Translate this page into:
Splenic Rupture During Pregnancy: A Misdiagnosed, Rare Obstetrical Emergency

*Corresponding author: Dr Tanu Sharma, Department of Obstetrics and Gynaecology, Rajendra Institute of Medical Sciences, Bariatu, Ranchi, India. tanisha.anu@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma T, Kumari A, Srivastava K. Splenic Rupture During. Pregnancy: A Misdiagnosed, Rare Obstetrical Emergency. Int J Recent Surg Med Sci. 2024;10:121-4. doi: 10.25259/IJRSMS_57_2023.
Abstract
Splenic rupture in pregnancy is a rare entity, and the exact ethology is not very clear. Splenic rupture during pregnancy can be due to trauma or spontaneous due to other non-traumatic causes like hemophilias, leukaemia, kalazaar, splenic artery aneurysm, etc. Patients usually present in 3rd trimester and are frequently misdiagnosed as a case of placental abruption or uterine rupture. It leads to hypovolumic shock and increases maternal and fetal morbidity and mortality. Here, we have presented 3 cases of spontaneous splenic rupture and injury without any antecedent history in the first case, after a fall in 2nd case, and associated with kalazaar in 3rd case. Two patients were managed conservatively and had uneventful postoperative period, while splenectomy was done in one case, and feto-maternal mortality was seen in the same. The first two cases were preoperatively misdiagnosed as uterine rupture, and 3rd case was postoperatively diagnosed as Kalazaar. There is a need to enhance the knowledge of this rare condition in pregnancy as it is usually misdiagnosed and lethal for both mother and foetus.
Keywords
Obstetrical emergency
Splenic hematoma
Splenic rupture
INTRODUCTION
A spontaneous rupture of the spleen is a rare, life-threatening condition that is usually misdiagnosed. It is often observed after trauma and in pre-existing pathology of the spleen, like splenic artery aneurysm or thalassemia, or infections such as malaria, typhoid, or infectious mononucleosis.[1-3] Spleen is a vascular organ, and if it is diseased or enlarged, minor trauma may result in significant bleeding. Splenic rupture in pregnancy is attributed to physiological factors like hypervolemic state and splenic enlargement and mechanical factors like decreased peritoneal cavity volume due to an enlarged uterus and muscular contractions during pregnancy. The risk of splenic rupture is further increased because of compression by abdominal musculature when there is an increase in intra-abdominal pressure following minimal strain like coughing or sneezing and observed mostly in the third trimester or puerperium.[4-6] Spontaneous (atraumatic) rupture of the spleen is an uncommon but catastrophic clinical entity. The clinical feature may mimic a uterine rupture or placental abruption and is often observed intraoperatively.[1] The delay in recognition can be fatal to both the mother and the fetus. The incidence of spontaneous splenic rupture during pregnancy is around 0.1–0.5%. The reported maternal mortality ranges between 0% and 45%, and fetal distress followed by death in 47%–82%.[4] The cause of maternal death is hypovolemic shock. Some cases need splenectomy, while few cases get managed conservatively. The purpose of this case series, comprising three cases, is to identify and enhance awareness of this unusual condition.
CASE SERIES
Case 1
A 25-year-old primigravida at 39 weeks of gestation was referred from a peripheral hospital with the diagnosis of fetal distress. She gave a history of acute pain in the epigastric region and less fetal movement since 3–4 hrs. There was no history of trauma, vomiting, leaking, or bleeding p/v. No history of hypertension as per her antenatal history or fever, rash, or pruritus. No significant past medical, surgical, or family history. On general examination she was perspiring, severely pale, PR = 142/min, BP = 100/66 mmHg, respiratory rate = 28/min, SpO2 = 98% on room air. On abdominal examination, there was distension, uterine contour indistinguishable, generalized tenderness, FHR = not audible by stethoscope or doppler. P/V = cx short, soft, central, os closed. Paracentesis shows blood tap. Her Hb was 5 g%, TLC = 21000/cumm, and Platelet count = 1,26000/cumm.
The patient was taken for emergency laparotomy in view of the ruptured uterus, along with resuscitation for hypovolemic shock. On laparotomy, approximately 1 L of hemoperitoneum was suctioned out. The uterus was found to be intact. Lower segment Cesarean section was done with the delivery of a alive, term, and asphyxiated male baby who was handed over to a pediatrician. The uterus was closed in double layers. Ovaries and tubes were normal. Upper abdominal exploration was done with the help of a surgeon to find the cause of hemoperitoneum. A large clot of approximately half a kidney tray was removed from the perisplenic region. There was subcapsular splenic hematoma grade 2 with a small laceration, which was confined, and no active bleeding was found, as shown in Figure 1. The intraperitoneal drain was applied, and the abdomen closed in layers 2 units of PRBC, 2FFP, and 2Platelet concentrate were transfused. Postoperatively, the patient was put in HDU. Vitals improved dramatically. 300cc collected blood was drained in the intraperitoneal drain in 24 hours, 100cc more blood was drained in the next 24 hours than minimal. Drain removed on post-op day 5. The postoperative period was uneventful, and she was discharged on post-op day 12.
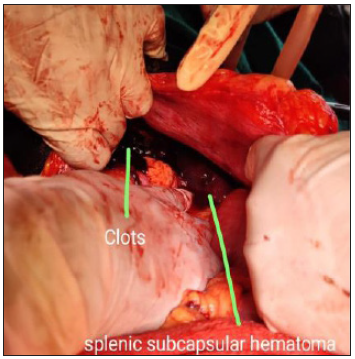
- Splenic subcapsular hematoma.
Case 2
A 32-year-old, G3P2L2, previous vaginal delivery, 37 weeks pregnancy, was referred from the district hospital in hypovolemic shock on inotropic agent. Attendants gave the history of a fall in the bathroom followed by severe pain abdomen, which was radiating to the shoulder and back (as per the patient). Her general condition was poor, conscious, perspiring, severe pallor, PR = 152/min, BP = 80/50 mmHg, RR = 32/min, SpO2 = 95% on room air. On abdominal examination, there was gross distension, uterine contour could not be delineated, guarding, and generalized tenderness all over the abdomen. FHR could not be audible with a stethoscope or Doppler. Per vaginally- the cervix was long, soft, central, internal, os admitting one finger. Paracentesis showed a blood tap.
With resuscitation, the patient was taken for emergency laparotomy in view of a ruptured uterus. On opening the abdomen, approximately 1.5 L of hemoperitoneum was suctioned out, and the uterus was found to be intact. A lower segment Cesarean section was done, delivering a fresh dead male baby. The uterus was closed. Bilateral adnexa and POD were found to be normal. The surgeon was called, and the upper abdomen was explored after extending the incision upwards. Two fists of clots were removed from the left paracolic gutter and perisplenic region. There was profuse bleeding seen from the hilum of the spleen, which was tried to secure by hemostatic sutures but could not be secured. Thus, the decision of splenectomy was taken and done, as shown in Figures 2a and 2b. Three units of PRBC, FFP, and platelet concentrate were transfused. However, the patient’s condition deteriorated and could not be extubated after surgery. She developed asystole thrice intraoperatively and unfortunately died within an hour of surgery.
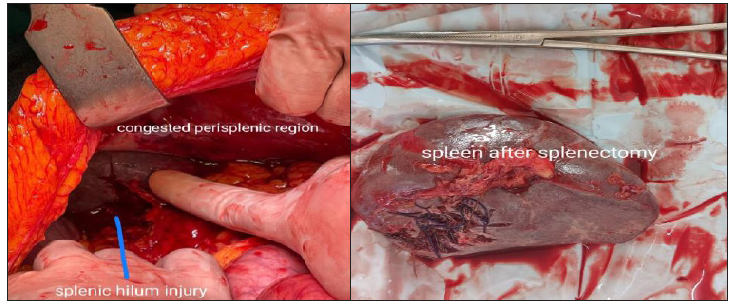
- (a) Splenic rupture at hilum. (b) Spleen after splenectomy.
Case 3
G2P1L1, 38 weeks 6 days pregnancy, previous 1 Cesarean section, came with the complaint of pain in the abdomen intermittently for 12 hours. She had a history of fever and abdominal fullness before this conception, for which she took some ayurvedic medication. Antenatal investigations showed Hb = 7.2g%, ABORh = B+, and serology = NR. She was lean, thin, built with moderate pallor, and normotensive. Abdominal examination showed massive splenomegaly, palpable up to the left lumbar region, symphysis-fundal height corresponding to 32 weeks size, severe IUGR, moderate contraction, cephalic presentation, head 5/5 palpable, scar tenderness present, FHR = 124 bpm. There were no features of bleeding tendencies. Per vaginal examination = cervix 2 cm dilated, 50% effaced, fore bag of membrane forming, vertex high up, bilateral sidewalls convergent.
Emergency LSCS was done after an urgent platelet count report (72000/cumm) and sickling test were found to be negative. On opening the abdomen, there were moderate ascites, the previous uterine scar was thinned out, and the uterus was stained with fresh blood. Lower segment Cesarean section was done with the delivery of an alive term, IUGR male baby of 2 kg and bilateral tubal ligation. The uterus was closed in double layers. A massively enlarged spleen was visible on the left side of the uterus, and blood was oozing from the undersurface of the spleen near the uterus. It can be due to injury from the contraction of the uterus. As there was no active bleeding, therefore abdomen closed in layers after applying an intraperitoneal drain on the right side of the abdomen. The drain was removed within 48 hours, as there was only a minimal serous collection noted. Meanwhile, the patient was investigated and found to be a case of Kalazaar, which is prevalent in some regions of Jharkhand. So, the patient was treated for the same, and the rest postoperative period was uneventful.
DISCUSSION
Rupture of the spleen in pregnancy is a rare clinical event. A spontaneous rupture of a normal spleen is observed in the absence of antecedent trauma. The etiology of spontaneous rupture of a normal spleen in pregnancy is not completely understood. It has been suggested that splenic enlargement, increased blood volume, and diminished peritoneum cavity volume due to an enlarged pregnant uterus could be implicated in the pathogenesis of splenic rupture.[1,3] Estrogen and progesterone cause structural changes to the spleen that may increase the risk of splenic rupture during pregnancy, even after minor trauma or without any underlying cause.[1] It is more commonly seen in 3rd trimester, and the basic problem is its delayed recognition as it mimics clinical features of a ruptured uterus and placental abruption.[2,5] A review of the literature shows splenectomy as the standard approach, while few case reports show conservative management depending on the patient’s hemodynamic condition and grade of splenic injury, as we have managed in the cases mentioned above. Maternal hemodynamic decompensation due to massive hemorrhage leads to maternal death and decreased uteroplacental flow, resulting in fetal demise. Etiological factors are traumatic (most common) and atraumatic risk factors like pregnancy-induced hypertension, infectious like malaria, infectious mononucleosis, kalazar, typhoid, hemolytic anemia, hemophilia, lymphoma, leukemia, metastatic cancer, hemangioma, aneurysm, iatrogenic due to drugs like heparin, warfarin, streptokinase, idiopathic and maybe even found in a normal spleen.[4] The most common symptom of atraumatic splenic rupture is left upper quadrant abdominal pain, which is sharp. Patients develop anemia with shoulder pain on the left side (Kehr’s sign), guarding and rebound tenderness, hypotension, and tachycardia. The spleen may be enlarged in size. The patient may develop periumbilical ecchymosis, known as the Cullen sign. The symptoms of splenic artery rupture or splenic capsular rupture are violent spontaneous pain in the left hypochondrium or epigastrium. It is usually misdiagnosed as abruptio placentae or uterine rupture. Diagnostic procedures like ultrasonography may detect free intraperitoneal fluid, and peritoneal lavage may reveal hemoperitoneum, but the final diagnosis is made on laparotomy. Treatment of splenic rupture involves primary surgical treatment like total splenectomy, non-surgical treatment like splenic arterial embolization, or conservative management. However, spontaneous splenic hematoma without any underlying cause is rarely reported during pregnancy, but we have observed this in our case 1 mentioned, leading to the wrong diagnosis of abruptio placentae and uterine rupture. Along with resuscitation of the patient, bedside ultrasonography can help in defining uterine contour and intra-abdominal collection. However, the use of ultrasound or other imaging modalities should not delay the definitive management as it will lead to more complications like hemorrhagic shock, fetal demise, and disseminated intravascular coagulation (DIC). Conservative management should be followed by intensive monitoring with the facility of round-the-clock availability of intervention radiologists, surgeons, and blood products. Otherwise, urgent exploratory laparotomy should be aimed to conserve the spleen by repair of the capsule, splenorrhaphy, and partial splenectomy. Ligation of splenic vessels should be tried before splenectomy according to the patient’s response on resuscitation, as splenectomy may increase the risk of frequent infections and overall morbidity and mortality. The cases of splenic hematoma in the third trimester of pregnancy are reported in the literature, where patients presented with hemoperitoneum. On laparotomy, a large splenic hematoma with splenic laceration was found, and the patient was managed conservatively with good maternal outcome [4,5] as in case 1. We have also done emergency laparotomy in view of uterine rupture in the first two cases and could save one patient conservatively while losing the second one even after splenectomy. Hamsho and Mouchanta reported a case of splenic rupture following the history of fall in the third trimester of pregnancy,[7] similar to case 2 was presented after the fall, and a splenectomy was performed for the same. Some studies have reported splenic injury even following trivial abdominal straining where the diagnosis was made during laparotomy only.[4] Splenectomy had to be done in our second-mentioned case as there was active bleeding, but whenever possible, conservative surgery should be preferred. Pregnancy with massive splenomegaly can also lead to lacerations over the spleen during labor, as uterine contraction can cause minor injury to the spleen, as in our case 3. Thus, surgeons should be vigilant and should keep in mind a differential diagnosis of uterine rupture or abruptio placentae.
CONCLUSION
Splenic rupture in pregnancy is a life-threatening situation. It should be considered as a diagnosis of hemoperitoneum without a uterine explication. Emergent laparotomy and splenectomy before the setting of collapse is the essential key to reducing maternal morbidity and mortality and increasing the chances of fetal survival. During the examination of pregnant women, we must also keep in mind the possibility of splenic rupture, especially if present in hypovolemia with abdominal pain in the epigastrium or left hypochondrium, with no antecedent history of trauma. Though this is a rare occurrence, failure to recognize it is common and can be fatal for both mother and child.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient consent is not required as the patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
REFERENCES
- Spontaneous Splenic Rupture in Pregnancy. Pan Afr Med J. 2015;21:312.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Splenic Rupture in Pregnancy-Traumatic or Spontaneous Event. Em J Obstet Gynecol Reprod Biol. 2004;115:113-4.
- [Google Scholar]
- Spontaneous Rupture of the Spleen during Pregnancy. J Obstet Gynaecol India. 2012;62:692-3.
- [CrossRef] [PubMed] [Google Scholar]
- Conservatively Managed Spontaneous Splenic Rupture in Pregnancy with Severe Preeclampsia: An Interesting Case Report. Int J Reprod Contracept Obstet Gynecol. 2023;12:2284-6.
- [Google Scholar]
- Rupture of the Spleen during Pregnancy with Intrauterine Fetal Death Mimicking Rupture Uterus: A case Report. Telangana Journal of IMA. 2022;2:48-52.
- [Google Scholar]







