Translate this page into:
Idiopathic Calcinosis Cutis of Hip: A Case Report and Review of Literature
*Corresponding author: Gauri Jadhav, DNB, Department of Surgery, Dr. Hedgewar Hospital, Aurangabad, Maharashtra, India. gaurisj27@gmail.com
Abstract
Calcinosis cutis is an uncommon disorder identified by the deposition of calcium in the skin and subcutaneous tissue. Idiopathic variety of calcinosis cutis is the one with no underlying damage at the tissue level or an absence of systemic derangement in the calcium and phosphorus metabolism. Here, we report a case of a 65-year-old female diagnosed with idiopathic calcinosis cutis of the hip after her calcium and phosphorus levels were found to be normal and no connective tissue disorder could be identified.
Keywords
Calcinosis cutis
Idiopathic calcinosis cutis
Subepidermal calcium nodule
Introduction
Physiological calcium stores are found in the bones and teeth of the human body in the form of calcium hydroxyapatite. In its ionized form, calcium plays a very important role in muscular contractility, vascular constriction/dilatation, clotting of blood, and transmission of nerve signals.[1] Initially described by Virchow in 1885, calcinosis cutis is a pathognomic condition with abnormal calcium deposition in the skin and subcutaneous tissue. Clinically, the lesion presents as single or multiple hard nodules under the skin, mostly painless. The nodules may grow in size with duration or may even become painful to an extent of functional impairment.
Hypercalcemia, hyperphosphatemia, connective tissue disorders, autoimmune diseases, a traumatic or inflammatory insult to the tissues, and tumors have all been attributed as a cause of calcinosis. CREST (calcinosis, Raynaud phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia) syndrome and systemic sclerosis are specifically associated with calcinosis cutis. Pathophysiological classification of calcinosis cutis includes five types—dystrophic, metastatic, iatrogenic, idiopathic, and calciphylaxis.[2–4] The rarest subtype among these is idiopathic calcinosis cutis which is of unknown cause with no demonstrable local tissue damage or proven metabolic disorder of calcium.[5]
Very few cases of unilateral idiopathic calcinosis cutis are reported in previous literature. This case is an interesting one with the presentation of a single calcinosis cutis lesion over the left hip.
Case Report
A 65-year-old female came to our surgery clinic with a chief complaint of swelling over the left hip for 1 year. The patient was apparently well 1 year back when she observed a small swelling over her left hip. As per the patient’s description, the swelling was initially of the size of a “peanut,” which progressed gradually over time to attain the size of a “lemon” and caused cosmetic concern that made the patient visit the hospital. The swelling was painless and not associated with local erythema or warmth. There was no history of fever, malaise, and weight loss. The patient had no discomfort or restriction while walking at the level of the left hip joint. Bowel and bladder habits were normal. There was no history of systemic illness, trauma, or previous surgery. Family history was not significant.
On examination, a spherical swelling of size 4 cm × 3 cm × 2 cm approximately was noted over the greater trochanter of the left hip [Figure 1]. The swelling was hard and nodular in consistency, nontender on touch with no local rise of temperature, and non-transilluminating. The swelling was freely mobile in all directions suggestive of nonfixity to the underlying bone, with no overlying skin changes. No similar swelling was observed on other parts of the body. Systemic examination was within the normal limits. X-ray of the left hip joint was suggestive of a well-defined area of calcification lying over the greater trochanter of the left hip without underlying bony involvement [Figure 2]. A diagnosis of calcinosis cutis was considered. Routine blood investigations revealed complete blood count, renal, and liver function tests were within normal limits. Total calcium and ionic calcium values were 9.2 and 4.8 mg/dL, respectively. Parathyroid hormone and vitamin D levels were 32 pg/mL and 73 ng/mL, respectively. An immunological workup was done to evaluate coexisting connective tissue disorder. Antinuclear antibodies (ANA), anti-double stranded deoxyribonucleic acid (dsDNA), ribonucleoprotein antibody, SS-A, SS-B, anti-Sm antibody, and complement C3/C4 were all found to be within normal range. Thyroid profile was within normal limits.

- Swelling over the left hip on inspection as indicated by arrow.
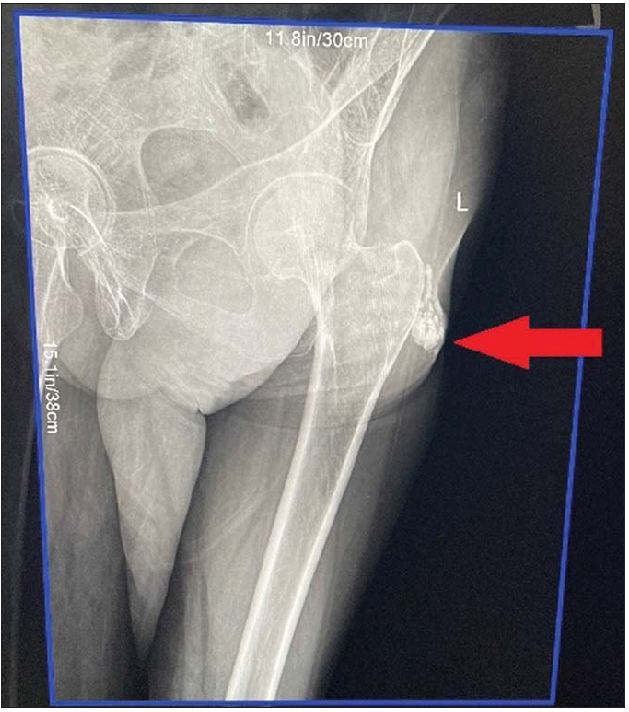
- X-ray left hip joint showing calcified lesion (arrow) over the left greater trochanter.
The patient was posted for surgical excision of the lesion under local anesthesia on a day care basis. Intraoperative findings revealed small, granular, subcuticular deposits of calcium with a dumbbell-shaped lesion of size 4 × 3 × 1.5 cm in the subcutaneous plane [Figure 3]. The lesion was excised in toto and sent for histopathological examination (HPE). The patient recovered well and sutures were removed on the 10th postoperative day. The HPE report was suggestive of extensive calcification with deposition of basophilic acellular material surrounded by fibrofatty tissue; findings consistent with calcinosis cutis [Figure 4].
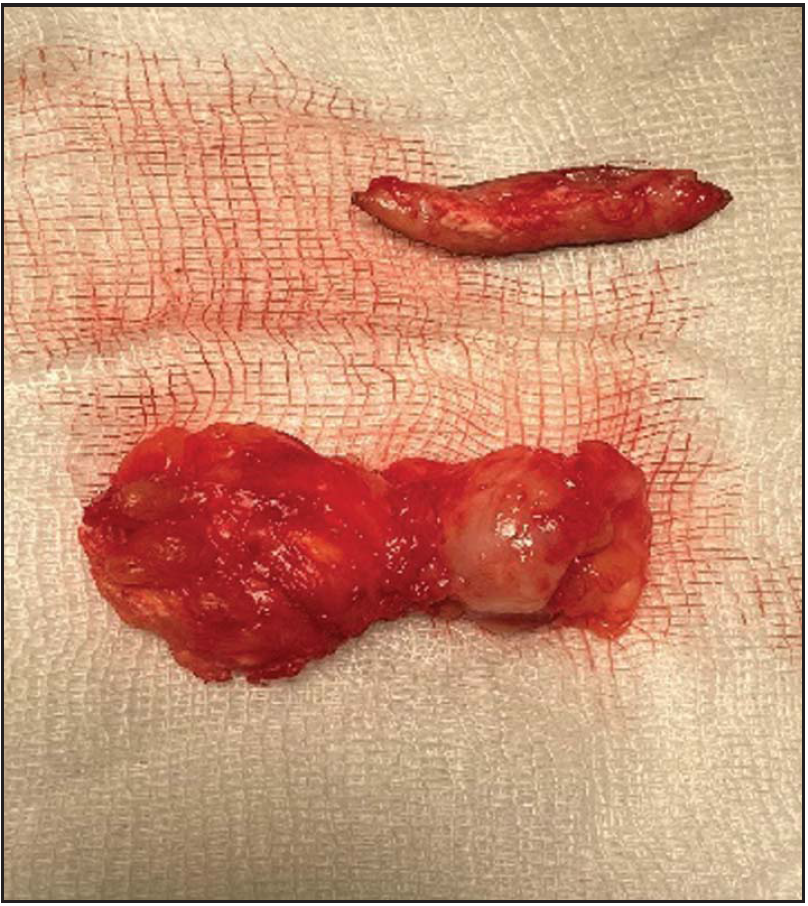
- Dumbbell-shaped specimen excised in toto.
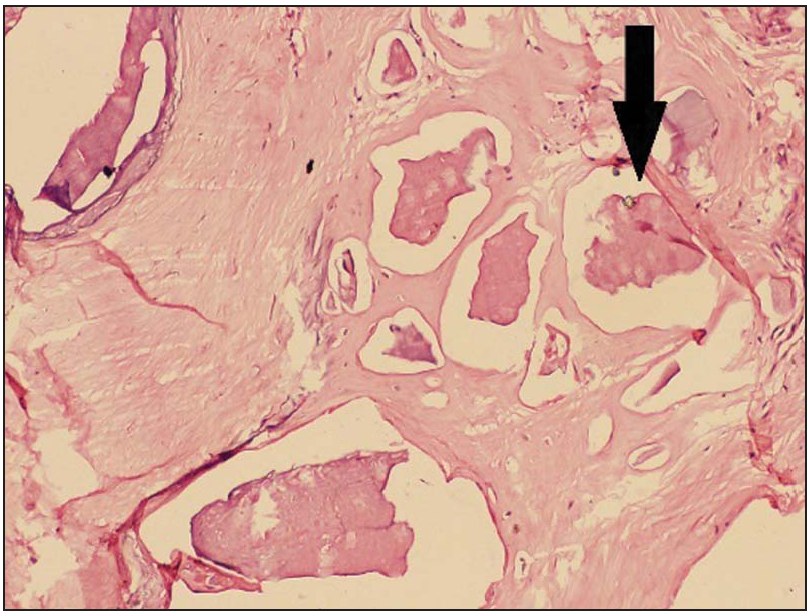
- Histopathological slide showing calcium deposits indicated by black arrow.
Discussion
Idiopathic calcinosis can be better considered as a diagnosis of exclusion when calcium or phosphorous levels are normal and no underlying tissue damage is detected. Increased uptake of phosphate ions by the kidneys is related to the familial tumoral calcinosis form. Subepidermal nodular forms are a subtype seen on the head and extremities as single, hard, white nodules.[3] Idiopathic scrotal calcinosis and tumoral calcinosis are other forms that have been reported in the literature. As per the findings and investigations, we categorize this case into an idiopathic subepidermal nodular variety.
Etiological classification of the calcinosis cutis includes four major variants: dystrophic, metastatic, iatrogenic, and idiopathic. Dystrophic calcium deposits are usually due to an inflammatory process secondary to an infection, skin neoplasm, or an underlying connective tissue disorder like systemic sclerosis, dermatomyositis, etc.[6] It is the most common type of calcinosis cutis associated with increased levels of phosphate-binding proteins that are released into blood circulation by the damaged tissues, which in turn binds with the phosphate causing calcium crystals formation. The dystrophic deposits are commonly seen at knees, elbows, forearms, and fingers; or they may also be localized around the underlying tissue damage.
Metastatic calcinosis cutis, as the name suggests, is due to abnormally high levels of calcium and phosphorous in the blood. Chronic renal failure is the most common cause of metastatic calcium deposits. Other causes include excessive dietary calcium intake, hyperparathyroidism, hypervitaminosis D, and malignant neoplasms. In most cases, the condition remains treatable with correction of serum calcium and phosphorous levels. The deposits are usually located around joints, that is, periarticular regions.[7]
Unmonitored and undiluted calcium supplementation with intravenous calcium gluconate or calcium chloride in the hospital settings may lead to extravasation of calcium salt into subcutaneous or cutaneous tissue causing iatrogenic calcinosis cutis. It is also seen in posttransplant cases or in conditions like tumor lysis syndrome.[8] The deposits may be clinically observed in proximity with the venipuncture sites.
A detailed metabolic workup may be necessary to identify the underlying cause. Serum calcium and phosphorus levels are done to rule out metastatic variety. Parathyroid, vitamin D, and 24-hour urinary calcium levels may aid in the diagnosis. Renal function tests (serum creatinine and urea) can be done to establish an underlying renal pathology such as chronic kidney disease. ANA, anti-dsDNA, and anti-extractable nuclear antigen estimation are done in cases of systemic sclerosis and lupus.[9] Increased levels of calcium are associated as paraneoplastic syndromes with various cancers such as multiple myeloma, breast cancer, squamous cell cancer of the lung, etc. Serum calcium levels of more than 14 mg/dL are considered severe and may require aggressive therapy in view of exaggerated clinical signs.[10]
Generalized presentation of calcinosis cutis requires medical treatment. Various modalities have been tried before with variable success. Diltiazem 2 mg/kg/day is the most common drug used in the treatment of calcinosis cutis. It acts by blocking the entry of calcium into the damaged tissues. Bisphosphonate derivatives such as zoledronate, pamidronate, etc. are useful in conditions like dermatomyositis and systemic sclerosis. They reduce calcium resorption and turnover thereby preventing the formation of calcium deposits. They also help in preventing the release of inflammatory cytokines. However, they usually demand long-term use and paradoxical hyperphosphatemia is a well-documented complication.[11] Other options include warfarin, antibiotics such as ceftriaxone and minocycline, intravenous immunoglobulins, and topical sodium thiosulfate but they have shown limited success.[3,12] Antacid preparations containing aluminum hydroxide acts by binding excessive phosphate in patients with hyperphosphatemia, however their use in cases of renal impairment is contraindicated.[13] In cases of a small and localized lesion, a surgical excision is a good option. In this particular case, our patient herself requested a surgical intervention for cosmetic reasons, hence medical therapy was not tried.
Conclusion
To conclude, this case report aims at underlying the importance of a thorough evaluation to rule out abnormalities of calcium and phosphate metabolism, presence of connective tissue disorders, malignancy, or renal impairment. Though the role of medical management is limited in idiopathic calcinosis cutis, the possibility of correctable/secondary causes should be sought in patients presenting with abnormal soft tissue calcification. Surgical excision is sufficient in cases with single and localized lesions.
Conflict of interest
None declared.
References
- Encyclopedia of Dietary Supplements (2nd ed.). Boca Raton, FL: CRC Press; 2015.
- Calcinosis cutis: part I. Diagnostic pathway. J Am Acad Dermatol. 2011;65:1-12. quiz 13-14
- [CrossRef] [PubMed] [Google Scholar]
- Calcinosis Cutis. July 17, 2021 In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2022.
- [Google Scholar]
- Idiopathic calcinosis cutis of the penis. J Clin Aesthet Dermatol. 2012;5:23-30.
- [PubMed] [PubMed Central] [Google Scholar]
- Andrews’ Diseases of the Skin: Clinical Dermatology (11 ed.). Philadelphia: Elsevier Saunders; 2011.
- Severe iatrogenic calcinosis cutis from extravasated calcium gluconate. Cureus. 2020;12:e9712.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dystrophic calcinosis cutis in subacute lupus. Dermatology. 1999;198:90-2.
- [CrossRef] [PubMed] [Google Scholar]
- Paraneoplastic syndromes: an approach to diagnosis and treatment. Mayo Clin Proc. 2011;85:838-54.
- [Google Scholar]
- New insight into calcinosis of juvenile dermatomyositis: a study of composition and treatment. J Pediatr. 2001;138:763-6.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of calcinosis cutis in systemic sclerosis and dermatomyositis: a review of the literature. J Am Acad Dermatol. 2020;82:317-25.
- [CrossRef] [PubMed] [Google Scholar]
- Calcinosis in rheumatic diseases. Semin Arthritis Rheum. 2005;34:805-12.
- [CrossRef] [PubMed] [Google Scholar]







