Translate this page into:
Focal Cortical Thickening along the Lateral Aspect of the Proximal Femoral Shaft: A Warning Radiographic Sign for Subsequent Complete Atypical Femoral Fracture in Patients on Bisphosphonates
Corresponding Author: Sachin Agrawal, Consultant, Department of Radiodiagnosis, National University Hospital, Singapore, Phone: +006590063238, e-mail: sachin_nandkishore_agrawal@nuhs.edu.sg
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
How to cite this article: Agrawal S, Santosa A. Focal Cortical Thickening along the Lateral Aspect of the Proximal Femoral Shaft: A Warning Radiographic Sign for Subsequent Complete Atypical Femoral Fracture in Patients on Bisphosphonates. Int J Recent Surg Med Sci 2017;3(1):58-60.
Abstract
Atypical femoral fracture is a known complication of patients receiving long-term bisphosphonates for osteoporosis. Recognizing early radiographic features is important to provide timely care and management before the development of a more debilitating complete fracture with its associated morbidity and mortality. We report a case of a 72-year-old lady on long-term treatment with alendronate, who presented initially with groin pain and subsequently with a femoral fracture, without any major trauma. The initial radiographic finding of focal thickening along the lateral cortex of the proximal femur was missed.
Keywords
Atypical femoral fracture
Bisphosphonates
Focal cortical thickening
INTRODUCTION
Bisphosphonates are widely used for the treatment of patients with osteoporosis. They reduce the incidence of vertebral and other fractures by suppressing the loss of bone volume.1 Contradictorily, however, long-term biphosphonate usage is itself sometimes associated with increased incidence of atypical fractures. These biphosphonate-related atypical fractures were first described in 2005 by Odvina et al.2 These fractures are insufficiency fractures with characteristic location and radiographic features.3 There are few reports in the radiology literature and many physicians including radiologists are not aware of this entity. Here, we report a patient with a biphosphonate-related fracture. The clinical presentation, characteristic radiographic features, further imaging work-up, and differential diagnosis and management strategies have been discussed with emphasis on early radiographic signs before the development of a complete fracture.
CASE REPORT
A 76-year-old woman was on long-term treatment with alendronate for osteoporosis. She presented to the outpatient with a 1-week history of groin pain. Premorbidly, she was ambulant with a walking stick. Since 1 week, pain has affected her mobility and she has become unsteady with the walking stick. A radiograph (Fig. 1) was performed which was read as normal by the reporting radiologist and the patient was discharged.

- Frontal radiograph of the right hip joint (on initial presentation) was read as showing no fracture or dislocation
A few hours later on the same day, the patient presented again with markedly increased pain after she tripped and fell in the kitchen. She was unable to bear her weight and walk after the incident. A repeated radiograph showed a complete and displaced transverse fracture through the proximal shaft of the femur (Fig. 2). No underlying pathological lesion was identified. A diagnosis of insufficiency fracture was made based on the transverse orientation of the fracture and absence of an underlying pathological lesion. The patient was managed with internal fixation of the fracture.

- Frontal radiograph of the right hip joint on follow-up demonstrates a displaced and complete transverse fracture through the proximal shaft of the femur (note the presence of a medial spike)
A retrospective review of the earlier radiograph revealed presence of focal cortical thickening along the lateral cortex of the proximal femur (Fig. 3), the site of later development of a complete fracture.
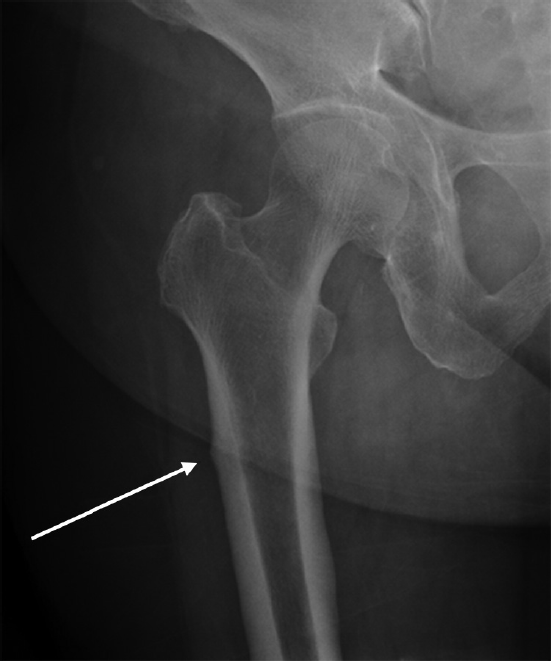
- A retrospective review of the frontal radiograph of the right hip joint (at initial presentation) showed the presence of focal cortical thickening along the lateral cortex of the proximal femur, the site of later development of a complete fracture
DISCUSSION
Atypical femoral fracture (AFF) is an insufficiency fracture that occurs as a result of normal activity or low-energy trauma in bones that are weakened by a generalized process, such as osteoporosis. Insufficiency fractures of the proximal femoral shaft are quite rare in the osteoporotic population.4 Several studies have identified a strong relationship between long-term receipt of bisphosphonates and atypical fractures in the proximal femoral shaft.5 It is rather a paradox that a fracture would be associated with biphosphonate therapy, as they are prescribed to reduce the incidence of osteoporosis-related fractures. The exact mechanism for biphosphonate-related insufficiency femoral fracture is not entirely understood, although it has been suggested that suppression of bone turnover could cause microdamage accumulation that allows small cracks to progress.6
The American Society for Bone and Mineral Research (ASBMR) task force has summarized the published reports on AFFs and defined the features of these fractures.7 In 2013, the case definition was revised by the ASBMR to highlight radiographic features that distinguish AFFs from ordinary osteoporotic femoral diaphyseal fractures (Table 1).8 Localized periosteal reaction or endosteal thickening of the lateral cortex was included in the revised case definition for the first time. This focal thickening of the lateral femoral cortex was present in our patient in the earlier radiograph, although was missed.
|
To satisfy the case definition of AFF, the fracture must be located along the femoral diaphysis from just distal to the lesser trochanter to just proximal to the supracondylar flare. In addition, at least four of five major features must be present. None of the minor features is required but have sometimes been associated with these fractures. Major features a
Minor features
|
aExcludes fractures of the femoral neck, intertrochanteric fractures with spiral subtrochanteric extension, periprosthetic fractures, and pathological fractures associated with primary or metastatic bone tumors and miscellaneous bone diseases (e.g., Paget's disease, fibrous dysplasia)
As per the ASBMR task force's recommendations, an AFF usually begins as a small focal beak-like cortical thickening of the lateral cortex which is usually the result of focal periosteal/endosteal thickening related to a microfracture. Subsequently, there may be an appearance of a small incomplete lucent fracture line in the region of the periosteal thickening which may later progress to a complete fracture involving both the lateral and the medial cortex.8 In the early stage, patients can present with groin or thigh pain which can be misdiagnosed to degenerative disease of the lumbar spine and sacroiliac joints. This prodromal thigh or groin pain was observed in approximately 70% of patients.1 The contralateral femur may be involved in approximately 20 to 64% of cases.5
Thus, if a patient on biphosphonate therapy presents with groin pain, one should have a high index of suspicion for a possible AFF, and a radiograph should be done. Also, if a radiologist encounters a radiograph of a patient with groin or thigh pain, he or she should look for signs of focal cortical thickening and sought the clinical history of biphosphonate therapy. Focal cortical thickening should be further evaluated with magnetic resonance imaging or a bone scan.4 The bone scan would demonstrate a focus of increased uptake in the lateral cortex of the proximal femur. Magnetic resonance imaging scan would reveal focal thickening of the lateral cortex with a focus marrow edema with or without the presence of an incomplete fracture line. These findings are suggestive of a micro-fracture and associated stress response. Management strategies include limited weight-bearing through the use of crutches or a walker when there is focal cortical thickening, and prophylactic intramedullary nail fixation if a small incomplete fracture line is seen.8
Fractures in the proximal femoral diaphysis seen in the setting of low-energy trauma can occur in other clinical situations. These include stress fractures in young military recruits and athletes, pseudofractures of osteomalacia, and pathologic fractures. These fractures can be differentiated based on their clinical presentation and imaging features. Both the stress fractures, as well as the pseudofractures of osteomalacia, involve the medial cortex, as opposed to the biphosphonate-related AFFs which involve the lateral cortex. Pathologic fractures usually demonstrate features of underlying disease like metastases and Paget's disease.5
CONCLUSION
Focal cortical thickening of the lateral cortex of the femoral shaft serves as a warning sign for the subsequent development of a complete AFF in patients on long-term biphosphonate therapy. Awareness and recognition of this early radiographic sign, especially in patients presenting with groin or thigh pain, allows for the institution of appropriate early intervention before the development of a debilitating complication.
Source of support:
Nil
Conflict of interest:
None.
REFERENCES
- Atypical femoral fractures and bisphosphonate use: current evidence and clinical implications. Ther Adv Chronic Dis. 2015;6(4):185-193.
- [CrossRef] [PubMed] [Google Scholar]
- Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab. 2005;90(3):1294-1301.
- [CrossRef] [PubMed] [Google Scholar]
- Management of atypical femoral fracture: a scoping review and comprehensive algorithm. BMC Musculoskelet Disord. 2016;17:227.
- [CrossRef] [PubMed] [Google Scholar]
- Subtrochanteric femoral insufficiency fracture following bisphosphonate therapy for osseous metastases. Radiol Case Rep. 2015;3(4):232.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of proximal femoral insufficiency fractures in patients receiving bisphosphonate therapy. AJR Am J Roentgenol. 2010;194(4):1061-1064.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical femoral fractures: epidemiology, etiology, and patient management. Curr Opin Support Palliat Care. 2012;6(3):348-354.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2010;25(11):2267-2294.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014;29(1):1-23.
- [CrossRef] [PubMed] [Google Scholar]







