Translate this page into:
Pediatric Femoral Neck Fractures: Our Institutional Experience of 5 Years
*Corresponding author: Kafeel Khan, MBBS, MS, Post Graduate, Department of Orthopedics, SKIMS MCH Bemina, Srinagar, Jammu and Kashmir, India. kafeelk40@gmail.com
Abstract
Introduction
Pediatric femoral neck fractures remain an enigma for orthopaedics, especially with regard to the development of avascular necrosis (AVN). These rare fractures are fraught with complications including non-union, coxa vara, premature physeal closure, and AVN. Aggressive urgent management is required to limit the development of complications. We aim to share our institutional experience of 10 such cases, spanning over a period of 5 years by analyzing the radiological and clinical outcomes after anatomical reduction and internal fixation.
Materials and Methods
Ten children, aged < 16 years with fractured neck of the femur, treated in our hospital with a minimum follow-up of 1 year, were retrospectively reviewed and radiological and clinical outcomes following anatomical reduction and internal fixation were analyzed. Written informed consent was taken from the parents of the children included in the study.
Results
The mean age was 9.6 years. In total, 60% of the cases were boys and 50% cases were due to road traffic accidents (RTA). Furthermore, 50% cases were of Delbet type II pattern, 30% Delbet type III, and 20% Delbet type IV. All patients were treated with anatomical reduction and internal fixation. The final outcome was good in 80% of cases and fair in 20% of cases. We encountered only one case of AVN in our series.
Conclusion
Aggressive, urgent anatomical reduction and stable internal fixation is the modality of treatment. The outcome in patients is influenced by the development of complications including AVN, limb length discrepancy, and coxa vara, and every attempt should be made to prevent them.
Keywords
Avascular necrosis
Delbet classification
Pediatric femur neck fracture
Introduction
Pediatric femoral neck fractures constitute a rare entity accounting for less than 1% of the entire population of pediatric fractures.[1] Most of these fractures are a result of high-energy trauma.[2] Pediatric femoral neck fractures are fraught with complications including avascular necrosis (AVN) of the femoral head, non-union, delayed union, premature physeal closure, and coxa vara.[3] The most common and serious complication of these fractures is avascular necrosis (AVN) of the femoral head. As such, a thorough understanding of the fracture, including the anatomy is crucial for planning proper treatment. We share our institutional experience of the fracture by retrospectively reviewing and analyzing the clinical and radiological outcomes of 10 such cases, spanning over a period of 5 years. The mode of treatment in all cases was internal fixation (either open or closed).
Materials and Methods
We performed a retrospective observational study on all children ≤ 16 years of age with a femoral neck fracture, managed in the Department of Orthopaedics, SKIMS MCH, Bemina, Srinagar from May 2015 to May 2020. A total of 14 children ≤ 16 years were operated on in the hospital for fractured neck of the femur. All children with pathological fractures, associated neuromuscular disorders, open fractures, and those having a follow-up of < 1 year were excluded from the study. Out of the 14 patients, 2 had cerebral palsy, 1 had a pathological fracture secondary to a simple bone cyst, and 1 had a follow-up of < 1 year. These cases were accordingly excluded from the study, leaving a total of 10 hips of 10 patients (6 boys and 4 girls) who completed a minimum follow-up of 1 year for inclusion in the study. Written, informed consent for participation in the study was obtained from the parents of all patients included in the study.
The fractures were classified according to the Delbet classification[4] system as popularized by Colonna[4] and were subdivided into displaced and undisplaced [Figure 1]. All patients were operated on an urgent basis, within a period of 24 to 48 hours of the initial trauma. The treatment modality used was open reduction/closed reduction and internal fixation depending upon the patient profile and fracture pattern. At 1 year of follow-up, a final clinical and radiologic assessment was made using the Ratliff method[1] [Table 1]. A good outcome was rated as “satisfactory,” and fair and poor outcomes, or the presence of complications were rated “unsatisfactory.” The radiographs were assessed for joint congruity, arthritic changes, neck-shaft angle, and AVN. AVN, if present, was classified according to the Ratliff classification system for AVN [Table 2, Figure 2].[1] Limb length discrepancy was measured clinically. The collected data were analyzed using the IBM SPSS software version 28.0.1.1 for Windows. Continuous variables are expressed as mean ± standard deviation (SD) with its respective range. Nominal and ordinal variables are expressed as proportions. The Chi-square and Fisher’s exact tests were used for comparison of different groups and a p-value of < 0.05 was taken as statistically significant.

- Delbet classification of pediatric femoral neck fractures. I: Transphyseal; II: Transcervical; III: Cervico-trochanteric; IV: Intertrochanteric.

- Ratliff’s classification of AVN.
Good |
No or negligible pain, full or minimal restriction of hip movements, normal activity, or the avoidance of games. Normal or some deformity of the femoral neck in the radiograph |
Fair |
Occasional pain, less than 50% restriction of hip movement, normal activity, or avoidance of games. Severe deformity of the femoral neck, mild avascular necrosis in radiographs |
Poor |
Disabling pain, more than 50% restriction of hip movement, and restricted activity. Severe AVN, degenerative arthritis, arthrodesis in the radiograph |
Type 1 |
Diffused increased density of the proximal fragment, accompanied by the total collapse of the epiphysis |
Type 2 |
Segmental involvement of the femoral head, minimal collapse of the epiphysis |
Type 3 |
Metaphyseal AVN, changes confined to the femoral neck, excluding the epiphysis |
Results
The mean age of patients included in the study was 9.6 ± 4.12 years (range: 4–16 years). Our study included six boys (60%) and four girls (40%). The mechanism of injury varied, with road traffic accidents (RTA) accounting for the injuries in five patients (50%), falls from height (FFH) accounting for injuries in three cases (30%), and falls from a bicycle accounting for injuries in one case (10%). One case had a fall while playing at home [Table 3]. Associated skeletal injuries were present in four patients. These included head injury with transient loss of consciousness in two patients, a distal radial physeal injury in one patient, and a calcaneal fracture in one child [Table 4].
Etiology |
No. of patients |
|---|---|
Road traffic accidents (RTA) including motor vehicle accidents (MVA) and motorcycle accidents (MCA) |
5 |
Fall from height (FFH) |
3 |
Fall from bicycle |
1 |
Fall while playing |
1 |
Injury |
No. of cases |
|---|---|
Head injury including transient loss of consciousness |
2 |
Distal radial physeal injury |
1 |
Calcaneal fracture |
1 |
Five cases (50%) were classified as Delbet type II (transcervical), three (30%) as Delbet type III (cervico-trochanteric), and two cases (20%) as Delbet type IV (inter-trochanteric). We had no patient with Delbet type I fracture pattern (trans-physeal). The fractures were further classified as displaced (either minimal or complete displacement) or non-displaced. Six patients (60%) had displaced fractures, while four patients (40%) had non-displaced fractures.
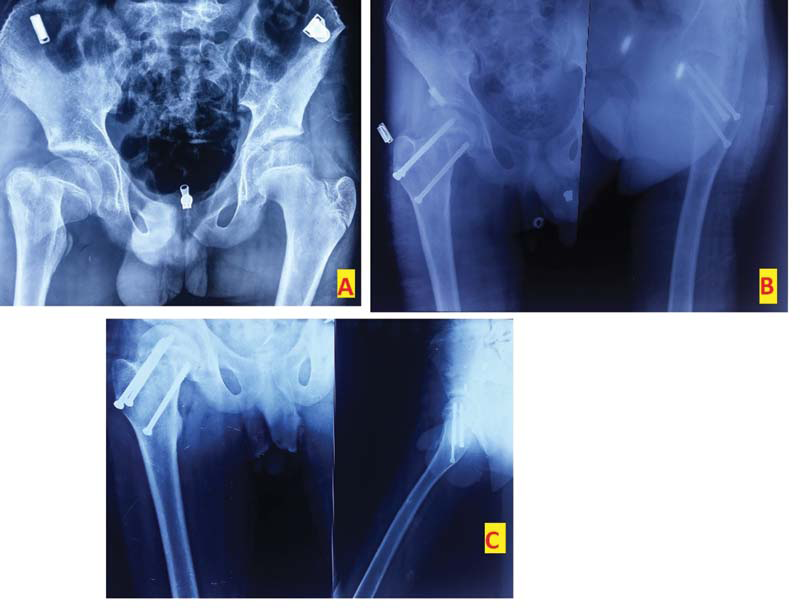
All patients were treated by internal fixation. Undisplaced fractures were treated by a percutaneous internal fixation on an orthopaedic table, under fluoroscopic guidance. Displaced fractures were treated either by CRIF under fluoroscopy [Figure 3] or by ORIF if closed reduction failed [Figure 4]. Of the six displaced cases operated, four had satisfactory anatomical reduction by closed methods. Two patients however needed ORIF. The choice of implants used for osteosynthesis depended on the surgeon’s preference and the age of the child. These included 6.5 mm partially threaded cannulated cancellous screws, 4.0 mm cannulated cancellous screws, pediatric dynamic hip screws, or pins [Table 5].
Case no. |
Age(y)/sex |
Mechanism of injury |
Delbet type |
Displacement |
Treatment |
Result |
|---|---|---|---|---|---|---|
1 |
04/M |
MVA |
II |
Undisplaced |
Percutaneous pinning |
Good |
2 |
10/M |
MVA |
III |
Undisplaced |
PCS |
Good |
3 |
11/M |
MVA |
IV |
Displaced |
CR+ pediatric DHS |
Good |
4 |
14/M |
MVA |
II |
Undisplaced |
PCS |
Good |
5 |
13/M |
FFH |
II |
Displaced |
CR + PCS and pinning |
Good |
6 |
16/M |
FFH |
IV |
Displaced |
OR+ Pediatric DHS |
Fair |
7 |
05/F |
Fall from bicycle |
III |
Displaced |
OR+ Screwing + one-leg spica |
Fair |
8 |
07/F |
FFH |
III |
Undisplaced |
PCS |
Good |
9 |
04/F |
MCA |
II |
Displaced |
CR+ screwing |
Good |
10 |
12/F |
Fall while playing |
II |
Displaced |
CR+ PCS |
Good |
Abbreviations: CR, closed reduction; DHS, dynamic hip screw; F, female; FFH, fall from height; M, male; MCA, motorcycle accident; MVA, motor vehicle accident; OR, open reduction; PCS, percutaneous screwing.

- Anteroposterior view of a 13-year-old boy with type II fracture (A). Postoperative radiograph showing fixation with a screw and two pins (B). Final radiograph at 1 year showing union (C).
- Anteroposterior radiograph of a 5-year-old boy showing a type III fracture (A). The boy needed OR and fixation with screws (B). Final radiograph at 1 year showing union (C).
Using the clinical and radiological assessment by the Ratliff system,[1] eight patients had a good clinical outcome (80%) [Figure 5]. Two patients had fair outcomes (20%). Of the two patients with unsatisfactory outcomes (fair outcomes), one had AVN and coxa vara [Figure 6], and one had a deep-seated infection of the hip leading to arthritic changes of the hip [Table 6]. We did not encounter any patient with a poor outcome in our series. In the study, one patient with a displaced, type III fracture had AVN and coxa vara. The patient had a type III Ratliff AVN with a neck-shaft angle of 120 degrees. A correlation analysis between different parameters and the outcome was made and the p-value was calculated for each parameter [Table 7]. We found no statistically significant association between the age of the patients, sex, fracture type and initial displacement, and outcomes in terms of the Ratliff system (p = 1.00, 1.00, 0.258, and 0.467, respectively). However, we found a statistically significant association between the type of reduction and the outcome (p = 0.022). With regard to the relation between AVN and outcomes, a satisfactory outcome was observed in eight of the nine patients without AVN (88.8%) and an unsatisfactory outcome was seen in one patient with AVN (100%). The only unsatisfactory outcome without AVN was seen in a 16-year-old male patient having a deep-seated infection of the hip, leading to arthritic changes in the hip.
Case No |
Age(y)/sex |
Delbet type |
Displacement |
AVN |
Coxa vara |
LLD (cm) |
Infection |
ROM limitation |
|---|---|---|---|---|---|---|---|---|
1 |
16/M |
IV |
Displaced |
– |
– |
– |
Osteitis |
– |
2 |
5/F |
III |
Displaced |
+ |
1200 |
3 |
– |
+ |
Abbreviations: AVN, avascular necrosis; F, female; LLD, limb length discrepancy; M, male; ROM, range of motion.
Parameter |
Satisfactory outcome (n) |
Unsatisfactory outcome (n) |
p-Value |
|
|---|---|---|---|---|
Age |
Age < 10 years |
4 |
1 |
1.00 |
Age > 10 years |
4 |
1 |
||
Sex |
Male |
5 |
1 |
1.00 |
Female |
3 |
1 |
||
Displacement |
Undisplaced |
4 |
0 |
0.467 |
Displaced |
4 |
2 |
||
Type of reduction |
Closed reduction |
8 |
0 |
0.022 |
Open reduction |
0 |
2 |
||
AVN |
AVN positive |
0 |
1 |
0.200 |
AVN negative |
8 |
1 |
||
Type of fracture |
I |
0 |
0 |
0.258 |
II |
5 |
0 |
||
III |
2 |
1 |
||
IV |
1 |
1 |
||

- Clinical image of the boy whose radiographs are shown in Figure 4 showing good outcomes; abduction (A), adduction (B), cross-legged sitting, (C) and squatting (D).
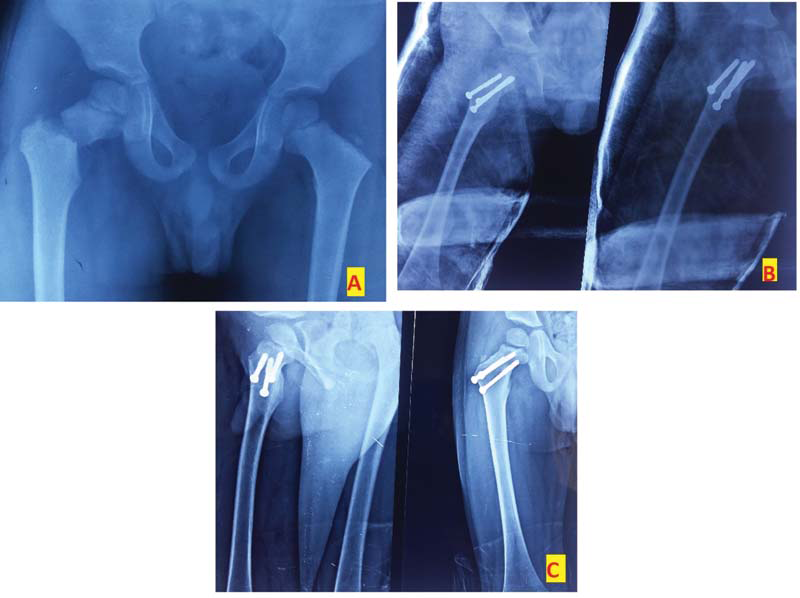
- Anteroposterior radiograph of a 5-year-old girl with type III fracture (A). The girl was managed by OR + screwing and a one-leg spica cast. (B). Although the child had type III AVN on final follow-up, the clinical result was considered fair (C).
Discussion
A high-energy force is required to fracture the femoral neck in children.[5] This is because the femoral neck is dense and hard in children compared with the adult counterpart.[6,7] The present study supported this knowledge, as 80% of the cases were a result of high-energy trauma (motor vehicle accident and fall from height). Concomitant injuries in children can frequently present with femur neck fractures. In our study, four patients had various associated injuries (40%). An orthopaedic surgeon should therefore do a meticulous examination of the patient so that these injuries are not missed.
In our study, we had five patients with a Delbet type II fracture (40%), three patients had a Delbet type III fracture pattern (30%), and two patients had a type IV fracture pattern (20%). We deduced that type II fracture patterns were the most common, followed by types III and IV. Type I fracture patterns are very rare. We did not encounter any patient with type I fracture pattern. As per the available literature, most of the large series on fracture neck of the femur in children reported similar findings.[8–12] We compared the fracture type with the final outcome and did not find any statistical significance (p = 0.258). Dai et al.[13] in their series on the analysis of risk factors for complications, did not see fracture displacement as an independent risk factor for developing AVN and poor outcomes. We support the same finding.
The blood supply of the femoral head differs in adults and children. The adult hip has intraosseous blood vessels that supply the femoral head. However, the blood vessels cannot cross the open physis, hence blood supply to the femoral head is critical in children and can be easily disrupted by a fracture.[14–17] Hence, AVN is the most common and damaging complication of pediatric femoral neck fractures.[18] The risk of AVN depends on several factors, including age, degree of initial displacement of the fracture, time to surgery, and the method of fixation.[19] The most important factor for the development of AVN is the severity of vascular compromise sustained at the time of trauma. The percentage of AVN reported in our series was 10%. The incidence of AVN ranges from 6 to 70% in the literature.[20–24] Most authors report a very high rate of AVN in type I fractures, ranging from 70 to 100%.[20,25–27] We did not encounter any type I fracture in our study. In a study published by Moon and Mehlman,[19] the rate of AVN in types II, III, and IV fractures were found to be 28, 18, and 5%, respectively. In our series, only one patient with a type III fracture pattern ultimately developed AVN and had an unsatisfactory outcome. However, her clinical outcome was considered fair with occasional pain and normal activities of daily living. The only patient without AVN having an unsatisfactory outcome was a 16-year-old male with post-infectious arthritis of the hip. Although a statistically insignificant p-value of 0.200 was obtained while comparing AVN and the outcome, the result was believed to be confounded by the unsatisfactory outcome due to post-infectious arthritis.
According to some authors, femoral head remodeling and blood supply restoration following femoral neck fractures are better achieved in children younger than 10 years.[8,27] However, most authors do not consider that young age prevents the development of AVN but reduces its extent and severity.[28,29] We encountered type III AVN in a child aged 5 years. With regard to the relation between the final outcome and the age of the patients, we found no statistical significance (p = 1.00). Similarly, we found no statistical significance between the gender of the patients and the final outcomes (p = 1.00).
Coxa vara is the second most common complication related to pediatric femoral neck fractures.[14] Coxa vara can occur after injury to the epiphyseal cartilage plate, cervico-cephalic necrosis, improper reduction/fixation, malunion, or a combination of these factors. This architectural problem of the proximal end of the femur may be associated with leg shortening.[3] In our series, we encountered one patient (10%) with coxa vara and limb shortening of 3 cm. Similar results were reported by Forlin et al.[29] and Togrul et al.[25]
The reported rate of infection in pediatric femoral neck fractures is 1%.[8,10,30] We encountered a single case of infection. The infection was resolved with intravenous antibiotics, sequential debridement, and saline lavages. The patient eventually developed an arthritic hip, which led to a poor outcome.
Anatomic reduction and adequate stabilization are essential to minimize the risk of complications.[14] Closed or open reduction followed by stable internal fixation is the current standard of care for all displaced fractures and is now increasingly being preferred for undisplaced fractures as well. In young children (<10 years), attempts should be made to spare the physis using screws short of it or using smooth Kirschner wires.[31] Transphyseal screw placement is preferable in children > 10 years of age, or whenever required for stable fracture fixation irrespective of the age. We found no statistical significance between the degree of initial displacement of the fracture and the outcome (p = 0.467). Similar results were drawn by a study conducted by Inan et al.[5] However, we found a statistically significant relationship between the type of reduction and the final outcomes (p = 0.022). We accordingly concluded that regardless of the age, sex, initial displacement, or fracture type, fractures that had an anatomical reduction on the operating table by closed methods had better outcomes than those requiring open reduction. However, certain authors suggest open reduction over closed means for displaced fractures, as it gives a complete anatomic reduction and may reduce the chances of complications.[32] This highlights the enigmatic nature of the fracture. In our study, we followed a middle path, where initially closed reduction was attempted, and open reduction was done only for children where closed reduction failed.
The evacuation of hematoma via a mini arthrotomy leads to a decrease in intracapsular pressure, which leads to a lower rate of AVN.[33] In contrast, several authors have reported no significant differences in the incidence of AVN with or without joint decompression.[18,34] Interpretation of the various reports is difficult as there are several confounding factors such as fracture type, displacement, and time to surgery. We did not perform joint decompression in any of our cases. Only one patient eventually had AVN.
One limitation of our study is the small sample size. However, considering the rarity of pediatric femoral neck fractures, we believe that anatomical reduction and stable internal fixation should be the modality of treatment. This fracture still remains an enigma, especially the development of AVN, and parents should be counseled about the possibility of the same.
Conclusion
Pediatric femoral neck fractures can be associated with devastating complications including AVN. A careful examination and urgent fixation of these fractures are required so that the complications are avoided. We believe that obtaining radiographically proven intraoperative anatomic reduction by closed methods and stable internal fixation should be the preferred modality of approach. However, one should not hesitate to perform an open reduction if closed methods failed. The presence of complications, including AVN, limb length discrepancy, joint incongruity, and infection leads to poor outcomes. Every attempt should be made to prevent these complications.
Funding
None.
Conflict of interest
None declared.
References
- Fractures of the neck of the femur in children. J Bone Joint Surg Br. 1962;44-B:528-42.
- [CrossRef] [PubMed] [Google Scholar]
- Fractures of the neck of the femur in children. JAMA. 1961;178:799-801.
- [CrossRef] [PubMed] [Google Scholar]
- Displaced femoral neck fractures in children: are complications predictable? Orthop Traumatol Surg Res. 2010;96:161-5.
- [CrossRef] [PubMed] [Google Scholar]
- Fracture of the neck of the femur in childhood: a report of six cases. Ann Surg. 1928;88:902-7.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric femur neck fractures: a retrospective analysis of 39 hips. J Child Orthop. 2009;3:259-64.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric femoral neck fractures: our 10 years of experience. Clin Orthop Surg. 2011;3:302-8.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvis and hip In: Rang M, Pring M, Wegner DR, eds. Rang’s children’s fractures, 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. p. :165-79.
- [Google Scholar]
- Fracture of the neck and intertrochanteric region of the femur in children. J Bone Joint Surg Am. 1977;59:431-43.
- [PubMed] [Google Scholar]
- Fractures of the hip in children: a review of forty cases. Clin Orthop Relat Res 1980:177-84.
- [CrossRef] [Google Scholar]
- Fractures of the neck of the femur in children. J Bone Joint Surg Am. 1971;53:1165-79.
- [PubMed] [Google Scholar]
- Controversies in the management of pediatric neck femur fractures- a systematic review. J Orthop. 2021;27:92-102.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Delayed treatment of femoral neck fractures in 58 children: open reduction internal fixation versus closed reduction internal fixation. J Pediatr Orthop B. 2016;25:459-65.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of risk factors for complications after femoral neck fracture in pediatric patients. J Orthop Surg Res. 2020;15:58.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Fractures of the proximal femur in childhood: a review. Indian J Orthop. 2020;55:23-34.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Hip fractures in children. J Am Acad Orthop Surg. 2009;17:162-73.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric proximal femur fractures. J Orthop. 2018;15:529-35.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Current controversies in management of fracture neck femur in children: A review. J Clin Orthop Trauma. 2020;11:S799-S806.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Factors affecting the outcome of fractures of the femoral neck in children and adolescents: a systematic review. Bone Joint J. 2013;95-B:135-42.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for avascular necrosis after femoral neck fractures in children: 25 Cincinnati cases and meta-analysis of 360 cases. J Orthop Trauma. 2006;20:323-29.
- [CrossRef] [PubMed] [Google Scholar]
- Fractures de hanche In: Clavert JM, Karger CL, Lascombes P, Ligier JN, eds. Fractures de l’enfant MOnographie du GEOP. montpellier: sauramps medical; 2002. p. :205-12.
- [Google Scholar]
- Dlouhodobé výsledky po zlomenine krcku stehenní kosti u detí. Acta Chir Orthop Traumatol Cech. 2005;72:98-104. [Long-term results following fracture of the femoral neck in children]
- [PubMed] [Google Scholar]
- Displaced fractures of the hip in children. Management by early operation and immobilisation in a hip spica cast. J Bone Joint Surg Br. 2002;84:108-12.
- [CrossRef] [PubMed] [Google Scholar]
- Les fractures du col du femur chez l’enfant In: Clavert JM, Metaizeau JP, eds. Les fractures des members chez l’enfant. Montpellier: Sauramps Medical; 1990. p. :295-313.
- [Google Scholar]
- Arthrotomy and open reduction of the displaced fracture of the femoral neck in children. J Pediatr Orthop B. 2001;10:205-10.
- [PubMed] [Google Scholar]
- Fractures of the femoral neck in children: long-term follow-up in 62 hip fractures. Injury. 2005;36:123-30.
- [CrossRef] [PubMed] [Google Scholar]
- Hip fractures in children. A long-term follow up of 17 cases. Orthopedics. 1989;12:361-7.
- [CrossRef] [PubMed] [Google Scholar]
- Transepiphyseal fractures of the neck of the femur in very young children. J Pediatr Orthop. 1992;12:164-8.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term follow-up of children with femoral neck fractures. J Bone Joint Surg Br. 1986;68:537-40.
- [CrossRef] [PubMed] [Google Scholar]
- Complications associated with fracture of the neck of the femur in children. J Pediatr Orthop. 1992;12:503-9.
- [CrossRef] [PubMed] [Google Scholar]
- Fractures of the hip in children; treatment and results. J Bone Joint Surg Am. 1953;35-A:867-87.
- [PubMed] [Google Scholar]
- Management of pediatric femoral neck fracture. J Am Acad Orthop Surg. 2018;26:411-9.
- [CrossRef] [PubMed] [Google Scholar]
- Open reduction of pediatric femoral neck fractures reduces osteonecrosis risk. Orthopedics. 2015;38:e983-e90.
- [CrossRef] [PubMed] [Google Scholar]
- Femoral neck fractures in children and the role of early hip decompression in final outcome. Injury. 2015;46:S44-S7.
- [CrossRef] [Google Scholar]
- Femoral neck fractures in pediatric patients: 30 years experience at a level 1 trauma center. Clin Orthop Relat Res. 2007;454:169-73.
- [CrossRef] [PubMed] [Google Scholar]








