Translate this page into:
Is Percutaneous Screw Fixation with 6.5 mm Cannulated Cancellous Screws a Viable Option in Pelvic Ring Fractures?
*Corresponding author: Yash Gulati, MBBS, Department of Orthopaedics, Netaji Subhash Chandra Bose Medical College and Hospital, Dhanvantari Nagar, Jabalpur, Madhya Pradesh, India. yash_gulati4790@yahoo.co.in
Abstract
Background
Historically, internal fixation in pelvic ring fractures has been proven to be better in outcome than both external fixation and conservative management. In an attempt to overcome the morbidity of extensile surgical approaches, percutaneous fixation of the pelvis has been receiving increasing attention. The aim of the study was to assess the functional outcome in patients with pelvic ring fractures treated with percutaneous screw fixation.
Methods
The study included 12 patients of pelvic ring fracture admitted at NSCB medical college, Jabalpur (Madhya Pradesh) from December 2019 to October 2021, all treated percutaneously with cannulated cancellous screw fixation. Four patients had Tiles type C1 injury, 4 patients with type C2, 2 with type B1 and 2 with type A2 injury. Functional assessment was done using the Majeed Scoring system at preoperative, at 3 weeks, 6 weeks, and 3 months postoperatively.
Results
Functional outcome score at 3-month follow-up was poor in 8% patients, fair in 8% patients, good in 33.3% patients, and excellent in 50% patients. Pain was the most frequent complaint on follow-up.
Conclusion
Fixation of acute pelvic ring injuries with 6.5 mm cc screws using percutaneous technique offers favorable functional outcome and can be performed in hemodynamically unstable patients.
Keywords
Fracture
MIS
Pelvis
Percutaneous
Ring
Screw
Introduction
Pelvic ring injuries cover a broad spectrum, ranging from simple minimally displaced fractures of the sacrum or pubis that can be treated conservatively to high-energy disruptions of the bony or ligamentous ring representing life-threatening injuries requiring intervention. Over the years, several methods of external and internal fixation have been devised.
Several studies have found that internal fixation is much better than both external fixation and conservative treatment in managing unstable pelvic ring disruptions.[1,2]
In an attempt to overcome the morbidity of extensile surgical approaches, percutaneous fixation of the pelvis described by Letournal[3] by open method and later by Routt et al.[4] by strictly percutaneous method has been receiving increasing attention.
This study highlights the use of 6.5 mm partially threaded cannulated cancellous screws for fracture fixation instead of conventionally used 7.3/7.5 mm screws (which may not be available at some centers), and functional outcome of operated patients.
Materials and Methods
This prospective interventional study included 12 patients with pelvic ring disruption admitted to the Department of Orthopedics, Netaji Subhash Chandra Bose Medical College and Hospital, Jabalpur, Madhya Pradesh from December 2019 and October 2021 as they presented to us in casualty/OPD department, with approval from the Institute’s Ethics Committee.
Inclusion Criteria:
Acute pelvic ring injury: stable as well as unstable
Fractures where closed reduction was possible by closed/transcutaneous method
Fracture duration less than 14 days after hemodynamic stability
Exclusion Criteria:
Pathological fractures such as those associated with primary, malignant or benign tumors, bony metastasis, and metabolic disorders
Patients with mental disorders
Patients walking with assistive devices before trauma
Pre-existing conditions affecting the pelvis (previous surgery, deformities)
Pregnancy
The patient was thoroughly examined upon presentation for osseous and extraosseous injuries. Anteroposterior, inlet, outlet and Judet oblique views were taken after admission. CT scan of the pelvis with 3D reconstruction was done to rule out occult fractures and better plan surgery.
All patients were classified using the Tiles Classification[5] into types A, B and C. Treatment was planned based on Tiles type–fractures (including open book and unstable injuries) fulfilling above criteria were included in the study.
Tiles classification of pelvic ring injuries:
Type A: stable (posterior arch intact)
-
-
A1: avulsion injury
-
-
A2: iliac-wing or anterior-arch fracture due to a direct blow
-
-
A3: transverse sacrococcygeal fracture
Type B: partially stable (incomplete disruption of posterior arch)
-
-
B1: open-book injury (external rotation)
-
-
B2: lateral-compression injury (internal rotation)
B2–1: ipsilateral anterior and posterior injuries
B2–2: contralateral (bucket-handle) injuries
-
-
B3: bilateral
Type C: unstable (complete disruption of posterior arch)
-
-
C1: unilateral
C1–1: iliac fracture
C1–2: sacroiliac fracture-dislocation
C1–3: sacral fracture
-
-
C2: bilateral, with one side type B, one side type C
-
-
C3: bilateral type C
Preoperatively, patients received an enema to clear the bowel and provide clear intraoperative fluoroscopic views. Intraoperatively C arm was used in different orientations to view the screw trajectories in pelvis.
Fracture was first reduced by manual compression or using reduction clamps percutaneously, as and when required.
As and when required, fixation of posterior pelvic ring was supplemented by the fixation of anterior pelvis using external fixator/symphyseal plating.
Implants
All cases were treated with partially threaded 6.5 mm cannulated cancellous screws of varying sizes (75–110 mm) for fixation of posterior pelvic ring, and 4 mm screws for acetabular fractures.
Posterior Fixation: Iliosacral screws were used to fix SI joint disruption/sacral fractures [Figure 1]. Anterior Fixation: Open anterior fixation by symphyseal plating was done in one patient [Figure 2], external fixation was done in one patient to supplement percutaneous fixation with screws for posterior ring disruption. Anterior acetabular column was fixed using a screw in one patient [Figure 3].
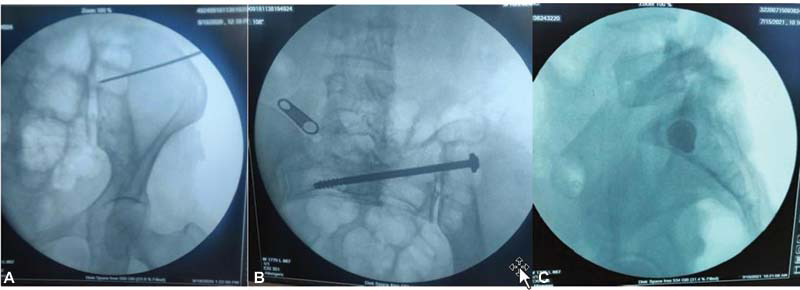
- Percutaneous cc screw insertion for SI joint disruption. (A) Passage of guide wire, along which drill bit is passed, (B) final position of screw, (C) screw position on lateral projection.

- (A) Preoperative X-rays, (B, C) postoperative X-rays. (D) At 6 weeks of follow-up: patient able to sit up without discomfort functional Majeed score of 33, (E, F) At 6 months of follow-up: patient able to walk freely without pain, returned to his previous occupation as a farmer with functional Majeed score of 98.

- Percutaneous cc screw insertion for fixation of anterior acetabular column fracture. (A) Insertion of guide wire and drill bit, (B) insertion of cc screw, (C) final position of screw on postoperative X-ray.
Quadrilateral plate was fixed with a “magic screw” in one patient.
Patients were discharged from ward on the third postoperative day and followed up at 3 weeks, 6 weeks, and 3 months radiologically with X-rays (AP, inlet, outlet, and Judet oblique views) and functionally by Majeed score, and visual analog scale.
Functional Majeed Score: Majeed[6] evolved a numerical grading system for functional outcome assessment of pelvic fractures based on a 5-year prospective study on 60 patients with pelvic fractures.[4] These included:
-
-
Pain (30 points)
-
-
Work (20 points)
-
-
Sitting (10 points)
-
-
Sexual intercourse (4 points)
-
-
Standing (36 points)
Each of these clinical parameters was scored, the total being a maximum of 100 points for patients who were working before the injury and 80 points for those who were not.
The results were graded as excellent good, fair, or poor as listed in [Table 1].
Working before injury |
Not working before injury |
Grade |
|---|---|---|
>85 |
>70 |
Excellent |
70–84 |
55–69 |
Good |
55–69 |
45–54 |
Fair |
<55 |
<44 |
Poor |
Visual analog scale (VAS) was used as a simple yet effective tool to gauge the amount of pain patient experiences. This is especially useful with less-educated patients.
Patients were also assessed for their ability to sit, squat, and cross leg comfortably on final follow-up, as these positions form an important part in doing activities of daily living in the Indian scenario.
Results
In this study, six male and six female patients were operated with most patients in the fourth and fifth decades of life (75%), among which, two patients had Tiles type A2 fracture, two had type B1, four with type C1, and four with type C2 fracture.
Road traffic accident was the most frequent cause of trauma (67%), followed by fall from height (25%).
Sacroiliac disruption was fixed in eight patients, sacral fractures in two using 6.5 mm iliosacral screws. Acetabular fracture was fixed in one patient. Quadrilateral plate of innominate bone was fixed in one patient with 4 mm cc screw.
Iliosacral screw misplacement and infection occurred in one patient and had to be removed. Among the 12 patients, 8 were working before trauma. Their average Majeed score on 3-month follow-up was 75.75. Six of these patients were able to return to their place of work, and one of them had a change of occupation.
Four non-working patients had an average Majeed score 68.5 after 3 months of follow-up.
Majeed score at 3 month follow-up showed poor outcome in one patient (8%), fair outcome in one patients (8%), good outcome in four patients (33.3%), and excellent outcome in six patients (50%) [Table 2].
Functional outcome |
Number of patients |
Percentage |
|---|---|---|
Excellent |
6 |
50.0 |
Fair |
1 |
8.3 |
Good |
4 |
33.3 |
Poor |
1 |
8.3 |
Total |
12 |
100.0 |
The average Majeed score at preoperative period, 3 week, 6 week, and 3 month postoperative follow-up showed a significant improvement in the functional outcome (p < 0.01). Eight out of the operated patients were able to sit, squat, and cross leg comfortably at 3 months of follow-up.
The Majeed score increased from the mean preoperative value of 12.83 ± 7.19 to 29.5 ± 7.17 at 3 weeks follow-up (p < 0.01) to 48 ± 14.35 at 6 weeks follow-up (p < 0.01) and to 73.25 ± 11.58 at 3 months follow-up (p < 0.01), all of which are statistically significant [Tables 3 and 4].
Minimum |
Maximum |
Mean |
Std. deviation |
|
|---|---|---|---|---|
Preoperative score |
4 |
24 |
12.83 |
7.19 |
3 weeks follow-up |
16 |
40 |
29.50 |
7.17 |
6 weeks follow-up |
24 |
68 |
48.00 |
14.35 |
3 months follow-up |
52 |
90 |
73.25 |
11.58 |
Pairs |
t-value |
Significance (2-tailed) |
|---|---|---|
Preoperative vs 3 weeks follow-up |
–10.935 |
<0.001 |
Preoperative vs 6 weeks follow-up |
–15.210 |
<0.001 |
Preoperative vs 3 months follow-up |
–20.641 |
<0.001 |
VAS score decreased from the mean preoperative value of 9.16 ± 0.93 to 6.25 ± 0.93 at 3 weeks follow-up (p < 0.01) to 6.25 ± 1.91 at 6 weeks follow-up (p < 0.01) and to 4.08 ± 1.8 at 3 months follow-up (p < 0.01), all of which were statistically significant [Tables 5 and 6].
Minimum |
Maximum |
Mean |
Std. deviation |
|
|---|---|---|---|---|
Preoperative Score |
8 |
10 |
9.16 |
0.93 |
3 weeks follow-up |
3 |
8 |
6.25 |
1.91 |
6 weeks follow-up |
1 |
7 |
4.08 |
1.83 |
3 months follow-up |
0 |
5 |
2.00 |
1.80 |
Pairs |
t-value |
Significance (2-tailed) |
|---|---|---|
Preoperative vs. 3 weeks follow-up |
2.0835 |
<0.001 |
Preoperative vs. 6 weeks follow-up |
4.1271 |
<0.001 |
Preoperative vs. 3 months follow-up |
6.1590 |
<0.001 |
Complications: Out of operated patients, one patient had surgical site infection, which subsequently was treated by removal of implanted screws.
There was persistent lower back pain in five (41.5%) patients at final follow-up. Iliosacral screw was removed in one patient for persistent lower back pain 6 months after surgery [Figure 4].

- (A) Preoperative 3D reconstruction of the pelvis, (B–D) postoperative X-rays, (E, F) At 5-month follow-up: patient able to walk with limp, Majeed score of 72.
There was no incidence of any neurovascular complication, fracture non-union, deep pelvic infection or postoperative thromboembolic phenomenon.
Discussion
Pelvic ring injuries have historically always been difficult to manage, often associated with visceral injuries that along with acute volume loss, prove to be life-threatening. In such cases, early intervention and treatment become imperative.
Matta et al.[7] conducted their study comparing three treatment techniques for unstable pelvic fractures–skeletal traction and/or pelvic sling, anterior frame external fixation and internal fixation–and concluded that internal fixation was superior to other modes of treatment in patient outcome.
Cole, Blum and Ansel et al.,[8] in their study on 64 patients, found percutaneous screw fixation to be a quick and safe method for fixation of pelvic fractures in the hands of an experienced surgeon. In the present study, an equal number of male and female patients were operated, with the majority of patients belonging to the age group 40 to 50 years, with the most common occupation among patients being construction workers. This is in contrast with studies conducted by Elzohairy et al.,[9] Lange and Hansen,[10] Zamzam,[11] all of which found male preponderance among patients with pelvic ring injuries, with road traffic accidents being the most frequent mode of injury. This may be explained by the fact the majority of patients presenting to our center came from neighboring rural areas, working at construction sites (both males and females). Also, due to the COVID pandemic-related restrictions during the study period, the incidence of road traffic accidents was reduced.
Po-Han Chen et al.[12] in their comparative study concluded that percutaneous screw fixation of pelvic ring injuries was superior in terms of patient outcome compared with conservative management. Among 15 patients operated in their study, the functional outcome distribution based on the Majeed functional classification among the operated group was: 8 excellent, 4 good, 2 fair, and 1 poor.
In the study conducted by Elzohairy et al.[9] on 20 patients of posterior pelvic ring fractures operated with percutaneous screw fixation, the final functional outcome was graded as excellent in 8, good in 9, and fair in 3 patients. The present study shows similar outcomes.
Among the working patients in this study, 6 (75%) were able to return to their place of work. This statistic has been variable in various studies conducted with different modes of fixation of pelvic fractures. Studies conducted by Holdsworth,[13] Tornetta,[14] and Miranda[15] found the proportion of their patients returning to their previous occupation to be 50%, 67%, and 80%, respectively.
Conclusion
Percutaneous fixation of pelvic ring fracture is a viable option for definitive fracture management in acute trauma setting with favorable functional outcome.
Intraoperative reduction of fractured ring by manual compression/traction or using bone clamps is a must before fixation to avoid future limb length discrepancy/fracture non-union. Partially threaded cc screws (6.5 mm) can also be used for this method instead of the conventionally used 7.3/7.5 mm cc screws.
Patients with hemodynamic instability or other osseous/extraosseous injuries, who may not be fit for fixation by conventional open methods, can also be managed with this method as it is minimally invasive and associated with nearly no blood loss.
Conflicts of interest
None declared.
References
- Biomechanical comparison of supraacetabular external fixation and anterior pelvic bridge plating. Proc Inst Mech Eng H. 2017;231:931-7.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of open book pelvic fractures: comparison between internal and external fixation. J Surg. 2021;9:145-8.
- [Google Scholar]
- Early results of percutaneous iliosacral screws placed with the patient in the supine position. J Orthop Trauma. 1995;9:207-14.
- [CrossRef] [PubMed] [Google Scholar]
- Acute pelvic fractures: I. Causation and classification. J Am Acad Orthop Surg. 1996;4:143-51.
- [CrossRef] [PubMed] [Google Scholar]
- Grading the outcome of pelvic fractures. J Bone Joint Surg Br. 1989;71:304-6.
- [CrossRef] [PubMed] [Google Scholar]
- Internal fixation of pelvic ring fractures. Clin Orthop Relat Res 1989:83-97.
- [PubMed] [Google Scholar]
- Outcome after fixation of unstable posterior pelvic ring injuries. Clin Orthop Relat Res 1996:160-79.
- [CrossRef] [PubMed] [Google Scholar]
- Open reduction internal fixation versus percutaneous iliosacral screw fixation for unstable posterior pelvic ring disruptions. Orthop Traumatol Surg Res. 2017;103:223-7.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvic ring disruptions with symphysis pubis diastasis. Indications, technique, and limitations of anterior internal fixation. Clin Orthop Relat Res 1985:130-7.
- [PubMed] [Google Scholar]
- Unstable pelvic ring injuries. Outcome and timing of surgical treatment by internal fixation. Saudi Med J. 2004;25:1670-4.
- [PubMed] [Google Scholar]
- Outcome analysis of unstable posterior ring injury of the pelvis: comparison between percutaneous iliosacral screw fixation and conservative treatment. Biomed J. 2013;36:289-94.
- [CrossRef] [PubMed] [Google Scholar]
- Dislocation and fracture-dislocation of the pelvis. J Bone Joint Surg Br. 1948;30B:461-6.
- [PubMed] [Google Scholar]
- Outcome of operatively treated unstable posterior pelvic ring disruptions. Clin Orthop Relat Res 1996:186-93.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvic ring injuries. A long term functional outcome study. Clin Orthop Relat Res 1996:152-9.
- [PubMed] [Google Scholar]







