Translate this page into:
Empty Nose Syndrome with Unilateral Ethmoidal Mucopyocoele – An Extremely Rare Presentation

*Corresponding author: Dr. Pradeepti Nayak, Department of ENT, School of Medical Sciences and Research, Sharda Hospital, Sharda University, Uttar Pradesh, India. pradeepti.nayak@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rizvi S, Kalra R, Pathak VK, Nayak P. Empty Nose Syndrome with Unilateral Ethmoidal Mucopyocoele – An Extremely Rare Presentation. Int J Recent Sur Med Sci. 2023;9:130-3. doi: 10.25259/IJRSMS-2021-5-7
Abstract
Introduction
Empty nose syndrome (ENS) is a poorly understood and rare iatrogenic disorder resulting from the destruction of normal nasal tissue. ENS is a recognized complication after turbinate excision. These patients suffer from endonasal crusting and dryness and a paradoxical sensation of nasal obstruction. These complications of ENS predispose these patients to recurrent sino-nasal infections.
Case report
Here we have reported the case of a 20-year-old female with right-sided nasal obstruction and headache. On diagnostic nasal endoscopy (DNE), the right nasal cavity was devoid of all anatomical landmarks. A hidden ethmoidal mucopyocoele was identified on radiological evaluation . This was drained surgically. Patient’s symptoms improved drastically postoperatively.
Conclusion
Despite the fact that occurrence of rhino-sinusitis is common in patients of ENS, a mucocoele or mucopyocoele has never been reported previously. To the best of our knowledge, this is the first ever reported case of ENS with ethmoidal mucopyocoele in a young, immuno-competent patient.
Keywords
Empty nose syndrome
ethmoidal mucopyocoele
inferior turbinate resection
secondary atrophic rhinitis
INTRODUCTION
The descriptive term “empty nose syndrome (ENS)” was coined in 1994 by Kern and Stenkvist to describe empty space in the region of the inferior and middle turbinates on coronal computed tomographic images of the patients.[1]
They observed that these patients suffered from endonasal crusting and dryness and that some of them also experienced a paradoxical sensation of nasal obstruction. ENS is a recognised complication, onset for months or years after inferior and medial turbinate surgery.[2]
It is distinguished from atrophic rhinitis (or ozena), a primitive pathology of sino-nasal structures of unknown origin, showing similar symptomatology, despite adequate intranasal airspace.[2,3]
The physiopathology of ENS still needs to be better understood, but several complementary hypotheses are found in the literature. It is thought to result from loss of nasal physiological functions (humidification, warming and cleansing of inhaled air) due to reduced mucosal area[4] inducing proportional loss of sensory, tactile and thermal receptors[5] essential for treating inhaled air.
Shiethauer[6] demonstrated that ENS was associated with decreased humidification, increased warming and reduced nasal airflow resistance.
These functional losses were estimated at around 23% following turbinectomy.[6,7]
These complications of ENS predispose these patients to recurrent nasal and sinus infections. Even though the occurrence of rhino-sinusitis is common in patients of ENS, a mucocoele or mucopyocoele has never been reported previously.
Here we have reported an unusual case of empty nose syndrome with right-sided ethmoidal mucocele in a young female with a history of undocumented nasal surgery during childhood.
CASE REPORT
A 20-year-old female presented to the ENT outpatient department of a tertiary healthcare center with complaints of right-sided nasal blockage and right-sided headache for one month. The right-sided nasal obstruction was insidious in onset and progressive, with an associated history of loss of sensation of smell. The accompanying right-sided nasal pain was gradual in onset, dull aching type, continuous, progressive, radiating to the right inner canthus and associated with a history of progressively worsening vision in the right eye. There was no associated diplopia. There was no history of nasal discharge, difficulty breathing or allergic symptoms. She did not have any history of fever or recent trauma. There was no history of any facial swelling. However, it was established that she underwent an undocumented nasal surgery when she was five years old, and no details were available.
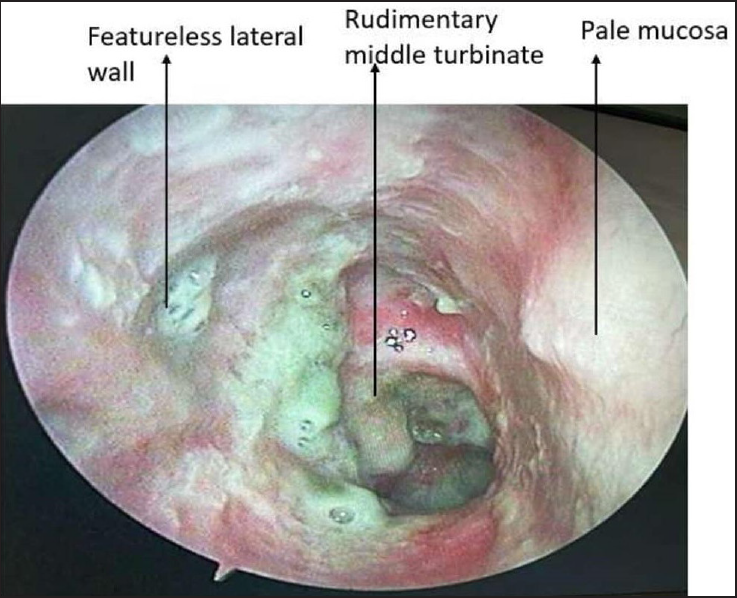
On examination, she was thin-built, well-hydrated, conscious and oriented to time, place and person. All her vitals were stable, and no obvious findings could be appreciated on systemic examination. On local examination, externally, the dorsum of the nose was found to be normal, and there were no malformations. Anterior Rhinoscopy revealed the septum to be in the midline. On examination of the right nasal cavity, however, we found that the lateral wall of the right nasal cavity was significantly featureless. The inferior turbinate was completely absent, and the middle turbinate was barely visible. The meatus, sinus ostia and other lateral wall structures were also noticeably absent. The mucosa of the right nasal cavity was found to be pale and dry. In contrast, the left nasal cavity was found to be entirely normal. The entire anatomy of the right nasal cavity was grossly distorted on diagnostic nasal endoscopy (DNE) [Figure 1]. No anatomical landmarks could be appreciated on the lateral wall on the right side. A rudimentary, barely appreciable middle turbinate was observed at the junction of the lateral wall and what was initially mistakenly thought to be the roof of the nasal cavity on anterior rhinoscopy. It was later discovered on DNE to be extensive adhesions between the significantly atrophied middle turbinate and the septum, probably mucosalized over the years. The cottle test was positive on the right side with no paranasal sinus (PNS) tenderness.
-
The left nasal cavity was found to be entirely normal. On diagnostic nasal endoscopy, the entire anatomy of the right nasal cavity was seen to be grossly distorted
An ophthalmological evaluation was done to assess the vision. The vision in the right eye was 6/36, whereas the left vision was normal.
Radiological imaging was done for further evaluation. CT-scan clarified our findings. It showed expansion of right ethmoidal air cells with underlying bony destruction and a significant breach in the lamina papyracea [Figure 2]. There was also a mild extension of soft tissue in the infraorbital region [Figure 3].
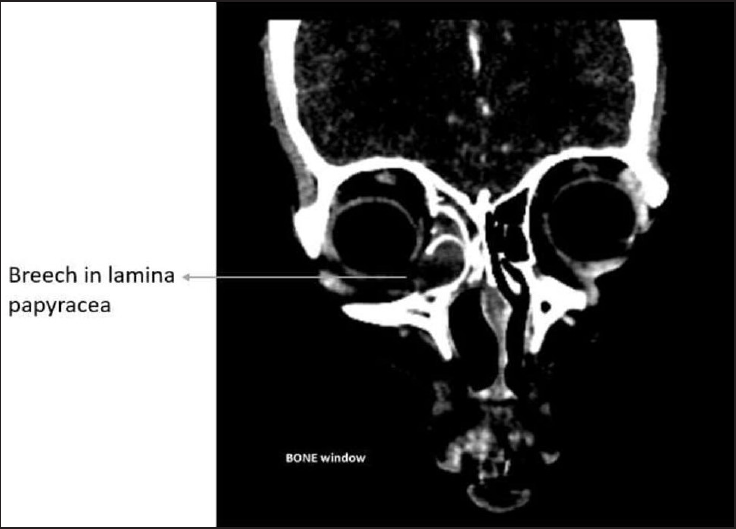
-
Radiological imaging was done for further evaluation. CT-scan clarified our findings. It showed expansion of right ethmoidal air cells with underlying bony destruction and a significant breech in the lamina papyracea
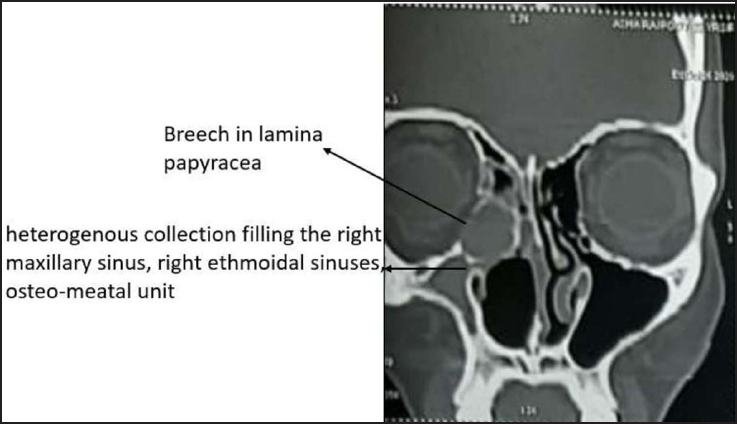
- There was mild extension of soft tissue in infraorbital region as well. There was hyperdense heterogeneous collection filling the right maxillary sinus, right ethmoidal sinuses, osteo-meatal unit and bilateral frontal sinuses
A hyperdense heterogeneous collection filled the right maxillary sinus, ethmoidal sinuses, osteomeatal unit and bilateral frontal sinuses [Figure 3]. The inferior turbinate was not visualized, and the middle turbinate on the right lateral wall was grossly underdeveloped, with extensive synechiae formation with the septum, forming a “false” roof, confirming our findings of DNE [Figure 4].
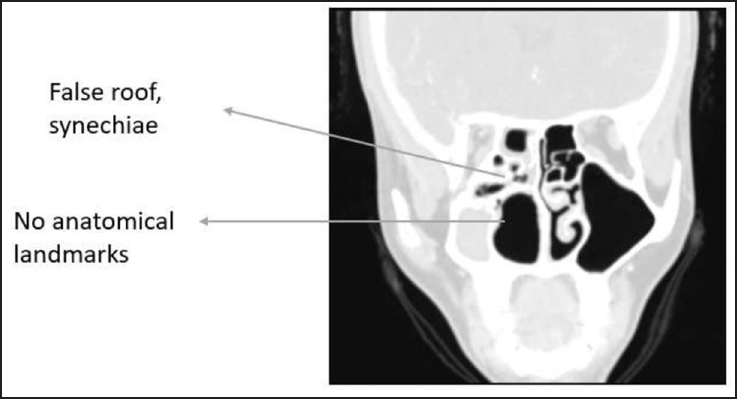
- Inferior turbinate was not visualized and the middle turbinate on the right lateral wall was grossly underdeveloped with extensive synechiae formation with the septum, forming a ‘false’ roof, confirming our findings of DNE
After diagnosis, the patient was taken up for endoscopic drainage under general anesthesia after appropriate pre-anesthetic clearance.
Despite lacking anatomical landmarks, the surgery was conducted by palpation, approximation and comparison with the left nasal cavity. The vestigial uncinate process was identified anterior to the middle turbinate remnant by palpation and excised after raising a mucosal flap. The maxillary antrum and ethmoidal cells were identified by guesstimate and drained of the purulent secretions. The sinuses were widened and cleared of all diseases. Betadine wash was given post-procedure. Haemostasis was achieved, and unilateral anterior nasal packing was done.
Postoperatively the patient’s symptoms were dramatically alleviated, and her vision returned to normal.
CONCLUSION
ENS is a poorly understood and rare iatrogenic disorder resulting from the destruction of normal nasal tissue. In severe forms like ours, it can be debilitating, and a lack of recognition and understanding of this disease process may be at great expense to the patient.
In our case, the early childhood trauma in the form of undocumented surgery may have completely derailed the development of facial morphology. This resulted in gross underdevelopment of the normal sino-nasal structures to the point that the ostia of the major sinuses were never formed. The severe obstruction caused to the drainage therein exacerbated a case of easily remediable rhinosinusitis to a case of destructive mucopyocoele with severe impending complications in a young, otherwise immunocompetent patient.
To our knowledge, this is the first-ever reported case of empty nose syndrome with ethmoidal muco-pyocoele.
Empty nose syndrome is an entity that should not be overlooked as it can severely affect patients whose only presenting complaint may be nasal obstruction. It is suspected that the nasal obstruction is initially disproportionate in its psycho-affective and social impact compared to the objective and clinical observations. Due to its uncommon entity, the diagnosis and management are yet to be streamlined. However, the best management remains preventive. The proper protocol needs to be followed for septal and turbinate surgeries, especially in the young, the key being “less is more”.
Acknowledgement
None.
Ethical Approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patients consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- The diagnosis and management of empty nose syndrome. Otolaryngol Clin North Am. 2009;42:311-30.
- [CrossRef] [PubMed] [Google Scholar]
- Empty nose syndrome: what are we really talking about? Otolaryngol Clin North Am. 2009;42:331-7.
- [CrossRef] [PubMed] [Google Scholar]
- Empty nose syndrome: limbic system activation observed by functional magnetic resonance imaging. Laryngoscope. 2011;121:2019-25.
- [CrossRef] [PubMed] [Google Scholar]
- The air-conditioning capacity of the human nose. Ann Biomed Eng. 2005;33:545-53.
- [CrossRef] [PubMed] [Google Scholar]
- Surgery of the turbinates and “empty nose” syndrome. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2010;9 Doc03
- [Google Scholar]
- Regional cerebral activation in irritable bowel syndrome and control subjects with painful and nonpainful rectal distention. Gastroenterology. 2000;118:842-8.
- [CrossRef] [PubMed] [Google Scholar]







