Translate this page into:
Tibial Malrotation after Intramedullary Locked Tibia Nailing and its Computed Tomography-Based Assessment

*Corresponding author: Dr. Sucheta Mahant, MDS Paedodontics and Preventive Dentistry, Department of Dentistry Dr Radhakrishnan Government Medical College Hamirpur, Himachal Pradesh, India. sansucheta.thakur142@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rathore LP, Thakur SK, Thakur A, Mahant S. Tibial malrotation after intramedullary locked tibia nailing and its Computed Tomography-based assessment. Int J Recent Surg Med Sci. 2024;10:7-11. doi: 10.25259/IJRSMS-2022-10-9
Abstract
Objectives
To assess the incidence and degree of malrotation of tibia after fixation with intramedullary nail for tibial shaft fractures and its measurement by computed tomography (CT). The study also aims to assess the value of CT-based torsion angle in such cases.
Material and Methods
In this prospective study, fifty patients with closed/open fracture of tibia shaft (proximal 1/3, middle 1/3 or distal 1/3) with or without fracture of fibula were chosen and operated with closed/open reduction internal fixation with reamed intramedullary locked nail. Torsion angle calculated by post-operative CT and revision done for selected cases when tibial malrotation was more than 10 degrees than the control (normal side).
Results
The range of malreduction was from 43 degrees of external rotation to 12 degrees internal rotation. 15 of the 50 (30%) tibia operated showed malrotation and 5 (10%) were above 20 degrees. The repetition of torsion angle showed a variation of 3.2 to 4.3 degrees. Some injury patterns showed more malrotation than the others.
Conclusion
Assessment of tibial malrotation following intramedullary nailing has shown higher incidence of malalignment than previously reported in the literature. CT-based torsion angle calculation can be used as a reliable indicator of malrotation.
Keywords
Computed Tomography
Interlocking nail
Malrotation
Tibial Fracture
INTRODUCTION
Fracture of the tibial diaphysis is the most common injury of all the long bones with a male preponderance of approximately three times.[1,2] Bony union along with good functional range of motion with acceptable alignment is the goal of treatment.[3] Many studies in the past have conclusively shown that closed tibial shaft fractures do well with intramedullary nailing as compared to conservative treatment or open reduction internal fixation in terms of better functional outcomes and lower complication rate.[4] Intramedullary reamed interlocked tibia nailing is a common procedure so much so that it is probably the first major procedure that an orthopaedic surgeon learns to perform independently. Closed reduction internal fixation with image intensifier or otherwise is an indirect method of reduction and whereas it can be challenging, it is not free of complications as well, such as malalignment, the topic under discussion.[5] Tibial torsion is the physiologic rotation of the proximal versus the distal articular axis of the tibia in the horizontalplane.[6] One of the first definitions put forward by Le Damany was based on a cadaver study, which was a mechanical one. Since then, many radiological methods have been suggested for the same and because they all use different reference points for measurement, many methods are not directly comparable.[7]
Malrotation of tibia subsequent to interlocked nailing of tibia is uncommonly specifically discussed and previous literature mainly has focussed on the calculation of rotational malalignment by roentgenograms or by clinical means.[7] Consequently, there appears to be a paucity of literature in the topic of incidence and severity grading of rotational malalignment of tibia after nailing.[4] The incidence of malunions with the interlocked technique has ranged from 0% to 13%.[6] Tibial malrotation has been estimated to range between 0 and 6% in some studies, most of which have done clinical estimation.[8–10] However, there is much variation in the clinical or mechanical assessment methods used in the past. Later, some studies posted results using CT as a guide for the measurement of tibial torsion and have reported good repeatability and reliability.[4] This study was aimed at assessing the incidence and degree of malrotation of tibia after fixation with intramedullary nail for tibial shaft fractures and its measurement by CT. This study shall also focus on the value of CT for assessing the same whilst discussing and comparing with the literature on the topic.
MATERIAL AND METHODS
This study included 50 consecutive patients with closed fracture of both bones of the leg with fracture level in the proximal, middle or distal third of the tibia. Closed fractures and Gustilo-Anderson grade1 open fractures were included in the study to keep other cofactors to a minimum. Patients with ipsilateral or contralateral lower limb injury, Gustilo-Anderson grade 2 and 3 open fractures, polytrauma, intraarticular fractures and pathological fractures were excluded. The study was done over a period of 9 months in a district hospital setup. All the surgeries were done under spinal anaesthesia in a supine position within 5 days of the injury. Position of leg was hanging from the side of the table over a side post with the knee flexed and fracture being manually reduced by the assistant. After midline skin incision over the patellar tendon, entry point was chosen according to fracture site and medullary canal was serially reamed over a guide wire while it was kept reduced manually by traction. After insertion of the intramedullary nail, it was locked distally and proximally with bolts that varied both in the number of screws and the direction of screws. There was further a variation as to which, proximal or distal, locking was done first. Proximal screws were medial to lateral and distal screws had two options, one screw in the anteroposterior (AP) direction and two in the mediolateral direction, just like in a standard nail.
Post-surgery, all 50 patients underwent plain CT-Scan of bilateral legs with knees and ankle in a supine position with both the legs strapped together. Focus was given to axial cuts, which were taken both at the knee joint and distally at and above the ankle joint. A method similar to previous studies was used to assess torsion of the tibia using the CT-Scan.[4–6] The first reference line was chosen to be as a tangent to the posterior tibial cortex at the level immediately superior to the head of the fibula. The second reference line was taken just above the crural surface of distal tibia and was made perpendicular to the tibiofibular joint at that level [Figure 1]. The angle between the two lines was labelled as the torsion angle [Figure 2] and was compared from the normal side as control. The definition of malrotation was decided to be a difference of more than 10 degrees from the normal side in either direction, that is, in external and internal rotation of tibia distal to the fracture site after fixation.

- Two Reference lines drawn in proximal and distal tibia.
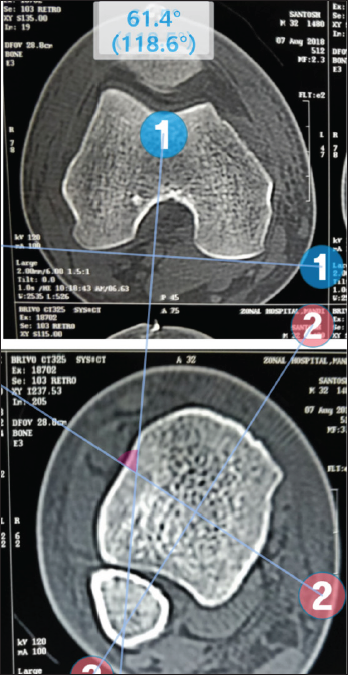
- The angle between the two lines was labelled as torsion angle.
RESULTS
The average age was 35.1±9.14 years, ranging from 18 to 58 years. Mode of injury was roadside accident in 5 cases and fall from height in 45 cases. There were 42 males and 8 females in the study. Left-sided fractures were more than right-sided fractures (31 left and 19 right). Using the Arbeitsgemeinschaft für Osteosynthesefragen (AO) classification, there were 24 AO type A, 17 type B and 9 type C fractures. Fibula fracture was seen in association with tibia fracture in all cases and was fixed in only four cases, all of which had distal 1/3rd tibia fractures. The difference in torsion was calculated using the normal side as control and the torsion found on CT-scan using the method described was calculated and subtracted from the normal to give the torsional difference. The mean value came out to be 7.41 ± 4.54 degrees with a range from 26 degrees to 2 degrees external rotation. Malrotation of more than 10 degrees was found in 15 patients (30%), more than 15 degrees in 7 (14%) and above 20 degrees in 3 (6%) patients [Table 1]. The results were assessed using the SF-36 and Short Musculoskeletal Functional Assessment functional questionnaires and were found to be excellent in 20 (40%), good in 17 (34%), fair in 9 (18%) and poor in 4(8%). Thus, fair to excellent results were noted in 92% of the patients. As per our study, more percentage of patients with fractures of the distal tibia showed malrotation of more than 10 degrees, and this correlation was not found to be significant (p-value < 0.05). Similarly, there was more incidence of malrotation in open fractures and in cases where fibula was not fixed, but the correlation was non-significant (p-value > 0.05). Equal percentage of malrotation was noted with AO type A and C fractures with non-significant correlation.
| Malrotation < 10 degrees | Malrotation >10 degrees | Percentage of malrotation >10 degrees (%) | |
|---|---|---|---|
| Fracture site | |||
| Proximal 1/3rd | 5 | 2 | 28.5 |
| Middle 1/3rd | 22 | 8 | 26.2 |
| Distal 1/3rd | 8 | 5 | 10 |
| Fracture type | |||
| Open (grade 1) | 18 | 8 | 33 |
| Closed | 17 | 7 | 29 |
| Fracture fibula | |||
| Fixed | 4 | 0 | - |
| Not fixed | 31 | 15 | 33 |
| AO/OTA | |||
| A | 16 | 8 | 33 |
| B | 13 | 4 | 24 |
| C | 6 | 3 | 33 |
DISCUSSION
Our study has shown that there is considerable incidence of tibial malrotation than has been previously believed. Although some previous studies have focussed on the same problem, the actual incidence and its grading still remains underestimated. Also, there has been no final consensus on the definition and threshold of acceptable tibial torsion in the past but 10 degrees[4] has been generally taken as the upper limit, whilst some have used 8 degrees.[11] The first definition widely accepted was the one given by Mikulicz and Le Damany, which used the proximal and distal articular axis as the reference.[12]
Although there is no convincing evidence about what amount of malalignment will cause functional impairment, the acceptable deformity in a fractured tibia has been classically mentioned as a shortening of less than 1 cm, 5 degrees of valgus, 10 degrees in the anteroposterior plane and 10 degrees of external rotation. No degree of varus or internal rotation deformity is taken to be acceptable.[13] However, in some studies, there has been research on the effects of malalignment on the biomechanics of the lower limb, which is found to have deleterious effects. Among these, rotational malalignment has been studied and results are convincing. Turner et al.[14] demonstrated methodically the increase in the patellofemoral instability and Osgood-Schlatter disease. It has also been strongly linked to osteoarthrosis of the knee and ankle as it has been shown to influence the biomechanics of the same.[15] Turner, in an independent study, found that panarticular arthritis of the knee was seen more in patients with tibial torsions away from the average value.[16] Apart from these, various other conditions have been linked to altered tibial torsion like longitudinal and horizontal tears of the menisci, meniscal cysts, chondromalacia patella, traction apophysitis of tibial tubercle, osteochondritis dissecans and fat pad entrapment.[11,14,16–19]
The identification of malrotation of tibia intraoperatively can be tricky and many a time goes unnoticed that leads to the undervaluation of the problem. Initially reported clinically by Velazco et al.,[20] Court-Brown et al.,[21] Puno et al.[22] and Krettek et al.,[23] the measurement of tibial torsion has been also quantified using x-rays by Hutter and Scott.[24] A method has been described for the intraoperative calculation of the same by comparing rotational alignment of the knee with that of ankle in a true anteroposterior view by Clementz and Magnusson,[25] but there are no reports supporting its widespread use. The first measurement of torsion of tibia using computed tomography was done in 1980 by Jakob et al.[12] and later in 1981 by Jend et al.[11] However, both did not conclusively describe the repeatability of the same. The same was later on questioned by a study by Laasonen et al.[26] in 1984. Over the years, there have been many studies in the area and most have reported improved repeatability using the reference lines as in our study so much so that it is now considered the gold standard in quantifying the malrotation of the tibia with considerable accuracy.[4,11,12,27]
The same kind of studies done previously have reported similar findings. In a series of 22 cases by Puloski et al.,[4] there was a 23% incidence of malrotation after Intramedullary (IM) nailing, which was seen in distal third tibia fractures in the 4 out of 5 malrotated cases. This is in direct agreement with findings in our study where we have found a significant correlation between these two variables. This finding has not been highlighted in the past. Also, a common finding reported was the external tibial torsion to be more common than internal. Prasad et al.[28] in 1999 have reported similar findings with 36% incidence, while Jend et al.[11] documented a 14% incidence, which are comparable to 32% incidence in our study. The malrotation was found more in AO/Orthopaedic Trauma Association (OTA) type A and C fractures similar to the study by Puloski et al.[4] There has also been a higher incidence of malrotation in cases where fracture of the fibula was not fixed; however, this finding cannot be definitively linked to malrotation as a causative factor since it requires further scrutiny and also the correlation was found to be statistically non-significant. Note was also made of increased incidence of malrotation in open fractures, the correlation of which was found to be insignificant. However, it can be attributed due to more soft tissue trauma leading to lesser support to the fracture and allowing malrotation.
Whilst on the topic, the authors would like to discuss the locking method practiced in the institute and many hospitals in the state, which might have some impact on the reported findings. Generally, after nail insertion, distal locking is done prior to proximal locking usually to have an option of back hammering to impact the fracture ends. The common position for distal locking is a figure of four position (Flexion Abduction External Rotation (FABER) at hip, flexion at knee) with the distal tibia kept on a radiolucent table and in order to have a round image of the holes in the nail, the knee is pressed down by the assistant and the distal tibia is elevated by keeping a folded sheet beneath it so as to keep the leg parallel to the ground in order to have the desired image. In the process, the foot maybe inadvertently rotated externally either by the assistant or by the surgeon himself in an innocent attempt for locking to take place easily. Also, the fact that the folded towel is below the distal leg only and the foot is a little off the table allows for this phenomenon to take place accidentally. In a case where soft tissue trauma is severe and there is internal degloving, this may happen on its own accord due to gravity. However, these variables were not taken into account when this study was started, but assuming they have some role in the problem under discussion, the authors would like to suggest a few solutions for the same purely on the basis of experience. It may be suggested that the surgeon may lock the proximal holes first and remove the zig. Then, lock the anteroposterior distal hole after clinically assessing for malrotation as the limb can be straightened out after zig removal and then go for mediolateral locking bolts.
Our study has reported similar findings as have the few studies done on the topic concerned. The sample size in the study was acceptable as per the authors; however, it lacked a long follow-up and biomechanical correlation of the malreduction on the lower limb. Some of the probable causative factors that came up during the study could not be taken into the statistics.
CONCLUSION
As discussed, the incidence of malrotation after tibia nailing is both under-evaluated and under-estimated. Although, CT is costly and ionising, it is the investigation of choice for assessment of the same. Relying on clinical assessment can be misleading as shown by Jend et al.[11] who reported that only about 25% of maltorsions were clinically evident. Since malrotation has a degrading effect on the biomechanics of the knee and the lower limb as a whole, missing occult malrotation can lead to suboptimal treatment of fractures of the tibia. In order to prevent an undesirable functional outcome, it is pertinent that we evaluate the rotational component of reduction closely.
Ethical approval
The research was in compliance with Helsinki declaration 1964.
Declaration of patients consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There is no conflict of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Fractures of the Tibia and fibula. In: Bucholz R, ed. Heckman J, ed. Court-Brown C, ed. Tornetta P, ed. McQueen M, ed. Ricci W, ed. editors Rockwood and Green’s Fractures in Adults (6th ed). Philadelphia: PA: Lippincott Williams and Wilkins; 2005. p. :2079-146.
- [Google Scholar]
- The epidemiology of tibial fractures. J Bone Joint Surg Br. 1995;77:417-21.
- [PubMed] [Google Scholar]
- Tibial shaft fractures - management and treatment options. A review of the current literature. Acta Chir Orthop Traumatol Cech. 2012;79:499-505.
- [PubMed] [Google Scholar]
- Rotational malalignment of the tibia following reamed intramedullary nail fixation. J Orthop Trauma. 2004;18:397-402.
- [CrossRef] [PubMed] [Google Scholar]
- Lower limb malrotation following MIPO technique of distal femoral and proximal tibial fractures. Injury. 2011;42:194-9.
- [CrossRef] [PubMed] [Google Scholar]
- Malrotation after locked intramedullary tibial nailing: Three case reports and review of the literature. J Trauma. 2002;53:549-52.
- [CrossRef] [PubMed] [Google Scholar]
- Unstable fractures of the tibia treated with a reamed intramedullary interlocking nail. Clin Orthop Relat Res. 1995;315:56-63.
- [PubMed] [Google Scholar]
- Interlocking nailing for fractures of the femur and tibia. Injury. 1992;23:381-6.
- [CrossRef] [PubMed] [Google Scholar]
- Malunion after intramedullary nailing of tibial shaft fractures. Ann Chir Gynaecol. 1997;86:56-64.
- [PubMed] [Google Scholar]
- Measurement of tibial torsion by computer tomography. Acta Radiol Diagnosis. 1981;22:271-6.
- [CrossRef] [PubMed] [Google Scholar]
- Tibial torsion calculated by computerised tomography and compared to other methods of measurement. J Bone Joint Surg Br. 1980;62:238-42.
- [CrossRef] [PubMed] [Google Scholar]
- Tibia and Fibula Fractures. Rockwood and Green’s fractures in adults (Seventh ed). Philadelphia: Lipincott Williams & Wilkins; 2010. p. :1878.
- The effect of tibial torsion on the pathology of the knee. J Bone Joint Surg. 1981;63B:396.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of limb malrotation on malalignment and osteoarthritis. Orthop Clin North Am. 1994;25:405-14.
- [PubMed] [Google Scholar]
- The Association Between Tibial Torsion and Knee Joint Pathology. Clin Orthop Relat Res. 1994;302:47-51.
- [PubMed] [Google Scholar]
- The biomechanical basis of osteoarthrosis of the knee in total knee replacement. In: London: The Medical Engineering Working Party in collaboration with the Tribiology Group of the Institute of Mechanical Engineering and the British Orthopaedic Association. 1974. p. :8.
- [Google Scholar]
- Rotational alignment of the lower limb in osteoarthritis of the knee. Int Orthop. 1985;9:209-16.
- [CrossRef] [PubMed] [Google Scholar]
- Tibial torsion in patients with medial type osteoarthritic knee. Clin Orthop Relat Res. 1986;213:177-82.
- [PubMed] [Google Scholar]
- Open fractures of the tibia treated by the Hoffmann external fixator. Clin Orthop Relat Res. 1983;180:125-32.
- [PubMed] [Google Scholar]
- Closed intramedullary tibial nailing. Its use in closed and type I open fractures. J Bone Joint Surg Br. 1990;72:605-11.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term effects of tibial angular malunion on the knee and ankle joints. J Orthop Trauma. 1991;5:247-54.
- [CrossRef] [PubMed] [Google Scholar]
- Nonreamed interlocking nailing of closed tibial fractures with severe soft tissue injury. Clin Orthop Relat Res. 1995;315:34-47.
- [PubMed] [Google Scholar]
- Fluoroscopic measurement of tibial torsion in adults. A comparison of three methods. Arch Orthop Trauma Surg. 1989;108:150-3.
- [CrossRef] [PubMed] [Google Scholar]
- Tibial torsion measured by computed tomography. Acta Radiol Diagn (Stockh). 1984;25:325-9.
- [CrossRef] [PubMed] [Google Scholar]
- Determination of tibial torsion by computed tomography. J Foot Ankle Surg. 1994;33:144-7.
- [PubMed] [Google Scholar]
- CT assessment of torsion following locked intramedullary nailing of tibial fractures. Injury Int J Care Injured. 1999;30:467-70.
- [CrossRef] [PubMed] [Google Scholar]







