRISE for safer implication of VR in clinical practice.[25] The possibility of VRISE during any session depends on VR head-mounted display, sound, navigation, ergonomic interaction and user experience. A technological review and meta-analysis of 44 neuroscientific or neuropsychological studies had highlighted the role of technology competency and implementation along with health and safety standards to reduce adverse symptomatology and dropouts.[26]
In the present study, IQP was used in the interventional group to estimate the feasibility and satisfaction of the VR session. Majority of the participants confirmed that the virtual world seemed real, and they were unaware of the real environment. Majority felt captivated by the VR session and reported lower NRS scores after a VR session. VR interfered with pain perception as the audio-visual inputs provided adequate distraction from pain, thus reducing pain perception.[7] Hospitalized patients often experience isolation, anxiety, boredom and emotional stress, which can exacerbate their pain perception.[8] Hence, clinicians should not only rely on physical outcomes but also consider psychosocial endpoints during pain management.
In the present study, 80% of the patients confirmed their willingness to undergo VR sessions as part of hospital care. The findings are similar to the study by McSherry T et al., in which 75% of participants showed willingness to use immersive VR session during wound dressing procedures.[20] Lesser pain perception shall motivate the patient to adhere to treatment protocols in the post-operative period. It is especially important in cases where mobilization is required to reduce post-operative complications. Better patient satisfaction and better functional status shall lead to shorter hospital stay and reduced hospital expenditure. A similar finding was observed in a study by Cacau LA et al., in which VR was used for post-operative rehabilitation of 60 patients with cardiac surgeries.[27]
The routine post-operative pain relief embraces the clock regimen of opioid or non-opioid analgesics.[3] Transforming the post-operative pain-care from the analgesics domain to a comprehensive model requires collaborative efforts. With the advent of safer technologically driven modalities, VR has the potential to open the door against the escalating analgesics prescription that carries the risk of side-effects and drug dependency. VR has good prospects to change dynamics in pain management with respect to change in preferences and demands in health care, especially pain services.
Limitation of the study
Recruiting participants from one single hospital has the possibility of affecting the external validity of the study and hence its implementation in the general population. There was a risk of personal bias as the measurement of pain perception and evaluation of VR experience were subjective end-points and could be influenced by personality traits. Also, NRS had the risk of the ceiling effect if the patient had scored 10 for pain intensity.[11] However, none of our patients gave the score of 10. Pain perception was driven by the NRS score and functional limitation or psychosocial factors were not taken into account.
CONCLUSION
In the present study, the combination of paracetamol and diclofenac (NSAID) was the highest prescribed for post-operative analgesia to both groups. In the interventional group, the NRS scores showed a significant reduction after the VR session as compared to the pre-session scores. Also, majority of patients expressed their satisfaction in the VR session in terms of its relation and engagement. Majority expressed their willingness to undergo VR sessions in future. Thus, VR confers a clinical window for pain alleviation in post-operative patients.
Acknowledgement
The present study was undertaken as the ICMR short-term studentship project in the year 2022, Reference no: 2022-08454.
We express our heartfelt gratitude to the participants who displayed immense interest and co-operation during the study. We are also thankful to the Department of Surgery, Department of Obstetrics and Gynaecology, Department of Anaesthesia, and the nursing staff who extended their support for patient selection and completion of the study.
Ethical approval
The study was initiated after acquiring approval from the Institutional Ethical Committee reference no: GVPIHCMT/IEC/20220620/01 dated 20.06.2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
REFERENCES
- The Revised International Association for the Study of Pain Definition of Pain: Concepts, Challenges, and Compromises. Pain. 2020;161:1976-82.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical Aspects of Acute Post-Operative Pain Management & its Assessment. J Adv Pharm Technol Res. 2010;1:97-108.
- [PubMed] [PubMed Central] [Google Scholar]
- Using Virtual Reality Distraction During Wound Management: A Brief Case Report in a Patient with Epidermolysis Bullosa. Pediatric Pain Letter. 2022;24:1-7.
- [Google Scholar]
- European Palliative Care Research Collaborative (EPCRC). Studies Comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for Assessment of Pain Intensity in Adults: A Systematic Literature Review. J Pain Symptom Manage. 2011;41:1073-93.
- [CrossRef] [PubMed] [Google Scholar]
- Virtual Reality as a Non-Pharmacological Adjunct to Reduce the Use of Analgesics in Hospitals. J Cogn Enhanc 2021:1-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Virtual Reality Interventions for Acute and Chronic Pain Management. Int J Biochem Cell Biol. 2019;114:105568.
- [CrossRef] [PubMed] [Google Scholar]
- Virtual Reality Assisted Non-Pharmacological Treatments in Chronic Pain Management: A Systematic Review and Quantitative Meta-Analysis. Int J Environ Res Public Health. 2022;19:4071.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Consequences of Inadequate Postoperative Pain Relief and Chronic Persistent Postoperative Pain. Anesthesiol Clin North Am. 2005;23:21-36.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Efficacy of Virtual Reality for Acute Procedural Pain Management: A Systematic Review and Meta-Analysis. PLoS One 2018:e0200987.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pain Measurement in the Elderly: A Review. Pain Manag Nurs. 2001;2:38-46.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Importance of Changes in Chronic Pain Intensity Measured on an 11-Point Numerical Pain Rating Scale. Pain. 2001;94:149-58.
- [CrossRef] [PubMed] [Google Scholar]
- I-Group Presence Questionnaire: Psychometrically Revised English Version. Mugla J Sci Tech. 2021;7:1-10.
- [Google Scholar]
- Pain Management: A Fundamental Human Right. Anesth Analg. 2007;105:205-21.
- [CrossRef] [PubMed] [Google Scholar]
- Local Anesthetic Systemic Toxicity: Reviewing Updates from the American Society of Regional Anesthesia and Pain Medicine Practice Advisory. J Perianesth Nurs. 2018;33:1000-5.
- [CrossRef] [PubMed] [Google Scholar]
- Combining Paracetamol (Acetaminophen) with Nonsteroidal Antiinflammatory Drugs: A Qualitative Systematic Review of Analgesic Efficacy for Acute Postoperative Pain. Anesth Analg. 2010;110:1170-9.
- [CrossRef] [PubMed] [Google Scholar]
- Single Dose Oral Paracetamol (Acetaminophen) for Postoperative Pain in Adults. Cochrane Database Syst Rev 2008:CD004602.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Virtual Reality and its Use in Post-Operative Pain Following Laparoscopy: A Feasibility Study. Sci Rep. 2022;12:13137.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The Effect of Virtual Reality on Pain and Anxiety During Colonoscopy: A Randomized Controlled Trial. Turk J Gastroenterol. 2021;32:451-7.
- [PubMed] [Google Scholar]
- Virtual Reality Distraction Decreases Pain During Daily Dressing Changes Following Haemorrhoid Surgery. J Int Med Res. 2019;47:4380-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Randomized, Crossover Study of Immersive Virtual Reality to Decrease Opioid Use During Painful Wound Care Procedures in Adults. J Burn Care Res. 2018;39:278-85.
- [CrossRef] [PubMed] [Google Scholar]
- Postoperative Pain Management of the Obese Patient. Best Pract Res Clin Anaesthesiol. 2011;25:73-81.
- [CrossRef] [PubMed] [Google Scholar]
- Managementul Durerii Postoperatorii La Pacientul Vârstnic [Postoperative Pain Management in Elderly Patient] Rev Med Chir Soc Med Nat Iasi. 2007;111:135-43.
- [PubMed] [Google Scholar]
- Guided Relaxation-Based Virtual Reality for Acute Postoperative Pain and Anxiety in a Pediatric Population: Pilot Observational Study. J Med Internet Res. 2021;23:e26328.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Use of Virtual Reality in Managing Paediatric Procedural Pain and Anxiety: An Integrative Literature Review. J Clin Nurs. 2022;31:3032-59.
- [CrossRef] [PubMed] [Google Scholar]
- Health and Safety Implications of Virtual Reality: A Review of Empirical Evidence. Appl Ergon. 2002;33:251-71.
- [CrossRef] [PubMed] [Google Scholar]
- Technological Competence is a Pre-Condition for Effective Implementation of Virtual Reality Head Mounted Displays in Human Neuroscience: A Technological Review and Meta-Analysis. Front Hum Neurosci. 2019;13:342.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The Use of the Virtual Reality as Intervention Tool in the Postoperative of Cardiac Surgery. Rev Bras Cir Cardiovasc. 2013;28:281-9.
- [CrossRef] [PubMed] [Google Scholar]








