Translate this page into:
Difficult Bronchoscopy and Foreign Body Removal: Our Experience
How to cite this article: Prabakaran S, Namasivaya NRB, Gowthame K, Karthika SR, Rajasekaran S. Difficult bronchoscopy and foreign body removal: Our experience. Int J Recent Sur Med Sci, doi: 10.1055/s-0043-1764365.
Abstract
Background
Foreign body in the airway is the most life-threatening situation. Most foreign bodies present as acute emergency and can be removed by endoscopy/bronchoscopy, while a few causes complication of a retained foreign body which requires emergency tracheostomy to secure airway followed by foreign body removal.
Case Presentation
We report our experience in the management of three children who required tracheostomy through which bronchoscope was introduced and foreign body removed. All patients with unrecognized retained foreign body presented with respiratory distress with desaturation. Imaging was suggestive of atelectasis. After foreign body removal patients recovered well and decannulated by day 5.
Subglottis is the narrowest part of pediatric airway. As these foreign bodies were vegetative they are hygroscopic in nature and hence would not be able to remove the foreign body by bronchoscopic guidance. Hence, tracheostomy was done to provide access followed by bronchoscopic removal.
Conclusion
Aspirated foreign body present challenges to the ear, nose, and throat surgeon. Newer techniques enable removal of foreign body easier. Tracheostomy combined with bronchoscopy can be a life-saving and easy to perform procedure which involves removal of foreign body at the same time.
Keywords
Flexible bronchoscopy
Laryngoscope
Respiratory distress
Tracheostomy
Introduction
Foreign body aspiration in children is an acute life-threatening emergency.[1] Children usually present with breathlessness, wheezing, cough, and stridor. FBs are divided into organic and inorganic. Foreign bodies in the tracheobronchial tree will cause more complications than other sites. Radiographs will only demonstrate radio-opaque foreign bodies and signs of aspiration. Rigid bronchoscopy will be useful in the identification and removal of foreign bodies in children. Tracheostomy is often required to secure the airway. Flexible bronchoscopy can be used for an initial assessment in case of a suspected foreign body aspiration.
This study aims to analyze our experience in the management of foreign body removal in three children who required emergency tracheostomy through which bronchoscope was introduced and foreign body was removed.
Case 1
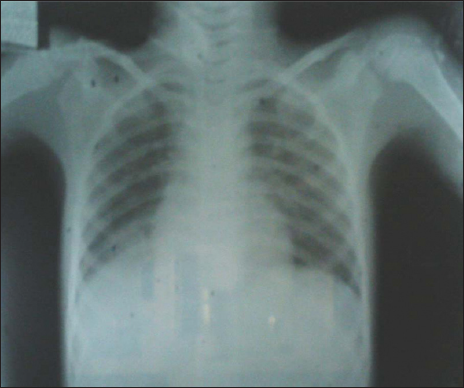
A 7-year-old male child was brought to the emergency unit with a history of foreign body aspiration (tamarind seed) 2 days back. The child had a history of breathlessness, drowsiness, refusal of feeds, vomiting, and intermittent fever. On examination, the child was in respiratory distress, trachea shifted to the right, decreased air entry on the right side, dull note on percussion, and vocal fremitus/vocal resonance decreased on the right side. Chest X-ray showed atelectasis changes of right lung [Figure 1].

- Chest X-ray showing atelectasis of right lung.
After all necessary investigations, the child was taken for surgery under general anesthesia, using a 4-mm rigid bronchoscope. Foreign body was visualized in the right main bronchus, but the foreign body could not be removed. A tracheostomy was done. Rigid bronchoscopy was introduced through the tracheostomy site and the foreign body was removed [Figure 2]. A 5 size Portex tracheostomy tube was inserted. Portex tube was changed into metal tube after 7 days. Spigotting was done after 3 days. Strapping was done after 2 days and the patient was discharged. Chest X-ray reverted back to normal after foreign body removal [Figure 3] and the child became stable.

- Removed foreign body—tamarind seed.
- Normal chest X-ray after foreign body removal.
Case 2
A 1.5-year-old female child was brought with complaints of foreign body ingestion (sapota seed) and history of difficulty in breathing. There was no history of vomiting or drowsiness. On examination, bilateral air entry and wheeze were present. There was a reduced air entry in the left infrascapular and infra-axillary area.
Under general anesthesia, a 3.5 size rigid bronchoscope was introduced and the foreign body was visualized in the trachea and the same was pushed to the right main bronchus. The foreign body could not be removed. The patient was intubated and shifted to the intensive care unit. Tracheostomy was done under general anesthesia and jet ventilation administered. Rigid bronchoscope (3.5 mm) was introduced through the tracheostomy site and the foreign body visualized in the right main bronchus and removed [Figure 4]. A 4-mm cuffed tracheostomy tube was introduced and secured [Figure 5]. The tube was changed into a metal tube after 7 days. Spigotting was done after 5 days. On the next day, decannulation was done.

- Removed foreign body—sapota seed.

- Child with tracheostomy tube.
Case 3
A 2 years and 10 months old female child was referred from a private hospital with the history of accidental foreign body aspiration (chicken bone) 4 days back. History of choking, noisy breathing, and change in voice was present. Previously, the child underwent a direct laryngoscope which showed glottic and subglottic edema and endotracheal intubation could not be done. On examination, the patient was in stridor and air entry decreased on both sides.
Under general anesthesia, tracheostomy was done through which a 4-mm bronchoscope was introduced and the foreign body was removed. Portex tracheostomy tube was inserted and secured [Figure 6]. Portex tube was changed into a metal tube after 3 days [Figure 7]. Direct laryngoscopy was done after 2 days, which showed normal glottis, subglottis, and supraglottis. Spigotting was done after 3 days. Strapping was done and the patient was discharged after 2 weeks.

- Procedure of tracheostomy.

- Child with metallic tracheostomy tube.
Discussion
Before the advent of bronchoscopy, foreign body aspiration resulted in mortality rates as high as 50%.[2] Gustav Killian was the first ear, nose, and throat (ENT) surgeon to remove an airway foreign body (pig bone) using a rigid esophagoscope which was later developed and modified by Chevalier Jackson who used rigid bronchoscope to remove airway foreign body.[3]
The aspiration of foreign body occurs more commonly in children aged less than 3 years. The most commonly aspirated items are food and coin especially during crying, laughing, and oral phase.[4] The clinical features will depend upon the site, size, and nature of the foreign body. Most commonly aspirated foreign body is peanut followed by pumpkin seeds and pen caps and common sites of foreign body enlodgement are right main bronchus, larynx, and trachea.[5]
Children usually present with difficulty in breathing, refusal of feeds, stridor, choking, and change in voice. Flexible bronchoscopy had high success rates of approximately 91.3% in removing airway foreign body though it failed in two patients who had a peanut lodged in the right bronchus and it was difficult to remove the foreign body as one piece meal.[5] Experiments in rabbits has shown acute inflammatory response after 3 days of retained foreign body.[6]
The initial investigation of choice for an aspirated foreign body is plain chest radiography which demonstrates the radio-opaque foreign body.[7] Other features suspecting presence of radiolucent foreign bodies include atelectasis, hyperinflation, pneumothorax, and pneumonia. Computed tomography can be useful in case of suspected foreign body and the late signs of aspiration like pneumonia, bronchiectasis, and bronchial stenosis. Up to 39% of foreign body aspiration will go unnoticed.[8]
Flexible bronchoscopy under general anesthesia is the gold standard method for diagnosis and removal of aspirated foreign bodies as single-stage procedure.[9] Subglottis is the narrowest part of pediatric larynx. Vegetative foreign bodies are hygroscopic in nature and hence could not be removed under bronchoscopic guidance alone. Tracheostomy is required to secure the airway and acts as a conduit for foreign body removal. Grasping forceps are used for the removal of inorganic foreign bodies where a firm grasp is required to prevent slipping.[10] Organic objects should not be removed with grasping forceps which may cause dispersion into distal airways. Flexible bronchoscopy is preferred in older children and adults. It is helpful in the identification of a foreign body when it is covered with blood or granulation tissue. Complications of bronchoscopy include acute bronchitis, postoperative pneumonia, and bleeding requiring reintubation.[11]
Newer diagnostic techniques like inflatable balloon catheters and cryoprobe can be used to remove a distal hygroscopic foreign body and have become an emerging trend, although it requires great expertise and adequate instrumentations.[4]
Complications of foreign body aspiration are divided into acute and chronic. Acute complications are asphyxia and respiratory distress whereas chronic complications are pneumonia, atelectasis, and empyema. Parents should be educated regarding lifestyle and cultural habits to prevent foreign body aspiration.
Conclusion
Aspirated foreign body presents challenges to the ENT surgeon. Newer techniques enable the removal of the foreign body easier. Tracheostomy combined with bronchoscopy can be a life-saving and easy to perform procedure which involves removal of a foreign body at the same time.
Conflict of interest
None declared.
Reference
- Management of foreign body removal in children by flexible bronchoscopy. J Bronchology Interv Pulmonol. 2017;24:21-8.
- [CrossRef] [PubMed] [Google Scholar]
- Rigid bronchoscopy for foreign body removal: an overview. Intl J Otorhinolaryngol Head Neck Surg. 2017;3:936-8.
- [Google Scholar]
- Foreign body removal in children and adults: review of available techniques and emerging technologies. AME Med J. 2018;3:75.
- [Google Scholar]
- Foreign body removal by flexible fiberoptic bronchoscopy in infants and children. Pediatr Pulmonol. 2005;40:392-7.
- [CrossRef] [PubMed] [Google Scholar]
- Morbidity and mortality in children undergoing bronchoscopy for foreign body removal. Laryngoscope. 2018;128:1226-9.
- [CrossRef] [PubMed] [Google Scholar]
- Foreign body inhalation in the adult population: experience of 25,998 bronchoscopies and systematic review of the literature. Respir Care. 2015;60:1438-48.
- [CrossRef] [PubMed] [Google Scholar]
- Tracheal foreign body removal using flexible bronchoscope in a pediatric patient. A novel approach. Am J Respir Crit Care Med. 2017;196:1071-2.
- [CrossRef] [PubMed] [Google Scholar]
- Foreign body ingestion in children. Clin Endosc. 2018;51:129-36.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Foreign body ingestion in children. Turk Pediatri Ars. 2015;50:234-40.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Flexible bronchoscopy with multiple modalities for foreign body removal in adults. PLoS One. 2015;10:e0118993.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Questioning the legitimacy of rigid bronchoscopy as a tool for establishing the diagnosis of a bronchial foreign body. Int J Pediatr Otorhinolaryngol. 2012;76:194-201.
- [CrossRef] [PubMed] [Google Scholar]







